 |
 |
- Search
| Asian Spine J > Volume 13(2); 2019 > Article |
|
Abstract
Purpose
To validate the Persian version of the Million Visual Analogue Scale Questionnaire (MVAS), a self-administered low back pain (LBP) questionnaire.
Overview of Literature
The majority of LBP questionnaires translated into Persian evaluate the impact of LBP on daily living. The MVAS is one of the most commonly used self-administered LBP questionnaires, and was developed to assess a different direction and effect of activities of daily living on LBP intensity.
Methods
The questionnaire was translated into Persian with the forward-backward method and was administered to 150 patients randomly sampled from an occupational medicine clinic in Tehran in 2017.
Results
Cronbach’s alpha for all subscales ranged between 0.670 and 0.799. Confirmatory factor analysis showed adequate construct validity of the Persian version of the MVAS, with root mean square error of approximation 0.046, goodness of fit index 0.902, and comparative fit index 0.969. Other indexes were satisfactory.
Low back pain (LBP) is one of the most common causes of patient visits to general physicians [1]. This complaint is not well approached and diagnosed in a great number of cases, resulting in inaccurate management [2]. In most cases, the pain resolves on its own in <4 weeks; however, some patients experience pain again later in life [3]. Although LBP is generally considered as a self-limiting complaint, it causes enormous expense, resulting from unnecessary diagnostic tests, inappropriate therapy, and long-term absence from work [4,5].
An essential part of a good clinical management is a thorough and systematic evaluation of the complaint. For this, the physician should rely on both subjective and objective data. The objective data are mandatory because the physician assesses the progress and response to treatment using parameters such as range of motion and tenderness [6]. However, subjective information plays an equally important role. No one is more aware of the pain and its associated factors than the patient himself. Standard questionnaires assessing the patient’s perception of their condition are useful in these situations [7], as they give the doctor and patient data which can be transformed into standard quantified variables. These data can then be shared worldwide with other clinicians and researchers [8].
The Million Visual Analogue Scale Questionnaire (MVAS) is a 15-item self-administered questionnaire [9], aimed to measure the impact of LBP on an individual’s different aspects of life. It is considered to be one the most useful instruments for assessing LBP in recent years owing to the ease of administration and the short time required for completing and scoring this questionnaire [10]. MVAS uses the Visual Analog Scale (VAS) and assesses the essential domains of daily living in its assessment. Therefore, we aimed to validate the Persian version of this questionnaire for clinicians and researchers with Persian patients, as a standard international instrument.
This was a descriptive cross-sectional study with random stratified sampling. The study was conducted in Tehran, Iran between June and September 2017, and comprised 150 Patients with LBP visiting the occupational medicine clinic of Baharloo Hospital. Baharloo Hospital is an educational referral center and is well known for its high quality occupational medicine clinic.
According to statistical guidelines, to validate a questionnaire, the number of participants should be 5–10 times greater than the number of questions, and >150 participants would not make any notable difference in the accuracy of results [11]. Therefore, 150 questionnaires were administered and collected. We used IBM SPSS Software ver. 21.0 (IBM Corp., Armonk, NY, USA) and AMOS ver. 18.0 (SPSS Inc., Chicago, IL, USA) for statistical analysis of our data. The two major domains of our analysis were descriptive and analytic statistics. We represented numerical data as mean±standard deviation, and categorical variables data as a number and percentage. We used confirmatory factor analysis (CFA) and intra-class correlation (ICC) for the statistical analysis. All p-values below 0.05 indicated a statistically significant difference.
The MVAS questionnaire evaluates the effect and intensity of LBP, and subsequent disability across different domains. The three main domains examined are physical function, social life, and daily activities, through questions simply asking patients about their pain in standard situations like standing, walking, and sleep. A VAS is available to help the participants answer each question, which comprises a 100-mm line with the numbers 0 and 100 on the extremes, and labels such as ‘none at all’ or ‘intolerable’ indicating the numbers and the direction as the condition intensifies. Participants place a mark on the VAS line based on their pain intensity in that specific situation. The score for each question is then calculated by measuring the distance from the beginning of the line to the marked point in millimeters. The total score is the sum of the scores of all the questions.
Patients with LBP who were being treated in the occupational medicine clinic were included. The inclusion criteria were as follows: (1) age ≥18 years; (2) able to read Persian; (3) chronic LBP for minimum 6 weeks; (4) currently working; and (5) completed written informed consent. The main exclusion criterion was a positive surgical history of the lumbar spine or a previously diagnosed rheumatologic disorder affecting the lower back.
The MVAS was translated by four independent translators, including clinicians and professional translators from English to Persian and then back translated to English. The original and the back-translated versions were then compared with each other, and the noticeable differences were discussed and implemented, resulting in a pre-final version of the Persian MVAS.
These Pre-Final versions of the Persian MVAS were then administered by almost 20 patients suffering from LBP with different socioeconomic and educational levels. We ensured that the perception of the patient of each question is as we intended, and that the questionnaires are easy to understand. After this step, the final version of the questionnaire was framed.
Content validity indicates the overlap of the performance of the instrument with the ability to function as intended. To measure content validity, we arranged a ‘Content Evaluation Panel,’ which consists of those familiar with the study and its aim [12,13]. Each member of the panel evaluated the questionnaires and judged the role of each item corresponding to three available options: ‘essential,’ ‘useful but not essential,’ and ‘not necessary.’ Items which were considered ‘essential’ by more than half of the panel were considered to have content validity. Content validity is considered greater when more items are considered as ‘essential.’
To determine how essential an item would be, a content validity ratio (CVR) was assigned as an indicator. The CVRs were parameters based on which our final decision of the included items in the final format was made. Next, we calculated the mean values of CVR of the final items, also known as the content validity index (CVI). The developing instrument would only be considered valid when the CVR and CVI are greater than 0.7.
We performed the CFA to assess the construct validity of our instrument. Analyses included fit indices of chi-square statistic, goodness of fit index (GFI >0.9), the root mean square error of approximation (RMSEA <0.05), and comparative fit index (CFI >0.9) [14].
The study was conducted with the approval of Baqiyatallah University of Medical Sciences Institutional Review Board (IRB approval no., IR.BMSU.1395.378). Each participant gave written informed consent before enrolling in the study, and could withdraw from the study any moment they pleased.
In total, 150 participants enrolled in the study (122 males and 28 females). Respondents were aged 46±9.8 years. Completion of each questionnaire took approximately 5 minutes and the scoring was completed in <3 minutes. To assess the factorial structure of the MVAS questionnaire, the CFA was also conducted (Fig. 1) and the results are summarized in Table 1. We used the hypothesized model and compared it with the covariance matrix based on our empirical data. According to our findings, the CFA indicated excellent goodness of fit results. The standard beta CFA and reliability indexes are reported in Table 2. Reliability values were acceptable for all the domains assessed in MVAS. The ICCs for all domains of MVAS were in the range of excellent reliability. The number of patients who achieved minimum or maximum scores in the test was not greater than the 15% threshold, therefore there was no need to consider the ceiling and floor effect. For content validity, the committee of researchers assigned to evaluate the questions considered almost all of the questions essential with CVI and CVR values greater than 0.78.
To confirm the Persian version of MVAS as a robust instrument, we evaluated the two major domains of validity and reliability. Validity was divided into three subgroups, including translation validity, construct validity, and content validity. We used the forward-backward translation method in accordance with specific guidelines [15]. The pre-final version of the questionnaire was derived through comparison of the translated and original version. Next, after administering a small pilot study, the final version was agreed upon. There were some minor changes in the content of the questions due to the linguistic properties of the Persian language, but the intention of questions and the overall structure were preserved. In questions 7 and 15, we added “Because of your LBP…” to the questions for clarity. There was no need for alterations owing to cultural differences. A hundred millimeter line was placed as an answering medium for each question. Both ends of these lines were marked with dots, the numbers ‘0’ and ‘100,’ with expressions added to clarify of the process of answering. We provided a brief guide at the beginning of the questionnaire to ensure that all patients could completely understand how to complete the questionnaire. To make the questions look more distinct and much easier to answer, the background color of questions was changed from white to grey, and alternated between questions. Our results indicated that almost all participants understood and answered the questions without difficulty. The questionnaires were completed in an average time of 5 minutes and scored in about 2 minutes, similar to that observed in the original version [9].
Construct validity was measured using the CFA, resulting in excellent chi-square, GFI, RMSEA, and CFI parameters listed in Table 1. The CFA indicates an excellent fitness of results for the Persian MVAS.
The reliability of our instrument was evaluated by measuring the ICC and Cronbach’s alpha. The ICC values, indicating the homogeneity of the questionnaire, as shown in Table 2, were all greater than 0.7. Our study also showed excellent scores of Cronbach’s alpha ranging from 0.670 to 0.799. The ICC values plus the Cronbach’s alpha measurements both are indicators of the excellent reliability of the Persian MVAS.
Musculoskeletal problems such as LBP can become chronic and influence physical activities. This chronic pain has an undeniable socioeconomic consequence in the patient’s life and the society, particularly in handworkers [16,17]. LBP not only harms the patient’s body, but can also limit their personal and social life. Occupational and psychosocial stresses are also considered risk factors for LBP [18,19]. Workload, shift work, workplace violence, and job stress all affect musculoskeletal injuries, particularly LBP [20,21]. Clinicians and researchers aim to measure and quantify this effect, and now have the ability to compare and share these parameters with other colleagues. We have selected MVAS because it is easy to use and supports different aspects of daily and social life. The MVAS questionnaire is one of the most-used instruments to assess LBP by clinicians and researchers alongside Roland-Morris Disability Questionnaire (RDQ) [22], Oswestry Disability Index (ODI) [23], and Quebec Back Pain Disability Scale [10,24].
Similar to the RDQ, the MVAS questions ask the patient about their own capabilities. In other words, MVAS is a performance-based questionnaire and not capacity-based. This is important because capacity-based questionnaires tend to overestimate or underestimate their condition and ability [25]. Unlike ODI and RDQ, which measure the effect of pain on patient’s activities, MVAS concerns itself with the effect of activities on pain, which makes it a unique instrument.
One of the limitations of our study was not assessing responsiveness, which reflects how good an instrument is in detecting small changes in answers after an event such as therapeutic intervention [26]. As MVAS uses a visual scale, it can potentially be one of the most powerful tools to assess responsiveness. Therefore, future studies are warranted in this domain for the Persian MVAS. There are also some limitations to the use of both original and Persian MVAS. Due to the use of VAS, it is difficult to complete the questionnaire over telephone. The other downside of MVAS compared to RDQ is that there is no specific time course assigned to the answers. With the RDQ, the questions must be answered based on the experience of the patient over the last 24 hours.
The Persian Version of MVAS is recommended for the evaluation of patient activities on pain, owing to its ease of administration, assessment of social and daily life, and excellent validity and reliability. Clinicians can benefit from administration of MVAS in combination with a physical examination.
Fig. 1.
Standard path way estimation of confirmatory factor analysis. F1, daily activities; F2, body functions; F3, social life.
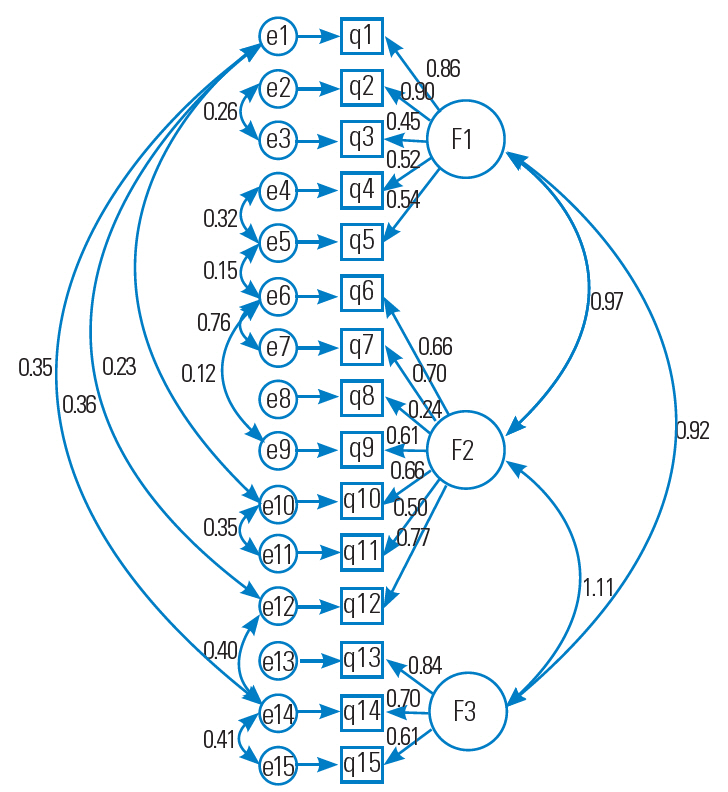
Table 1.
Confirmatory factor analysis of seven domains in Million Visual Analogue Scale Questionnaire
| χ2 | Degrees of freedom | p-value | Root mean square error of approximation | Goodness of fit index | Comparative fit index |
|---|---|---|---|---|---|
| 117.783 | 76 | 0.002 | 0.046 | 0.902 | 0.969 |
Table 2.
The confirmatory factor analysis standard beta and reliability index (Cronbach’s alpha and ICC)
References
1. Licciardone JC. The epidemiology and medical management of low back pain during ambulatory medical care visits in the United States. Osteopath Med Prim Care 2008 2:11.



2. Fullen BM, Baxter GD, O’Donovan BG, Doody C, Daly L, Hurley DA. Doctors’ attitudes and beliefs regarding acute low back pain management: a systematic review. Pain 2008 136:388–96.


3. Indahl A, Velund L, Reikeraas O. Good prognosis for low back pain when left untampered: a randomized clinical trial. Spine (Phila Pa 1976) 1995 20:473–7.


4. Gore M, Sadosky A, Stacey BR, Tai KS, Leslie D. The burden of chronic low back pain: clinical comorbidities, treatment patterns, and health care costs in usual care settings. Spine (Phila Pa 1976) 2012 37:E668–77.


5. Childs JD, Fritz JM, Wu SS, et al. Implications of early and guideline adherent physical therapy for low back pain on utilization and costs. BMC Health Serv Res 2015 15:150.



6. Mousavi SJ, Parnianpour M, Mehdian H, Montazeri A, Mobini B. The Oswestry Disability Index, the Roland-Morris Disability Questionnaire, and the Quebec Back Pain Disability Scale: translation and validation studies of the Iranian versions. Spine (Phila Pa 1976) 2006 31:E454–9.


7. Stratford PW, Binkley J, Solomon P, Gill C, Finch E. Assessing change over time in patients with low back pain. Phys Ther 1994 74:528–33.



8. Grotle M, Brox JI, Vollestad NK. Functional status and disability questionnaires: what do they assess?: a systematic review of back-specific outcome questionnaires. Spine (Phila Pa 1976) 2005 30:130–40.


9. Million R, Hall W, Nilsen KH, Baker RD, Jayson MI. Assessment of the progress of the back-pain patient 1981 Volvo Award in Clinical Science. Spine (Phila Pa 1976) 1982 7:204–12.


10. Longo UG, Loppini M, Denaro L, Maffulli N, Denaro V. Rating scales for low back pain. Br Med Bull 2010 94:81–144.



11. Munro BH. Statistical methods for health care research. 5th ed. New York (NY): Lippincott Williams and Wilkins; 2005.
12. Akbari H, Satkin M, Gangi M, Akbari H, Fesharaki MG. Standardization and study of psychological properties of the HSE Stress Questionnaire. Iran Red Crescent Med J 2017 19:e40466. https://doi.org/10.5812/ircmj.40466

14. Grace JB. Structural equation modeling and natural systems. New York (NY): Cambridge University Press; 2006.
15. Guillemin F, Bombardier C, Beaton D. Cross-cultural adaptation of health-related quality of life measures: literature review and proposed guidelines. J Clin Epidemiol 1993 46:1417–32.


16. Andersson GB, Svensson HO, Oden A. The intensity of work recovery in low back pain. Spine (Phila Pa 1976) 1983 8:880–4.


17. Lunde LK, Koch M, Hanvold TN, Wærsted M, Veiersted KB. Low back pain and physical activity: a 6.5 year follow-up among young adults in their transition from school to working life. BMC Public Health 2015 15:1115.




18. Kamalikhah T, Morowatisharifabad MA, Rezaei-Moghaddam F, Ghasemi M, Gholami-Fesharaki M, Goklani S. Alexander technique training coupled with an integrative model of behavioral prediction in teachers with low back pain. Iran Red Crescent Med J 2016 18:e31218.



19. Sorensen CJ, George SZ, Callaghan JP, van Dillen LR. Psychological factors are related to pain intensity in back-healthy people who develop clinically relevant pain during prolonged standing: a preliminary study. PM R 2016 8:1031–8.



20. Rezaee M, Ghasemi M. Prevalence of low back pain among nurses: predisposing factors and role of work place violence. Trauma Mon 2014 19:e17926.



21. Shieh SH, Sung FC, Su CH, Tsai Y, Hsieh VC. Increased low back pain risk in nurses with high workload for patient care: a questionnaire survey. Taiwan J Obstet Gynecol 2016 55:525–9.



22. Roland M, Morris R. A study of the natural history of back pain: part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976) 1983 8:141–4.



23. Fairbank JC, Couper J, Davies JB, O’Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy 1980 66:271–3.


24. Kopec JA, Esdaile JM, Abrahamowicz M, et al. The Quebec Back Pain Disability Scale: measurement properties. Spine (Phila Pa 1976) 1995 20:341–52.









