|
 |
- Search
| Asian Spine J > Volume 12(5); 2018 > Article |
|
Abstract
Purpose
To compare the efficacy between virtual reality intervention (using Nintendo Wii) along with conventional occupational therapy and conventional occupational therapy alone in improving upper limb function in patients with spinal cord injury (SCI).
Overview of Literature
The use of virtual reality has gained importance in the rehabilitation sector over the last few years. Nintendo Wii has the potential to encourage upper limb function while engaging in an interesting activity, which is important in long-term interventions, such as the treatment of SCI.
Methods
Overall, 22 patients with SCI participated in the study. They were randomly assigned to two groups. Group I received 30 minutes of virtual reality intervention (using Nintendo Wii) and 30 minutes of conventional therapy, whereas group II received conventional therapy only for 30 minutes. Both groups received therapy 3 days a week for 4 weeks. One hand of each patient was identified as the target hand based on the inclusion criteria. All patients were assessed at baseline, 2 weeks and 4 weeks (post-intervention), and 6 weeks (follow-up). The functional ability of the target hand was assessed using the Capabilities of Upper Extremity (CUE) questionnaire. Gross motor dexterity was assessed using the Box and Block Test (BBT). The level of independence in activities of daily living was assessed by the Spinal Cord Independence Measure-Self Report and quality of life by the World Health Organization Quality of Life-BREF.
Spinal cord injury (SCI) is a devastating state of disability encountered in todayŌĆÖs health care environment [1]. It is a low incidence, high cost impairment requiring tremendous changes in an individualŌĆÖs lifestyle [2]. The extent of an individualŌĆÖs impairment varies according to the level of lesion and location and severity of injury [3]. Approximately half of all patients with SCI have tetraparesis due to cervical injury [1].
Spinal cord injuries at the cervical level have a higher prevalence than those at the thoracic and lumbar levels [4]. One of the most distressing aspects of SCI at the cervical level is the impairment of arm and hand function, and this has a great impact on the level of independence [5]. The rehabilitation program, duration of hospital stay, and degree of independence depend, to a great measure, on the impaired function of upper limbs. Therefore, the extent and severity of impaired upper limb function in tetraplegia is of critical significance for independence [6].
These deficits in hand functions are primarily the results of the damage to descending motor pathways, which are responsible for fine control of the hand and finger [7]. Injury to the cervical spinal cord adversely affects the arm and hand function to a varying degree depending on the level and severity of injury. Recovery of function after SCI chiefly depends on the preservation of some anatomic connections and physiologic reorganization of the brain and spinal cord [8]. Factors that regulate recovery in traumatic SCI include baseline neurological level, baseline motor strength, and whether the injury is neurologically complete or incomplete [9]. Most of the recovery occurs within the first 6 months, with the greatest rate of change occurring within the first 3 months. Motor strength improvement continues during the second year, but at a slower pace and to a smaller degree [9,10].
Intensive task-specific training may augment hand function in people with tetraplegia. It is believed that therapy provides the damaged spinal cord with excitation from the sensorimotor cortex along with intensive sensory input from the periphery. Neural bombing in this kind on the damaged spinal cord promotes neural plasticity and may provide the critical stimulus required to elicit neurophysiologic and structural reorganization of the relevant pathways [11].
The recovery of function, both spontaneously and secondarily, to intense rehabilitative treatments, is sustained by plasticity and rewiring of the injured brain in adults. Activation of this mirror-neuron system, including the frontal, parietal, and temporal lobes, can encourage cortical reorganization, thereby contributing to functional recovery. Virtual reality- (VR-) based neuro-rehabilitation is a novel technology that allows users to interact in three dimensions with a computer-generated setting (a virtual world), thereby engaging the mirror-neuron system [12].
VR is a computer-based, interactive, multisensory simulation environment that occurs in real time. It presents users with opportunities to engage with what appears to be real world objects and events. It has the potential to create motivating and fun environments and to develop a range of skills and task-based techniques that can sustain participant interest and motivation. This results in better movement outcomes for rehabilitation purposes, demonstrating a greater range of functional improvements, including both active and passive upper limb joint range of motion, and a transfer of therapy gains into the activities of daily living (ADL) [13]. Systems such as Nintendo Wii encourage players to use natural actions and movements to play games. Wii is very flexible with respect to the movements that are needed to play the game, thereby offering the patient an opportunity to work on the affected upper limb with reasonable success, all the while benefiting from the visual feedback that the console offers.
The use of Nintendo Wii in upper limb rehabilitation is well documented in patients with stroke. However, there has been limited research regarding the use of VR for upper limb rehabilitation in patients with SCI. Therefore, the present study was designed to determine the effectiveness of Wii rehabilitation in upper limb functioning in patients with SCI and to identify its utilization as an adjunct to conventional occupational therapy program.
The study was approved by the Institutional Review Board of Indian Spinal Injuries Center, New Delhi, India and is registered with the Clinical Trials Registry under number CTRI/2016/11/007448. Written informed consents were obtained from the subjects.
This was a pilot, randomized, single-blinded, parallel group trial comprising 22 patients with cervical SCI. This study was conducted at the Indian Spinal Injuries Centre in New Delhi during September 2015ŌĆōMarch 2016 and included all patients with cervical SCI from the inpatient as well as the outpatient department of the hospital. Patients were included if they were aged 18ŌĆō55 years (either male or female), had complete or incomplete motor paralysis due to SCI at the neurological level of C5ŌĆōC8 [11], were at least 6 months post SCI [11], had undergone rehabilitation for 4ŌĆō8 weeks, had the ability to hold a 2.54-cm block of Box and Block apparatus with the thumb, were alert and medically stable, and were able to read and understand either the English or Hindi language.
Patients were excluded if they were unable to follow commands, had any other type of neurological injury affecting the target upper limb [11], had uncorrected vision, had pain in the affected upper limb restricting upper limb movement [13], had a pacemaker or implantable cardioverter-defibrillator device, or had a history of seizures [12]. A patient was considered to have withdrawn from the trial either when the consent was revoked or when the patient could not be contacted.
Prior to the intervention, baseline characteristics, including demographics (age, sex), educational status, time since injury, level of injury, and dominant and target hand, were collected. The demographic and clinical characteristics of the patients are presented in Table 1.
One hand of each patient was identified as the target hand on the basis of the inclusion criteria. In conditions where both hands met the criteria, the hand having better grip and pinch strength was identified as the target hand.
The following outcome measures were evaluated at baseline, 2 weeks and 4 weeks (post-intervention), and 6 weeks (follow-up): the Capabilities of Upper Extremity (CUE) questionnaire (score of 1ŌĆō7) for functional ability of the target hand and the Box and Block Test (BBT) for gross motor dexterity. The Spinal Cord Independence MeasureŌĆōSelf Report (SCIM-SR) was used to assess the level of independence in ADL, and quality of life was assessed using the World Health Organization Quality of Life-BREF (WHOQOL-BREF) by a blinded assessor who was not involved in the administration of the study intervention.
After screening the patients according to the inclusion and exclusion criteria and obtaining the informed consent, the baseline assessment was performed and the patients were randomly allocated to either of the two groups, i.e., the experimental group (group I) or the control group (group II), by fixed random allocation method. The allocation ratio was 1:1. The patients in group I received a treatment program comprising 12 interventional sessions (NWii and conventional therapy [CT]) of 60 minutes, 3 days a week for 4 weeks. The NWii was calibrated before each training session. The patient was asked to hold the Wiimote in their target hand to control play. When necessary, they were allowed to stabilize the Wiimote using the other hand. For patients with a weak grasp, the Wiimote was strapped to their hand by either a glove or with a crepe bandage.
Therapy included playing the Wii Sports Resort game of Table Tennis, Swordplay Speed Slice, Bowling, and Cycling. The NWii training session lasted for 30 minutes (excluding set-up time). Along with the NWii intervention, the patients also received 30 minutes of conventional hand therapy and strength training. After the final therapy session, satisfaction and perceived functional improvement with Wii-based movement therapy were rated on a scale of 10 using a visual analog scale.
The patients in group II or in the control group also underwent 12 interventional sessions of 30 minutes, 3 days a week for 4 weeks. They received the traditional hand therapy protocol only. This included strength training of the target upper limb (active or active assisted movements) and functional tasks such as reaching, moving checkers, grasping and releasing objects, and manipulating and rotating objects.
Statistical analysis was performed using SPSS ver. 16.0 (SPSS Inc., Chicago, IL, USA). Analysis was done for 20 patients (11 in group I and nine in group II) who completed the study. Repeated measures analysis of variance (ANOVA) was performed to check the within group analysis, and an independent sample t-test was performed to check the between group analysis among the baseline, 2 weeks, 4 weeks, and 6 weeks scores for CUE questionnaire, BBT, SCIM-SR, and WHOQOL-BREF. Statistical significance was set at pŌēż0.05 with a 95 % confidence interval.
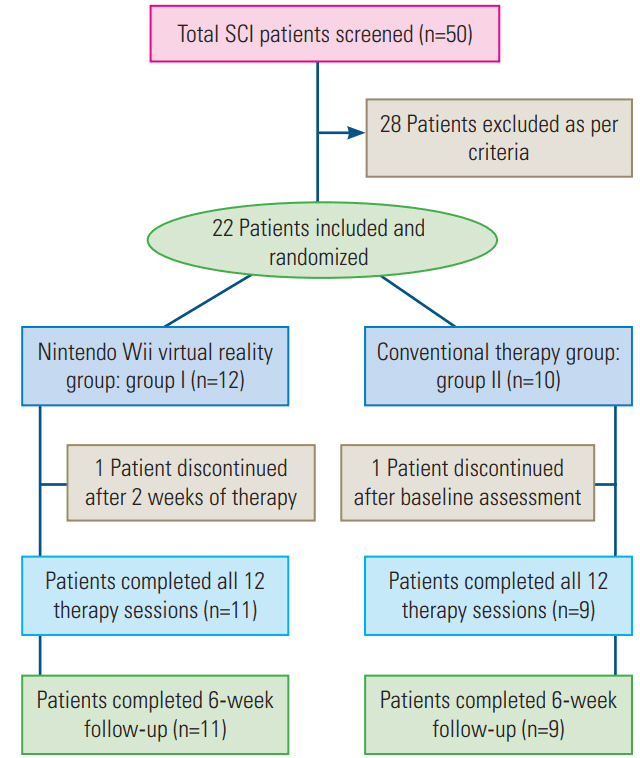
From September 2015 to March 2016, 50 potential candidates diagnosed with cervical SCI were identified as being able to participate in the study; of them, 28 patients were excluded for not meeting the criteria. Therefore, 22 patients (44%) were evaluated. Of them, 12 patients were randomized to group I and 10 patients were randomized to group II via computer-generated random allocation. One patient dropped out of group I after the first 2 weeks of treatment, and one patient dropped out of group II after the baseline assessment. Finally, 20 randomized patients (11 in group I and nine in group II) were subjected to further follow-up and analysis (Fig. 1).
Mean age was 28.32┬▒7.93 years (range, 18ŌĆō47 years). The patients in group I were younger (mean age, 23.67┬▒5.19 years) than those in group II (mean age, 33.9┬▒7.09 years). Out of the 22 patients included in the study, 21 (95%) were male and one (5%) was a female.
Mean time from SCI onset to enrollment was 12.89┬▒9.29 months (range, 6ŌĆō46 months). Mean time since injury was 15.17┬▒11.22 months and 10.15┬▒5.71 months in group I and group II, respectively. Overall, 15 patients were treated for their right hand and seven for their left hand.
The between group analysis through an independent t-test showed no significant improvement in CUE questionnaire, BBT, SCIM-SR, and WHOQOL-BREF scores. However, mean scores in the VRWii group were higher than those in the control group, whereas the within group comparison using repeated measures ANOVA showed significant improvement in both groups for CUE questionnaire, BBT, and SCIM-SR scores. WHOQOL-BREF scores did not show any significant change in either of the groups.
Statistically significant improvements were seen in CUE questionnaire, BBT, and SCIM-SR scores in group I. Statistically significant improvement was not seen in WHOQOL-BREF in group I. Statistically significant improvement was not seen in group II for CUE questionnaire, SCIM-SR, and WHOQOL-BREF scores. However, BBT showed significant improvement in the control group.
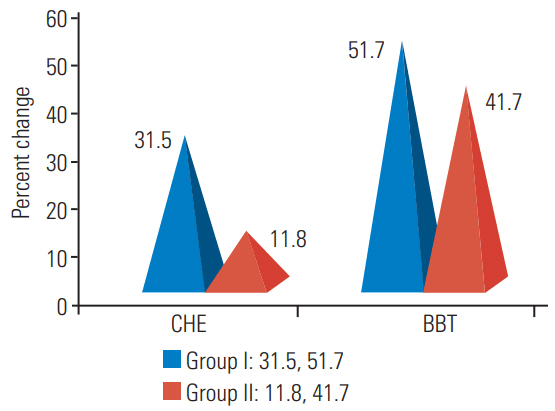
Fig. 2 shows the average percentage change in the pre-intervention and post-intervention scores of CUE questionnaire and BBT for group I and group II. The raw scores of patients from CUE questionnaire and BBT indicates that Nintendo Wii along with conventional therapy (group I) had a greater percentage change from pre-intervention to post-intervention (31.5┬▒29.7 for CUE questionnaire and 51.7┬▒56.2 for BBT) than conventional therapy alone (group II: 11.8┬▒20.2 for CUE questionnaire and 41.7┬▒70.9 for BBT) (Table 2).
Feedback on Nintendo Wii gaming from patients who completed the study: When asked to rate their satisfaction with Wii-based therapy, the patients were highly satisfied, with a mean score of 8.17┬▒1.2 (range, 6ŌĆō10) on the Visual Analog Scale. No adverse effects were reported by any patient, although the problem encountered during the intervention was the difficulty in holding the Wii mote due to poor grasp (seven patients). This problem was overcome by strapping either by bandage or gloves, as mentioned earlier.
The aim of this pilot, randomized, controlled trial was to investigate the effects of an intensive and repetitive VR program combined with CT on upper limb function in patients with subacute and chronic complete and incomplete tetraplegia. We compared the results obtained after 12 treatment sessions over a period of 30 days between two groups: group I and group II. The findings of the study showed that VR added to conventional therapy produced similar functional changes in upper limb function as did conventional therapy alone. However, a high level of satisfaction was seen in patients using VR.
The sample in our study comprised tetraplegics, both complete and incomplete. Significant differences were not found between the two treatments in terms of the outcome measures.
The findings of this study were consistent with those reported by Dimbwadyo et al. [14] in 2016 that VR along with conventional therapy produces similar results in upper limb function when compared to only conventional therapy. In the present study, the small sample size (N=22) may have contributed to the absence of statistical significance between the two groups. Although statistically significant differences in the effectiveness between the two groups were not found, the patients in group I had improved upper extremity motor function ability, which was seen by a greater percent change from pre-intervention to post-intervention in CUE questionnaire and BBT scores.
This result demonstrated that Nintendo Wii in combination with conventional therapy could be equivalent to conventional rehabilitation for improving upper extremity motor functions, which is consistent with the results of Gustavo et al for stroke rehabilitation, representing the VRWii gaming technology as a safe, feasible, and potentially effective alternative to facilitate rehabilitation therapy and promote recovery [15].
VR gaming allows users to interact with a computersimulated environment and receive near real-time feedback on performance [15]. Rehabilitation is an essential component to any program aimed at improving motor function in patients with SCI [16]. Researches have shown that neuroplasticity is enhanced by repetitive, high-intensity, task-specific activities [16,17], which is due to cortical reorganization and rewiring in the brain [16,18]. VR Nintendo Wii shows practice-dependent improvement of the functional ability of the target hand through real-time visual biofeedback and allows patients to undergo taskspecific, high-intensity, repetitive activities that mimic real world activities in a safe environment. Not only this, it allows for the modification of difficulty levels based on the patientŌĆÖs deficit, allowing for greater neuroplasticity and patient recovery [17].
All patients in both the groups gained improved functional use of the target arm and hand during both testing and in ADL. Furthermore, the patients reported a high level of satisfaction, resulting in greater adherence to the treatment on the patientŌĆÖs part. The success of Wii-based movement therapy has been demonstrated previously in patients in the early subacute period (<3 months) after stroke [19]. However, its application in patients with SCI is limited. The Wii and Wii Sports Resort were used without modifications. The result obtained from our study suggests the following benefits of using the Nintendo Wii as part of the rehabilitation process: it provides increased motivation leading to greater adherence to treatment; the patient receives positive feedback seeing results in the form of scores and moving to higher levels of difficulty. It also allows the individual to learn new self-improvement strategies [19], which was reflected by the feedback scores of the patients who underwent Wii-based therapy and also by the consistent improvement in their scores while playing the games. It expedites interest and motor learning, promoting motivation through the in-built commentary, prizes, visual and verbal cues, and tapping into patientsŌĆÖ competitive nature and their desire for interaction, thereby further facilitating compliance and motivation [20]. The patients work with functional movements that are to be performed at a specific time determined by a visual stimulus, which further leads to visual-motor integration. Being fairly inexpensive, Nintendo Wii can be used on a long-term basis as an adjunct to outpatient rehabilitation tool or even at home to address the leisure needs of patients, even in those with high levels of injury [19,21]. The automated nature of stimulus delivery within the virtual environment enables the therapist to focus more on providing maximum physical support to the patient, when needed, without being distracted by the complexity of the task and withdrawing their support as the function improves [22].
This study extended the use of Wii-based movement therapy in the functional ability of the target hand in subacute and chronic SCI. The functional ability of the target hand increased in therapy (as was seen by improvement in scores while playing the games) as well as in the real world (improvement in CUE questionnaire, BBT, and SCIM-SR scores) in patients with subacute as well as in patients with chronic SCI. Furthermore, improvements were seen at follow-up, i.e., data collected at 6 weeks, and the improvements remained the same in the rest, albeit four patients, suggesting that there may be sustenance of therapeutic benefit following Nintendo Wii therapy.
While improvements have been seen in upper limb function after VR treatment along with conventional therapy in subacute and chronic stroke patients, the evidence of its application in tetraplegia is still very limited. Therefore, we believe that our study adds to the limited evidence for VR-based therapy for upper limb function in patients with tetraplegia. The results indicate that participation in Nintendo Wii activity adds to the functional gains. However, the results do not determine which type of intervention was more beneficial in positively impacting functional skills and upper extremity function.
The treatment and rehabilitation period for tetraplegia are long, expensive, and exhausting. As a rehabilitation supplement, VR has shown several motivating factors, such as perceived control, curiosity, exploration, competition, and social interaction. It provides a more engaging treatment for people with tetraplegia within the context of therapeutic goals and decreasing therapist support. VR use does not replace conventional rehabilitation, rather it adds a dimension of enjoyment by offering an opportunity for socialization and leisure. It acts like rudimentary ŌĆ£biofeedback,ŌĆØ as the patients see how they respond to specific stimuli. It allows patients to track their progress within the gameŌĆÖs scoring system and monitor their performance on a day-to-day basis.
The results of this study do not negate the addition of Nintendo Wii into rehabilitation; they provide important guidelines for future researches in this area. Therefore, we infer that adding VR-based movement therapy to traditional rehabilitation strategies may be useful in increasing the dosage of therapy and for augmenting patientŌĆÖs engagement and motivation during the process.
However, the limitations of our study deserve comment. This was a pilot study with a small sample size. Because most of the patients in this study were incomplete, a group of patients with complete cervical SCI should be included in future studies to determine the influence of the injury in the effectiveness of VR treatments. Moreover, only traumatic cases of SCI were included in the study. Thus, the results cannot be generalized to non-traumatic cases. Lastly, the duration of the intervention was short (12 sessions in 4 weeks).
In summary, this study constitutes the initial step in the understanding of the potential benefits of VR intervention. However, it requires more randomized clinical trials with larger sample size and follow-up. It also needs to be independently compared to conventional therapy to finally ascertain its effectiveness and validation.
Fig.┬Ā2.
The average percentage change of group I and group II from pre-intervention to post-intervention. CUE, Capabilities of Upper Extremity; BBT, Box and Block Test.
Table┬Ā1.
Demographic and clinical characteristics of the patients included in the study
| Characteristic | Group I (n=12) | Group II (n=10) |
|---|---|---|
| Age (yr) | 23.7┬▒5.2 | 33.9┬▒7.1 |
| Sex | ||
| ŌĆāMale | 11 (92) | 10 (100) |
| ŌĆāFemale | 1 (8) | 0 |
| Neurological level | ||
| ŌĆāC5 | 5 (42) | 6 (60) |
| ŌĆāC6 | 6 (50) | 3 (30) |
| ŌĆāC7 | 1 (8) | 1 (10) |
| ISNCSCI gradea) | ||
| ŌĆāASIA-A | 1 (8) | 4 (40) |
| ŌĆāASIA-B | 6 (50) | 3 (30) |
| ŌĆāASIA-C | 2 (17) | 2 (20) |
| ŌĆāASIA-D | 3 (25) | 1 (10) |
| Spinal cord injury type | ||
| ŌĆāComplete | 1 (8) | 4 (40) |
| ŌĆāIncomplete | 11 (92) | 6 (60) |
| ŌĆāTime since injury (mo) | 15.2┬▒11.2 | 10.2┬▒5.7 |
| Dominant hand | ||
| ŌĆāRight hand | 12 (100) | 10 (100) |
| ŌĆāLeft hand | 0 | 0 |
| Target hand | ||
| ŌĆāRight hand | 6 (50) | 9 (90%) |
| ŌĆāLeft hand | 6 (50) | 1 (10%) |
Table┬Ā2.
Pre- and post-intervention CUE and BBT scores of both group I and group II
References
1. American Spinal Injury Association. International standards for neurological classification of spinal cord injury. Chicago (IL): American Spinal Injury Association; 2002.
2. OŌĆÖSullivan SB, Schmitz TJ,Traumatic spinal cord injury. OŌĆÖSullivan SB, Schmitz TJ, editors. Physical rehabilitation. New Delhi: Jaypee Brothers Medical Publishers; 2007.
3. Miller RC, Popovic MR, Thrasher AT, Verrier M. Functional electrical stimulation therapy improves grasping in chronic cervical spinal cord injury: two case studies. J Autom Control 2008 18:53ŌĆō61.

4. Agarwal P, Upadhyay P, Raja K. A demographic profile of traumatic and non-traumatic spinal injury cases: a hospital-based study from India. Spinal Cord 2007 45:597ŌĆō602.



5. Snoek GJ, IJzerman MJ, Hermens HJ, Maxwell D, Biering-Sorensen F. Survey of the needs of patients with spinal cord injury: impact and priority for improvement in hand function in tetraplegics. Spinal Cord 2004 42:526ŌĆō32.



6. Curt A, Dietz V. Traumatic cervical spinal cord injury: relation between somatosensory evoked potentials, neurological deficit, and hand function. Arch Phys Med Rehabil 1996 77:48ŌĆō53.


7. Pamela KL, Cynthia CN. Joint structure and function: a comprehensive analysis. 4th ed. Philadelphia (PA): F. A. Davis Company; 2006.
8. Green JB, Sora E, Bialy Y, Ricamato A, Thatcher RW. Cortical sensorimotor reorganization after spinal cord injury: an electroencephalographic study. Neurology 1998 50:1115ŌĆō21.


9. Hoffman LR, Field-Fote EC. Cortical reorganization following bimanual training and somatosensory stimulation in cervical spinal cord injury: a case report. Phys Ther 2007 87:208ŌĆō23.



10. Harvey LA, Batty J, Jones R, Crosbie J. Hand function of C6 and C7 tetraplegics 1 - 16 years following injury. Spinal Cord 2001 39:37ŌĆō43.



11. Raineteau O, Schwab ME. Plasticity of motor systems after incomplete spinal cord injury. Nat Rev Neurosci 2001 2:263ŌĆō73.



12. Kirshblum S, Millis S, McKinley W, Tulsky D. Late neurologic recovery after traumatic spinal cord injury. Arch Phys Med Rehabil 2004 85:1811ŌĆō7.


13. Lynskey JV, Belanger A, Jung R. Activity-dependent plasticity in spinal cord injury. J Rehabil Res Dev 2008 45:229ŌĆō40.



14. Dimbwadyo-Terrer I, Gil-Agudo A, Segura-Fragoso A, et al. Effectiveness of the virtual reality system Toyra on upper limb function in people with tetraplegia: a pilot randomized clinical trial. Biomed Res Int 2016 2016:6397828.




15. Ortiz-Catalan M, Nijenhuis S, Ambrosch K, BovendŌĆÖEerdt T, Koenig S, Lange B,Virtual reality. Pons JL, Torricelli D, editors. Emerging therapies in neurorehabilitation. Berlin: Springer-Verlag; 2014. p.249ŌĆō65.
16. Halton J. Virtual rehabilitation with video games: a new frontier for occupational therapy. Occup Ther Now 2008 9:12ŌĆō4.
17. Yong Joo L, Soon Yin T, Xu D, et al. A feasibility study using interactive commercial off-the-shelf computer gaming in upper limb rehabilitation in patients after stroke. J Rehabil Med 2010 42:437ŌĆō41.


18. Mouawad MR, Doust CG, Max MD, McNulty PA. Wii-based movement therapy to promote improved upper extremity function post-stroke: a pilot study. J Rehabil Med 2011 43:527ŌĆō33.


19. Harvey LA, Dunlop SA, Churilov L, Hsueh YS, Galea MP. Early intensive hand rehabilitation after spinal cord injury (ŌĆ£Hands OnŌĆØ): a protocol for a randomised controlled trial. Trials 2011 12:14.




20. Rahman S, Shaheen A. Virtual reality use in motor rehabilitation of neurological disorders: a systematic review. Middle-East J Sci Res 2011 7:63ŌĆō70.
21. Deutsch JE, Brettler A, Smith C, et al. Nintendo Wii sports and Wii fit game analysis, validation, and application to stroke rehabilitation. Top Stroke Rehabil 2011 18:701ŌĆō19.


22. Hatfield ML. Virtual reality in rehabilitation: project at International Cooperation at the faculty of Biomedical Engineering CTU. Prague: Czech Technical University in Prague; 2013.