|
 |
- Search
| Asian Spine J > Volume 8(5); 2014 > Article |
Abstract
Purpose
To compare the treatment outcome of nocturnal leg cramps in lumbar spinal canal stenosis (LSCS) patients on conservative treatment with historical surgical cohorts and to determine the sensitivity and specificity as well as positive predictive value and negative predictive value of knee flexion test suggested for LSCS patient.
Overview of Literature
True prevalence of nocturnal leg cramps in LSCS patients as well as the clinical outcome of its surgical treatment have been reported.
Methods
A questionnaire suggested from previous study with minor modifications was used in this study. Clinical data was collected. Knee flexion test was performed in two groups.
Results
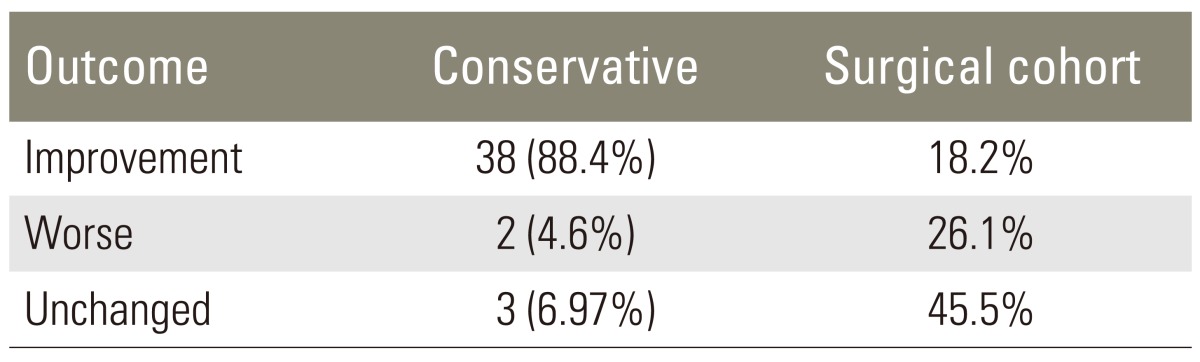
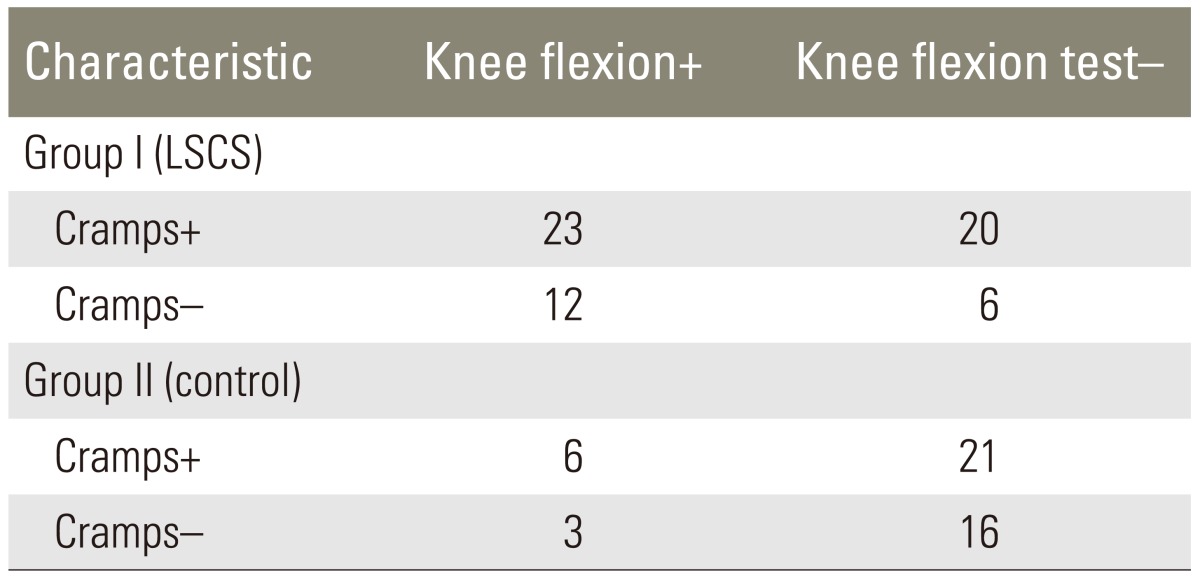
The prevalence of nocturnal leg cramp was higher in the LSCS group compared to the control group (second group). In LSCS patients, 38 (88%) had improved leg cramps after the conservative treatment, 3 (6.97%) remained unchanged, and 2 (4.6%) had worsened leg cramps. Of the 43 patients, 21 (48.8%) had no disturbance to their activities of daily living. In the LSCS group, the sensitivity and specificity of the knee flexion test was 53.5% and 33.3%, respectively. The knee flexion test in the LSCS group had a positive predictive value and a negative predictive value of 65.71% and 23.1%, respectively.
Lumbar spinal canal stenosis (LSCS) has variable presentation: the most common presentation is neurogenic claudication followed by leg pain and back pain. Restless leg sensation, chilliness and paraesthesia are other symptoms often less attended by spinal care professionals. One the few noticed symptoms, such as leg cramps, are often ignored or less noticed in patients with LSCS. Leg cramps are acute involuntary painful contractions of the muscles in the lower extremities. These cramps affect athletes, pregnant women, and the elderly population [1,2,3,4,5,6]. A majority of these patients can be treated conservatively; if the conservative treatment ultimately fails, surgery is performed done. Previous general population surveys have reported that leg cramps occur in 38% to 50% of the elderly population [1,2,3,4]. Despite the fact that its etiology remains unknown, leg cramps have been reported to be associated with various diseases like diabetes, neuromuscular diseases, hyperthyroidism, hypertension, hypocalcaemia, hypokalaemia, vascular diseases, and some medications including diuretics, statins, steroids, and nifedipine-blockers, etc. [2,5,7].
The term 'nocturnal cramp' has been given due its occurrence mostly at night is actually a 'misnomer,' because in our experience these occur during different times of the day. Another study [8], has looked into the possible relationship between leg cramps and surgical interventions that have an impact on leg cramps in patients with LSCS. Our hypothesis is that leg cramps can be treated conservatively and surgical intervention should be done in selected cases after failed conservative treatment. The other purpose of this study was to look into the variations in patterns with respect to time of and site of occurrence. The knee flexion test previously suggested by Demircan et al. [9] for the clinical diagnosis of these cramps was evaluated for its sensitivity, specificity, positive predictive value and negative predictive value.
We prospectively assessed and treated sixty-one patients with LSCS from April 2013 to June 2013. Our study also included patients already being conservatively managed for more than a month. The diagnosis was confirmed by clinical examination, radiological assessment by magnetic resonance imaging (MRI), or spine fellows and the chief of spine services examining previous case records. After a thorough clinical assessment, a questionnaire was recorded by the spine fellow.
Group 1 included patients with LSCS who satisfied the following criteria: 1) Patients with typical signs and symptoms of LSCS (leg pain, neurogenic claudication) that was confirmed on MRI; 2) Patients without any history of previous lumbar spine surgeries; 3) Patients without severe scoliosis (Cobb angle >20┬░) or spondylolisthesis (% slip >20%), which required instrumented fusion; and 4) Patients without any history of neuromuscular diseases such as cerebral palsy, congenital, and acquired myopathy, etc. Group II was a control group of 46 subjects selected from the general population; the subjects had no history of back surgery. The subjects had undergone a general health check-up and completed the questionnaire for low back pain.
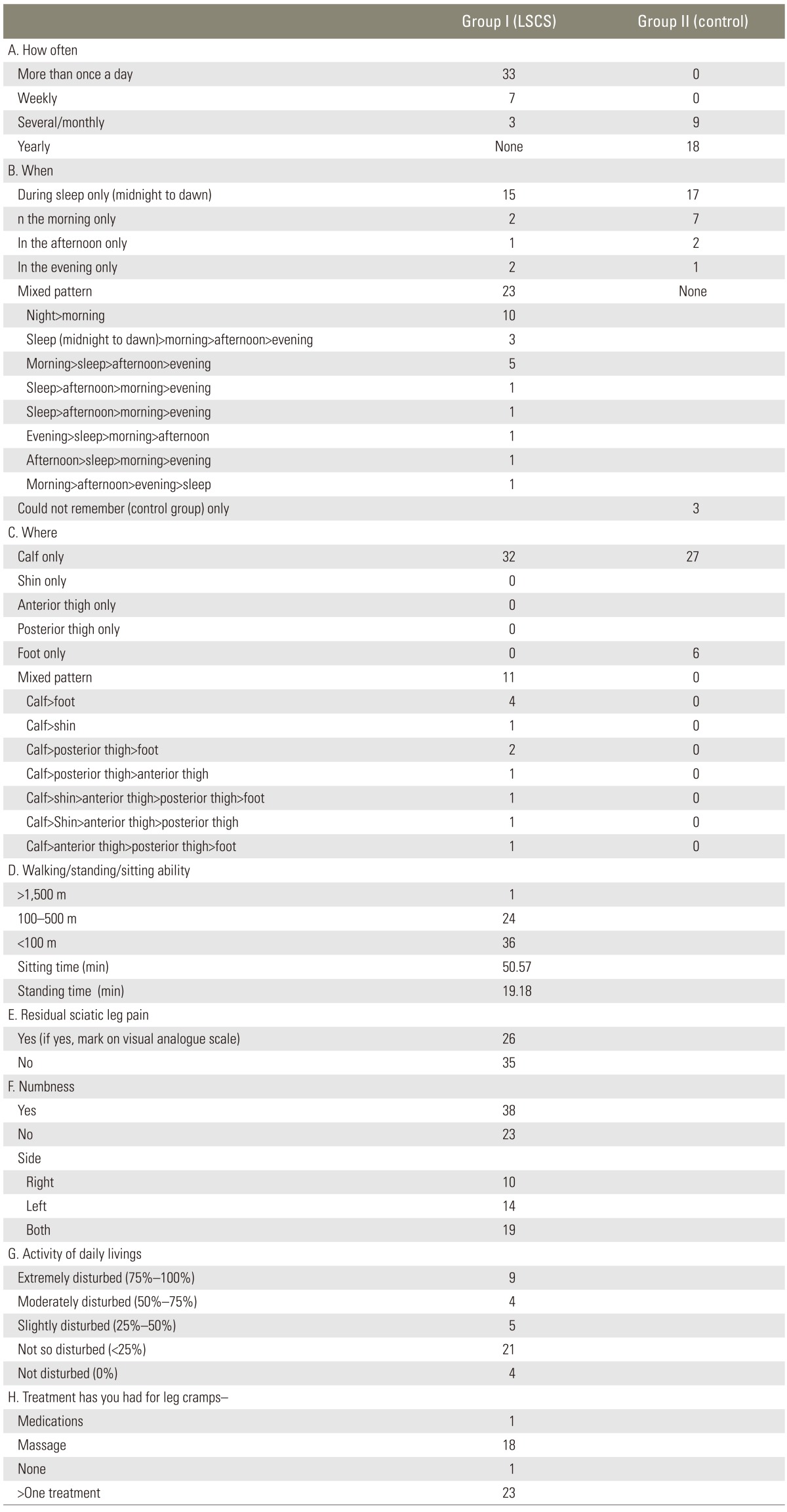
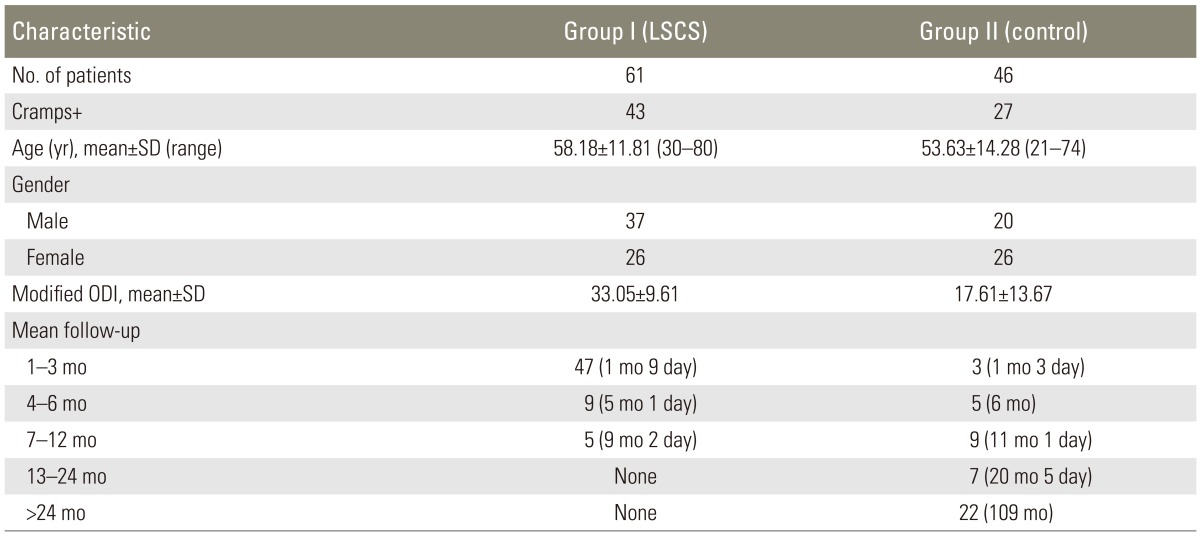
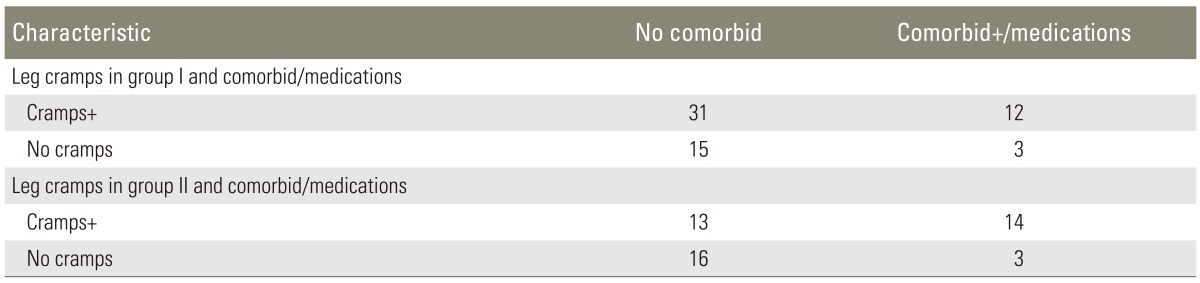
All participants in both groups filled in the questionnaire regarding the following issues: 1) Experience of leg cramps; 2) Frequency and time of day of cramp attack; 3) Area of cramps; and 4) Walking ability. Only LSCS patients filled in the questionnaire regarding the following issues; 5) Changes in cramps before and after conservative treatment; 6) Residual sciatica (evaluated by visual analogue scale, 0-10 points) and numbness in the legs and feet; 7) Activities of daily living (ADL) disturbance by leg cramps; 8) Satisfaction with conservative treatment modality [10]; 9) New modified the Oswestry disability index (ODI); 10) treatment for leg cramps. This questionnaire was used in a previous study [8], and changes were made from the previous questionnaire for question 11: in addition to a more qualitative (subjective) assessment of leg cramps, we also added a question where the effect of leg cramps on ADL was expressed as a percentage. Association of diabetes mellitus and hypertension, which are the most common comorbidities of elderly people and which have been reported to be associated with leg cramps [6,7,11], were also investigated. For LSCS patients, demographic data was collected that included age, sex, comorbidities, medications (known to cause nocturnal cramps), and history of previous spine surgery. The modification in ODI was given to all sections. If patient disability was not due to pain in any section, then a score of zero was given. Of all the patients, 72.09% in the LSCS group and 48.14% in the control group, patients had no comorbidities such as diabetes, hypertension, cardiac diseases, etc. Average follow-up was recorded at 3, 6, 12, 24, and >24 months. 47 patients had a minimum follow up of 1-3 months, 9 patients had 4-6 months follow-up. The maximum follow up in LSCS group was only for one year with minimum follow-up for 3 months. The rest of the socio-demographic data is given in Tables 1, 2. The results of Žć2 test between group I and group II for age and modified ODI is given in Tables 1, 2. Age and gender was matched between group I and group II; the p-value for age is 0.074 and gender is 0.250 (p-value>0.05) respectively; this means there was no significant differences between the groups in age or gender.
The clinical test was performed by holding the leg of the patient against forceful knee flexion. The test was considered positive if a disturbing cramp was produced in the leg or thigh region.
The chi-squared (Žć2) test and logistic regression analysis were used to compare the prevalence and treatment outcome of leg cramps between group I and II. A p-value less than 0.05 was considered statistically significant. Levene's test for equality of variance for logistic regression analyses using age, gender, and comorbidities as independent variables between group I and group II. The Pearson chi-square and Fisher exact test, along with linear by linear association, was established. The knee flexion test was evaluated for its sensitivity, specificity, positive predictive value, and negative predictive value in both groups.
Prevalence of leg cramps between group I (LSCS) and group II (control) was highly significant (i.e., p-value <0.001), when matched for occurrence with respect to the frequency (daily/weekly/monthly/yearly). The treatment outcome in group I was significant with a p-value<0.0001.
Of all study subjects, 70.5% of patients with LSCS and 58.6% in the control population experienced leg cramps.
A detailed description of the occurrence and pattern of leg ramps is provided Table 3. Among the mixed pattern of cramps, the most prevalent pattern was night>morning occurrence of cramps. 58.6% of patients experienced cramps at some point of time in the control group. 62.9% of patients experienced these cramps at night. There was significant difference in ODI in LSCS and control groups with mean 33.05┬▒9.61 and 17.61┬▒13.67, respectively.
The calf was the most common site of occurrence; a majority of the patients did not have residual sciatic pain and ADL was not as much affected. The treatment outcome is illustrated in Table 4.
The knee flexion test in the LSCS group was not significant with a p-value of p>0.254. The sensitivity and specificity of the test was 53.5% and 33.3%, respectively. The above test in LSCS group had positive reductive value of 65.71% and negative predictive value of 23.1%. The prevalence of the disease was 70.5%. Group II sensitivity and specificity was 22.2% and 84.2%, respectively. The predictive value and negative predictive value was 66.7% and 43.2%, respectively. The values are displayed in Table 5.
This is the first study that assesses outcomes of cramps following a conservative treatment regimen and compared the outcome from historical cohorts treated surgically. This is also the first study to study that looked into the pattern, timing, and site occurrence of cramps. This also first study to compare these cramps analysing between LSCS group and control group with similar age, gender, and comorbidities. Similar to the previous study, our findings confirmed these cramps have a higher prevalence in patients with LSCS than the general elderly population. However, the authors noticed several disparities in terms of our findings compared to previous studies. Matsumoto et al. [8] reported that cramps disturbed ADL in almost one-half of the patients and seldom improved after surgery, or even became worse in 26% of the patients. This was contrary to our findings in which 48% of our patients (21 out of 43) reported only 25% of their ADL was affected (G in Table 3). The same study reported that conservative treatment resulted in 85% of patients having complete resolution of cramps. In our study, the claudication distance showed improvement in only 50% of the patients. Looking into the pattern, we conclude that the word "nocturnal cramps" is a misnomer because these cramps do occur at other times than night time. Matsumoto et al. [8] also reported this pattern. Amyotrophic lateral sclerosis, poliomyelitis, peripheral neuropathy, lumbar spinal radiculopathy; metabolic disorders including diabetes, pregnancy, uremia, liver cirrhosis, and hypothyroidism; acute extracellular volume depletion including excessive perspiration, hemodialysis, diarrhea, and diuretic therapy; hereditary disorders; and medications including diuretics, antidepressants, calcium blockers, -blockers, statins, and steroid, diseases or disorders reported to be associated with cramps; lower motor neuron disorders including and so on. The exact causal mechanism of leg cramps is yet to be established [11,12,13]. Electromyographic studies have suggested that abnormalities in the motor units including motor neurons, neuromuscular junctions, and muscles can cause cramps [11,12,13]. Other hypotheses also exist such as changes in hydrostatic pressure and ionic shift across the cell membrane in the calf muscles in a recumbent position leading to hyper excitability of the motor neurons [11], accumulation of metabolites and focal ischemia could be the pathomechanism behind their occurrence. Disturbance in the functions of the lumbar spinal nerves controlling the tonus of the muscles innervated by them [13] was suggested as the possible etiology for the high incidence of leg cramps in patients with lumbar radiculopathy. The cause of these cramps in elderly has been attributed to the loss of motor neurons [14]. In LSCS patients, we filed all medications administered to the patients, and evaluated the prevalence of leg cramps with stratification by medications to investigate their possible association with leg cramps, but we found no difference in the prevalence between patients with such medications and those without, similar to the previous study [8].
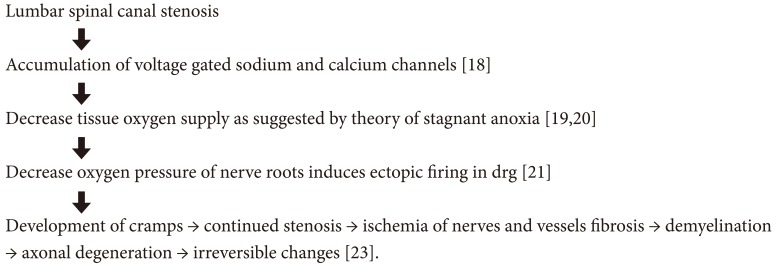
Few studies on the association between leg cramps and lumbar spinal diseases have been published. Rish [15] reported that leg cramps were frequent in patients with lumbar radiculopathy [16]. In a retrospective study, Haskell and Fiebach [17] used quinine sulphate for treatment of nocturnal leg cramps in comparison with age-matched controls, and concluded that peripheral vascular disorders and peripheral neurologic deficits were more common in patients than in the controls. A close association between LSCS and peripheral vascular disease has been reported. Explanation for the failure of any form of treatment is supported by literature [9] and is due to irreversible ischemic changes. This leads to irreversible damage to nerves, which explains the failure of conservative or surgical treatment to alleviate the symptoms of cramps (Fig. 1) [18,19,20,21,22,23].
Prolonged compression leads to irreversible damage to the lumbar nerve roots more often observed in patients with residual numbness after surgery as reported by Kobayashi et al. [24] in a dog nerve root compression model. This dysfunction of the motor neurons extends beyond the site of degeneration at the compression to the motor neurons within the lumbarspinal cord as a result of the axonal reaction. This pathology results in motor deficits that would not resolve immediately after surgery. The process of reinnervation of the affected muscles can enhance the hyperexcitability of the motor units [11,12,24]. The theory of accumulation of metabolites leading to these cramps and fatigue can be disapproved as suggested by the previous study [8] and our study since most of our patients improve in walking ability after conservative treatment without surgical intervention. Proposed remedies for leg cramps are stretching, massage, intake of vitamins B and E, magnesium, quinine, and anticonvulsants such as carbamazepine [18,25,26,27,28,29]. Quinine is an antimalarial drug, and has been reported to be effective for leg cramps by decreasing the excitability of the motor endplate, thereby reducing the muscle contractility [19]. In our study, comparison between the conservative treatment and historical surgical cohort's shows that neurotropic are quite effective to alleviate the symptoms of the leg cramps and conservative treatment was successful in 85% of these patients.
Demircan et al. [9] reported that knee flexion test was reported positive in 72% of patients with lumbar disc herniation. The sensitivity, specificity, positive predictive value and negative predictive value of this test was low and did not show a higher relevance as compared to control group as reported by the previous study. The gait load test reported by Kim et al. [30] is still the standard test for objective and quantitative assessment of neurogenic claudication and is also applicable to legs cramps.
Our study has a few limitations. The small number of study subjects could possibly alter some of the findings such as the pattern of occurrence of leg cramps and their distribution. Secondly, there was no blinding in the study and bias could not be ruled out. Thirdly, existence of preclinical stages of peripheral vascular disease cannot be made solely by pulse examination. The test could be positive in patients with established or preclinical stages of peripheral vascular disease. There is minimal literature regarding association of peripheral vascular disease with LSCS. Henceforth, the vascular theory regarding the occurrence of these cramps cannot be disapproved completely and needs further studies to study relationship between relationship of these cramps in LSCS and Peripheral vascular disease.
References
1. Young JB, Javid M, George J. Rest cramps in the elderly. J R Coll Physicians Lond 1989 23:103ŌĆō106. PMID: 2659779.


2. Abdulla AJ, Jones PW, Pearce VR. Leg cramps in the elderly: prevalence, drug and disease associations. Int J Clin Pract 1999 53:494ŌĆō496. PMID: 10692732.


3. Naylor JR, Young JB. A general population survey of rest cramps. Age Ageing 1994 23:418ŌĆō420. PMID: 7825490.


4. Butler JV, Mulkerrin EC, O'Keeffe ST. Nocturnal leg cramps in older people. Postgrad Med J 2002 78:596ŌĆō598. PMID: 12415081.



5. Dahle LO, Berg G, Hammar M, Hurtig M, Larsson L. The effect of oral magnesium substitution on pregnancy-induced leg cramps. Am J Obstet Gynecol 1995 173:175ŌĆō180. PMID: 7631676.


6. Vinciguerra G, Belcaro G, Cesarone MR, et al. Cramps and muscular pain: prevention with pycnogenol in normal subjects, venous patients, athletes, claudicants and in diabetic microangiopathy. Angiology 2006 57:331ŌĆō339. PMID: 16703193.


7. Kanaan N, Sawaya R. Nocturnal leg cramps. Clinically mysterious and painful--but manageable. Geriatrics 2001 56:3439ŌĆō42. PMID: 11417373.

8. Matsumoto M, Watanabe K, Tsuji T, et al. Nocturnal leg cramps: a common complaint in patients with lumbar spinal canal stenosis. Spine (Phila Pa 1976) 2009 34:E189ŌĆōE194. PMID: 19247159.


9. Demircan MN, Colak A, Kutlay M, Kibici K, Topuz K. Cramp finding: can it be used as a new diagnostic and prognostic factor in lumbar disc surgery? Eur Spine J 2002 11:47ŌĆō51. PMID: 11931063.


10. Roland M, Morris R. A study of the natural history of back pain. Part I: development of a reliable and sensitive measure of disability in low-back pain. Spine (Phila Pa 1976) 1983 8:141ŌĆō144. PMID: 6222486.


11. Fairbank JC, Pynsent PB. The Oswestry Disability Index. Spine (Phila Pa 1976) 2000 25:2940ŌĆō2952. PMID: 11074683.


13. Jansen PH, Lecluse RG, Verbeek AL. Past and current understanding of the pathophysiology of muscle cramps: why treatment of varicose veins does not relieve leg cramps. J Eur Acad Dermatol Venereol 1999 12:222ŌĆō229. PMID: 10461641.


14. Jansen PH, Joosten EM, Vingerhoets HM. Muscle cramp: main theories as to aetiology. Eur Arch Psychiatry Neurol Sci 1990 239:337ŌĆō342. PMID: 2140785.


16. Vandervoort AA. Aging of the human neuromuscular system. Muscle Nerve 2002 25:17ŌĆō25. PMID: 11754180.


17. Haskell SG, Fiebach NH. Clinical epidemiology of nocturnal leg cramps in male veterans. Am J Med Sci 1997 313:210ŌĆō214. PMID: 9099150.


18. Jansen PH, Veenhuizen KC, Wesseling AI, de Boo T, Verbeek AL. Randomised controlled trial of hydroquinine in muscle cramps. Lancet 1997 349:528ŌĆō532. PMID: 9048790.


19. Man-Son-Hing M, Wells G, Lau A. Quinine for nocturnal leg cramps: a meta-analysis including unpublished data. J Gen Intern Med 1998 13:600ŌĆō606. PMID: 9754515.



20. Moll C, Mourre C, Lazdunski M, Ulrich J. Increase of sodium channels in demyelinated lesions of multiple sclerosis. Brain Res 1991 556:311ŌĆō316. PMID: 1657307.


21. Kavanaugh GJ, Svien HJ, Holman CB, Johnson RM. "Pseudoclaudication" syndrome produced by compression of the cauda equina. JAMA 1968 206:2477ŌĆō2481. PMID: 5754987.


23. Sugawara O, Atsuta Y, Iwahara T, Muramoto T, Watakabe M, Takemitsu Y. The effects of mechanical compression and hypoxia on nerve root and dorsal root ganglia, An analysis of ectopic firing using an in vitro model. Spine (Phila Pa 1976) 1996 21:2089ŌĆō2094. PMID: 8893432.


24. Kobayashi S, Uchida K, Yayama T, et al. Motor neuron involvement in experimental lumbar nerve root compression: a light and electron microscopic study. Spine (Phila Pa 1976) 2007 32:627ŌĆō634. PMID: 17413466.


25. Kiernan MC, Hart IK, Bostock H. Excitability properties of motor axons in patients with spontaneous motor unit activity. J Neurol Neurosurg Psychiatry 2001 70:56ŌĆō64. PMID: 11118248.



26. Coppin RJ, Wicke DM, Little PS. Managing nocturnal leg cramps--calf-stretching exercises and cessation of quinine treatment: a factorial randomised controlled trial. Br J Gen Pract 2005 55:186ŌĆō191. PMID: 15808033.


27. Roffe C, Sills S, Crome P, Jones P. Randomised, cross-over, placebo controlled trial of magnesium citrate in the treatment of chronic persistent leg cramps. Med Sci Monit 2002 8:CR326ŌĆōCR330. PMID: 12011773.

28. Mandal AK, Abernathy T, Nelluri SN, Stitzel V. Is quinine effective and safe in leg cramps? J Clin Pharmacol 1995 35:588ŌĆō593. PMID: 7665718.


29. Man-Son-Hing M, Wells G. Meta-analysis of efficacy of quinine for treatment of nocturnal leg cramps in elderly people. BMJ 1995 310:13ŌĆō17. PMID: 7827545.



30. Kim YS, Park SJ, Oh IS, Kwan JY. The clinical effect of gait load test in two level lumbar spinal stenosis. Asian Spine J 2009 3:96ŌĆō100. PMID: 20404954.



Table┬Ā3
Descriptive pattern of occurrence of the leg cramps, clinical features, activities of daily living and treatment received