 |
 |
- Search
| Asian Spine J > Volume 9(6); 2015 > Article |
Abstract
Overview of Literature
Few reports have documented potential complications related to the use of cervical laminoplasty plates.
Methods
Records and radiographs of consecutive plated laminoplasty patients of one academic surgeon were analyzed. Group 1 had screw back-out, defined as change in screw position, and group 2 did not.
Results
Forty-two patients (mean age, 56.9) underwent "open-door" cervical laminoplasty using 165 plates. Mean follow-up was 24 months (range, 12-49 months). Mean Nurick grade improved from 2.1 to 0.9 postoperatively. Cervical lordosis (C2-7) was 12.1° preoperatively and 10.0° postoperatively. Range-of-motion was 27.0° preoperatively and 23.4° postoperatively. Partial screw back-out was noted in 27 of 165 plates (16.4%) and in 34 of 660 screws (5.2%). Of the 34 screws, 27 (79.4%) were at either the most cranial (12/27, 44.4%) or the most caudal (15/27, 55.5%) level. Cranially, 11/12 screws (91.7%) had back-out. Caudally, 9/15 lateral mass screws (60.0%) backed-out versus 6 laminar screws (40.0%). Of the 22 patients with screw back-out, 15 (68.2%) occurred <3 months postoperative and 6 (27.3%) occurred 4-12 months postoperative. No statistical differences were found between group 1 and 2 for age, gender, preoperative and postoperative lordosis, focal sagittal alignment, range-of-motion, or Nurick grade. Despite screw backout in 22 patients, there were no plate dislodgements, laminoplasty closure, or neurological deterioration.
Conclusions
Although screw back-out may occur with the use of cervical laminoplasty plates, the use of these plates without a bone block appears to be safe and reliable. As screw back-out is most common at the cranial and caudal ends of the laminoplasty, we recommend using the maximum number of screws (typically 2 for the lateral mass and 2 for the spinous process) at these levels to secure the plate to the bone.
Laminoplasty is an accepted treatment for symptomatic cervical myelopathy resulting from spondylotic disease [12] and ossification of the posterior longitudinal ligament [3]. It avoids the surgical morbidity [456789101112] and the graft related complications [12710131415] associated with anterior cervical surgery and has become the treatment of choice for myelopathic diseases involving three or more cervical spinal segments [2716171819]. Since Hirabayashi et al. [3] first reported the result of open-door laminoplasty in 1977, the technique is commonly practiced in the United States and Europe [20].
In the original description, the open-door laminoplasty is kept open with a suture technique [3]. Sutures are placed at each level through the base of the spinous process and then through the zagapophyseal articular capsule and surrounding muscle fascia on the hinge side. Closure of the laminoplasty using suture technique was reported [23172122]. This prompted the development of a variety of methods using auto- or allograft [23], hydroxyapatite [2425], glass ceramic [26] and metal plates [20232427282930] to act as spacers to keep the lamina in the open position.
Park and Heller [30] in 2004 had published their technique using a custom-made mini titanium plate to keep the lamina open in the open-door cervical laminoplasty. Since then this plate (Ti-Mesh LP system plate, Medtronic Sofamor Danek, Memphis, TN, USA) has gained wide popularity among the spine surgeons (Fig. 1A). However few reports have documented the potential complications related to the use of the plate and the aim of the study is to describe any potential complication and the clinical observation of screw back-out in these laminoplasty plates.
A retrospective review of patients who had open-door laminoplasty were done. All consecutive patients who had undergone "open-door" cervical laminoplasty using Ti-Mesh LP laminoplasty plates (Medtronic Sofamor Danek) without a bone block by a single surgeon (KDR) at a single academic institution were identified. Patient clinical data was recorded with attention to preoperative patient age, gender, and neurological deficits based on Nurick grading [719]. Operative data and any complications were studied. Degree of cervical lordosis and range of cervical spinal motion were measured in both preoperative and postoperative plain radiographs. Patients were divided into two groups: those who had evidence of screw back-out from the plate (group 1) and those who did not (group 2). Screw back-out was defined as a change in screw position on serial radiographs. SSPSS ver. 20 (IBM Co., Armonk, NY, USA) was used for statistical analysis.
In our study, a total of 42 patients with a mean age of 56.9 years (range, 30-85 years) underwent "open-door" cervical laminoplasty using a total of 165 plates. There were 10 female and 32 male patients. The average operative time was 170 minutes (range, 75-240 minutes) with a 190 mL (range, 100-900 mL) estimated blood loss. The mean postoperative follow-up was 24 months (range, 12-49 months). The average Nurick grade improved from 2.1 preoperatively to 0.9 postoperatively. Cervical lordosis (measured from C2 to C7) was 12.1° preoperatively and 10.0° postoperatively. Cervical range of motion was 27.0° preoperatively and 23.4° postoperatively.
A partial screw back-out (group 1) occurred in 27 of 165 plates (16.4%) and in 34 of 660 screws (5.2%) postoperatively. Of the 34 screws, 27 (79.4%) were found at either the most cranial (12 of 27 screws [44.4%]) or the most caudal (15 of 27 screws [55.5%]) laminoplasty level. Cranially, 11 of 12 screws (91.7%) had evidence of backout from the lateral mass, whereas caudally, only 9 of 15 screws (60.0%) had back-out from the lateral mass with the remaining 6 screws (40.0%) having back-out from the spinous process (Fig. 2).
Of the 22 patients who had evidence of screw back-out, 15 (68.2%) had evidence of screw back-out within the first three months of surgery and 6 (27.3%) had evidence of screw back-out from 4 to 12 months following surgery. There was no change in any screw position after the first year of patient follow-up. No statistical differences were found between group 1 and group 2 with respect to patient age, gender, preoperative and postoperative cervical lordosis, focal sagittal alignment, range of motion, or Nurick grade. Despite evidence of screw back-out in 22 patients, there were no instances of plate dislodgement, laminoplasty closure, or neurological deterioration following surgery at the final patient follow-up.
The use of miniplates obtained from the cranial fixation systems to avoid closure of the open-door cervical laminoplasty was first described by Frank and Keenen [27] in 1994. Using computerized morphometric analysis, O'Brien et al. [29] had confirmed an average increase in cervical canal diameter to 11.6±1.2 mm or 105% in 10 myelopathic patients who underwent laminoplasty held by this plate. In their study, a straight 5-holes miniplate was bent into a "Z" configuration to allow for a one-hole fixation into the laminar and its corresponding lateral mass. Although the technique is effective, the "z" plate application is challenging as the plate often slips away from the bony surface. Park and Heller [30] had modified the 2 ends of the plate (Ti-Mesh LP system plate; Medtronic Sofamor Danek) to provide initial resistance to displacement of the plate-bone interface. This is achieved when the "mouth" of the plate accepts the cut edge of the lamina and the ventral prong on the lateral part of the plate catches the cut edge of the lateral mass along the gutter. This inherent plate-bone stability facilitates subsequent screw application. Also the plate is designed to allow a two-holes fixation on both of its ends to increase screw placement options and plate stability (Fig. 1B).
In the current study, 42 patients had undergone "opendoor" cervical laminoplasty using a total of 165 plates (Ti-Mesh LP system plate; Medtronic Sofamor Danek) and 660 screws with no bone block. In these patients, the average Nurick grade had improved from 2.1 preoperatively to 0.9 postoperatively. Cervical lordosis was 12.1° preoperatively and maintained as 10.0° postoperatively. The range-of-motion in the cervical spine was preserved from 27.0° preoperatively to 23.4° postoperatively. There was no restenosis from laminoplasty closure, plate dislodgment or neurological deterioration. These results fulfilled the aims of using laminoplasty plates to provide immediate postlaminoplasty stability in patients and allowing early neck mobilization without the risk of lamina closure in attempt to achieve better preservation of cervical motion and possible reduction of postoperative axial neck pain [30]. Similar results have been reported using various forms of laminoplasty plates.
Iwakura et al. [28] compared the postoperative results between 38 patients who underwent laminectomy and 32 patients with laminoplasty held with titanium miniplates. Post-laminectomy spinal deformity occurred in 5 (13%) patients and none in the laminoplasty group. The author concluded that laminoplasty with miniplates provided stability to the posterior cervical column and was a useful and safe technique. Deutsch et al. [20] reported the results of 5 patients who underwent laminoplasty held with the Ti-Mesh LP miniplates (Medtronic Sofamor Danek). There was no post-laminoplasty plate dislodgement and lamina closure in these patients. Postoperative cervical computed tomography (CT) demonstrated an average increase of sagittal canal diameter from 8 to 17 mm or 112%.
Despite the favorable clinical outcomes reported in the current study, radiologically partial screw back-out was noted in 16% of the plates and in 5% of all the screws. Interestingly 79% of the partial screw back-out occurred at either ends of the laminoplasty, of which 44% were found at the most cranial and 56% at the most caudal end. At the most cranial end of the laminoplasty 11 screws were found to have backed-out partially at the lateral mass and one screw at the lamina end of the plate. At the most caudal end of the laminoplasty 9 screws were found to have backed-out partially at the lateral mass and 6 screws at the lamina end of the plate. These results have not been previously reported in the literature.
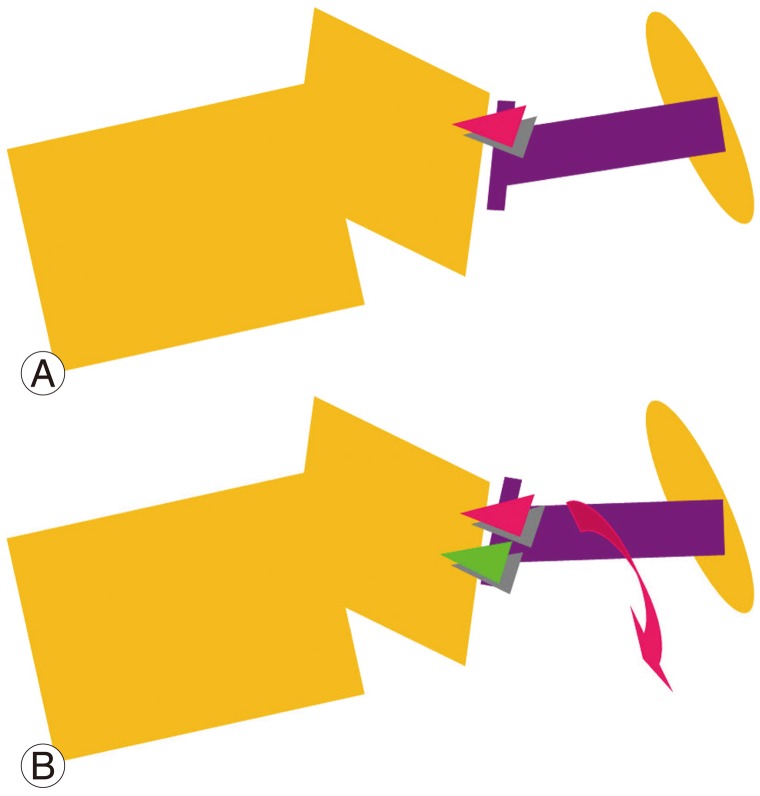
Statistical comparison between the patients with evidence of partial screw back-out (group 1) and those who did not (group 2) showed patient age, gender, pre- and post-laminoplasty Nurick grade, cervical lordosis, range of cervical motion and focal sagittal alignment at either ends of the laminoplasty were not risk factors for screw back-out. Screw back-out at either ends of the laminoplasty may be related to one or combinations of others factors. Firstly, judicial dissection at both ends of the laminoplasty to avoid damage of the semispinalis cervicis at the base of C2 and trapezium muscle insertion at C7 is required to prevent the development of post-laminoplasty kyphosis and axial neck pain; limited exposure and access are often found at both ends of the laminoplasty. This makes instrumentation and screw application at both ends of the laminoplasty more awkward with less ideal screw placement trajectory and possible increase fixation error when compared to screw insertion in the center of the laminoplasty. Evidence of increased screw back-out from the most cranial lateral mass compared to the lateral mass screw back-out at the caudal end of the laminoplasty further substantiated the concept of difficult access for screw fixation, as the most cranial lateral mass is found in the deepest part of the surgical field from the skin incision (Fig. 3). Secondly, failure to retighten the first screw after the application of the second screw at each end of the plate may cause the first screw to loosen. With the first screw in situ, the second screw drives the plate closer towards the bone while it is being tighten, this may increase the space between the first screw head- plate interface as the plate is driven closer towards the bone and moved relatively away from the first screw head (Fig. 4). Finally, the use of short screws with a 2.6 mm diameter and 5 mm in length as described in the original technique by Park and Heller [30] allows little room for screw fixation error. The use of a longer 7 mm screw may increase bony purchase and afford greater margin of technical error during screw application and that may result in less screw back-out as observed in the recent cases.
A limitation of the current study is its retrospective design which relies on data collection from past medical records. No records of practice of routine final tightening of all screws or the screw lengths being used could be found for the study. In addition it is not a routine practice to subject patient to a post-laminoplasty CT cervical scan and thus post laminoplasty spinal canal dimension analysis was not performed. Despite partial screw back-out was found radiologically with unknown significance, clinically this study has provided evidence of a favorable clinical outcome in patients who underwent open-door cervical laminoplasty with Ti-Mesh LP plates (Medtronic Sofamor Danek). There were no plate dislodgements or laminoplasty closures resulting in patient neurological deterioration found in the study.
Although screw back-out may occur with the use of cervical laminoplasty plates, the use of these plates without a bone block appears to be safe and reliable. Should one discover radiological evidence of partial screws back-out, these often result in no significant clinical problems. Majority (68%) of screw back-out occurred within the first three months of surgery and no further change in any screw position was found after the first year of patient follow-up. As screw back-out is most common at the cranial and caudal ends of the laminoplasty, we recommend using a maximum number of screws (typically 2 for the lateral mass and 2 for the spinous process) at these levels to secure the plate to the bone. The use of 7 mm long screws instead of 5 mm ones and the practice of retightening of all screws after the initial placement of the screws at the end of the operation may further reduce screw back-out from the plate.
Conflict of Interest
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
1. Riew KD, Sethi NS, Devney J, Goette K, Choi K. Complications of buttress plate stabilization of cervical corpectomy. Spine (Phila Pa 1976) 1999 24:2404–2410. PMID: 10586468.


2. Rhee JM, Riew KD. Evaluation and management of neck pain, radiculopathy, and myelopathy. Semin Spine Surg 2005 17:174–185.

3. Hirabayashi K, Toyama Y, Chiba K. Expansive laminoplasty for myelopathy in ossification of the longitudinal ligament. Clin Orthop Relat Res 1999 (359): 35–48. PMID: 10078127.


4. Apfelbaum RI, Kriskovich MD, Haller JR. On the incidence, cause, and prevention of recurrent laryngeal nerve palsies during anterior cervical spine surgery. Spine (Phila Pa 1976) 2000 25:2906–2912. PMID: 11074678.


5. Burke JP, Gertzen PC, Welch WC. Iatrogenic vertebral artery injury during anterior cervical spine surgery In: Proceedings of the 16th Annual Meeting North American Spine Society; 2001 Oct 31-Nov 3; Seattle, WA:
6. Clements DH, O'Leary PF. Anterior cervical discectomy and fusion. Spine (Phila Pa 1976) 1990 15:1023–1025. PMID: 2263966.


7. Edwards CC 2nd, Riew KD, Anderson PA, Hilibrand AS, Vaccaro AF. Cervical myelopathy: current diagnostic and treatment strategies. Spine J 2003 3:68–81. PMID: 14589250.


8. Emery SE, Smith MD, Bohlman HH. Upper-airway obstruction after multilevel cervical corpectomy for myelopathy. J Bone Joint Surg Am 1991 73:544–551. PMID: 2013593.


9. Heeneman H. Vocal cord paralysis following approaches to the anterior cervical spine. Laryngoscope 1973 83:17–21. PMID: 4683910.


10. Hilibrand AS, Carlson GD, Palumbo MA, Jones PK, Bohlman HH. Radiculopathy and myelopathy at segments adjacent to the site of a previous anterior cervical arthrodesis. J Bone Joint Surg Am 1999 81:519–528. PMID: 10225797.


11. Riew KD, Won DS, Calvert G, et al. Parameters for maintaining intubation postoperatively following anterior cervical procedures In: Proceedings of the 16th Annual Meeting North American Spine Society; 2001 Oct 31-Nov 3; Seattle, WA.
12. Riley LH 3rd, Skolasky RL, Albert TJ, Vaccaro AR, Heller JG. Dysphagia after anterior cervical decompression and fusion: prevalence and risk factors from a longitudinal cohort study. Spine (Phila Pa 1976) 2005 30:2564–2569. PMID: 16284596.


13. Belanger TA, Roh JS, Hanks SE, Kang JD, Emery SE, Bohlman HH. Ossification of the posterior longitudinal ligament. Results of anterior cervical decompression and arthrodesis in sixty-one North American patients. J Bone Joint Surg Am 2005 87:610–615. PMID: 15741630.


14. Bolesta MJ, Rechtine GR 2nd, Chrin AM. Three- and four-level anterior cervical discectomy and fusion with plate fixation: a prospective study. Spine (Phila Pa 1976) 2000 25:2040–2044. PMID: 10954634.


15. Emery SE, Fisher JR, Bohlman HH. Three-level anterior cervical discectomy and fusion: radiographic and clinical results. Spine (Phila Pa 1976) 1997 22:2622–2624. PMID: 9399447.


16. Epstein N. Posterior approaches in the management of cervical spondylosis and ossification of the posterior longitudinal ligament. Surg Neurol 2002 58:194–207. PMID: 12480213.


17. Kawakami M, Tamaki T, Ando M, Yamada H, Yoshida M. Relationships between sagittal alignment of the cervical spine and morphology of the spinal cord and clinical outcomes in patients with cervical spondylotic myelopathy treated with expansive laminoplasty. J Spinal Disord Tech 2002 15:391–397. PMID: 12394663.


18. Rao RD, Gourab K, David KS. Operative treatment of cervical spondylotic myelopathy. J Bone Joint Surg Am 2006 88:1619–1640. PMID: 16818991.


19. Yonenobu K, Oda T. Posterior approach to the degenerative cervical spine. Eur Spine J 2003 12(Suppl 2): S195–S201. PMID: 12942354.



20. Deutsch H, Mummaneni PV, Rodts GE, Haid RW. Posterior cervical laminoplasty using a new plating system: technical note. J Spinal Disord Tech 2004 17:317–320. PMID: 15280762.


21. Hosono N, Sakaura H, Mukai Y, Ishii T, Yoshikawa H. En bloc laminoplasty without dissection of paraspinal muscles. J Neurosurg Spine 2005 3:29–33. PMID: 16122019.


22. Itoh T, Tsuji H. Technical improvements and results of laminoplasty for compressive myelopathy in the cervical spine. Spine (Phila Pa 1976) 1985 10:729–736. PMID: 3909451.


23. Shaffrey CI, Wiggins GC, Piccirilli CB, Young JN, Lovell LR. Modified open-door laminoplasty for treatment of neurological deficits in younger patients with congenital spinal stenosis: analysis of clinical and radiographic data. J Neurosurg 1999 90:170–177. PMID: 10199245.

24. Goto T, Ohata K, Takami T, et al. Hydroxyapatite laminar spacers and titanium miniplates in cervical laminoplasty. J Neurosurg 2002 97:323–329. PMID: 12408386.


25. Nakano K, Harata S, Suetsuna F, Araki T, Itoh J. Spinous process-splitting laminoplasty using hydroxyapatite spinous process spacer. Spine (Phila Pa 1976) 1992 17(3 Suppl): S41–S43. PMID: 1314432.


26. Kamo Y, Takemitsu Y, Hamada O, et al. Cervical laminoplasty by splitting the spinous process using AW glass-ceramic laminar spacer. Rinsho Seikeigeka 1992 10:1115–1122.
27. Frank E, Keenen TL. A technique for cervical laminoplasty using mini plates. Br J Neurosurg 1994 8:197–199. PMID: 7917092.


28. Iwakura M, Yamamoto K, Nagashima T, Tamaki N. Surgical technique and long-term follow-up of laminoplasty using titanium miniplates. No Shinkei Geka 1999 27:525–531. PMID: 10396735.

29. O'Brien MF, Peterson D, Casey ATH, Crockard HA. A novel technique for laminoplasty augmentation of spinal canal area using titanium miniplate stabilization: a computerized morphometric analysis. Spine 1996 21:474–483. PMID: 8658252.


30. Park AE, Heller JG. Cervical laminoplasty: use of a novel titanium plate to maintain canal expansion: surgical technique. J Spinal Disord Tech 2004 17:265–271. PMID: 15280753.


Fig. 1
(A, B) This plate provides inherent bone-plate stability upon application to the opened lamina, and makes screw fixation easier. The "mouth" of plate accepts the cut edge of lamina and the ventral prong on the lateral part of plate catches the cut edge of the lateral mass. 2-hole screw fixation is allowed at each end of the plate when compared to other laminoplasty plate system.
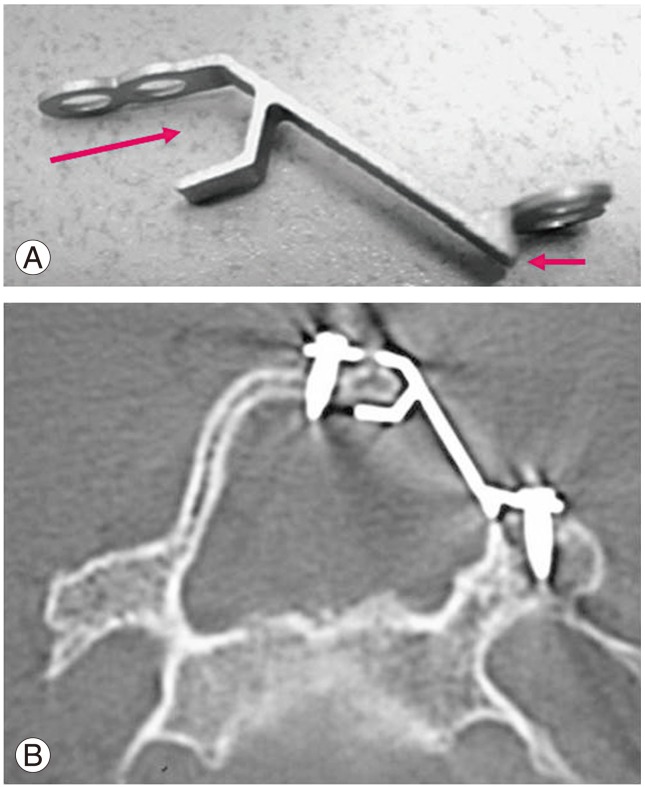
Fig. 2
This radiograph shows screw back-out at the lateral mass at both cranial and caudal ends of the open-door laminoplasty.

Fig. 3
Limited laminoplasty exposure (red line) was made to preserve semispinalis cervics at C2 and trapezium at C7. This exposure reduced postlaminoplasty complications but may limit the ideal screw insertion trajectory as shown by the blue lines of screw trajectories. This may lead to suboptimal screw purchase and lead to screw back-out.
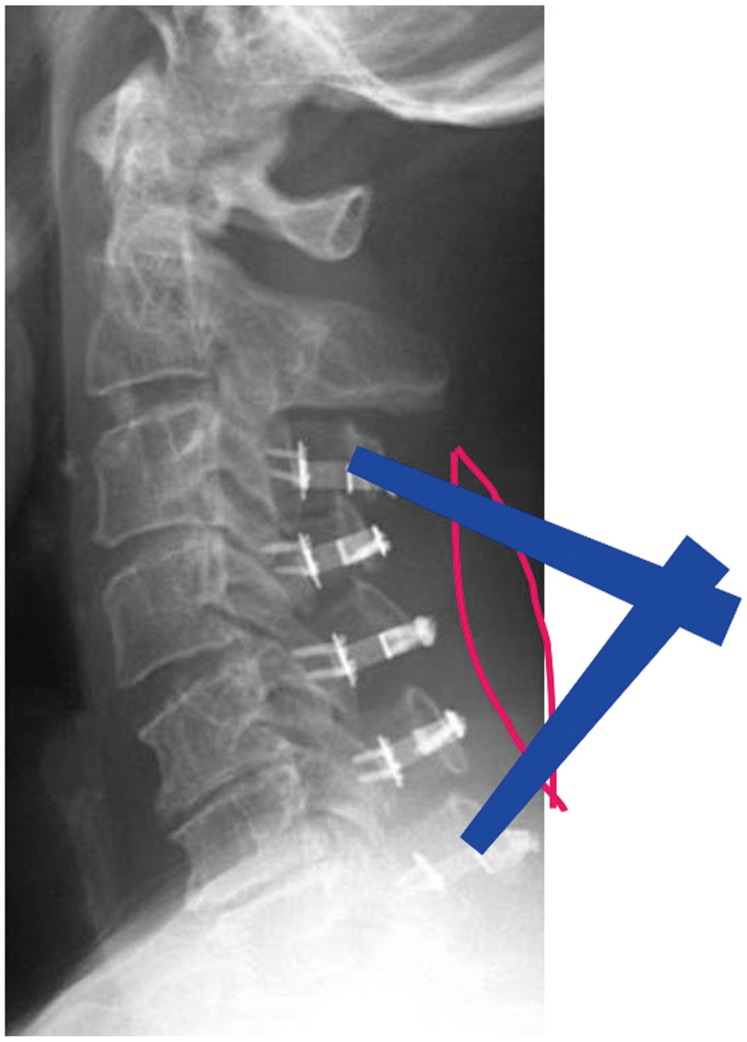
Fig. 4
(A) Insertion of the first screw brings the plate closer to the bone. (B) Insertion of the second screw may bring lower end of the plate closer to bone compared to the upper end of the plate where the first screw was inserted. This indirectly loosens the first screw if the first screw is not being re-tightened after the insertion of the second screw.
- TOOLS






