 |
 |
- Search
| Asian Spine J > Volume 14(4); 2020 > Article |
|
Abstract
Overview of Literature
C1 laminectomy has been the standard procedure for decompression at the C1 level. However, there have been some reports of trouble cases after C1 laminectomy. C1 laminoplasty might be superior to C1 laminectomy with regard to maintaining the original C1 anatomical shape, preventing compression from the posterior soft tissue, and ensuring an adequate bone-grafting site around the C1 posterior part if additional salvage fusion surgery is necessary afterward.
Methods
Seven patients with spinal cord compression without obvious segmental instability at the C1/2 level treated by C1 laminoplasty were included. The indication of C1 laminoplasty was same as that of C1 laminectomy. C1 laminoplasty was performed in the same way as subaxial double-door laminoplasty. The imaging findings were evaluated using X-ray, computed tomography, and magnetic resonance imaging. The clinical results were evaluated using the Japanese Orthopaedic Association (JOA) Cervical Myelopathy Evaluation Questionnaire (JOACMEQ) and JOA score. Peri- and postoperative complications were also investigated.
Results
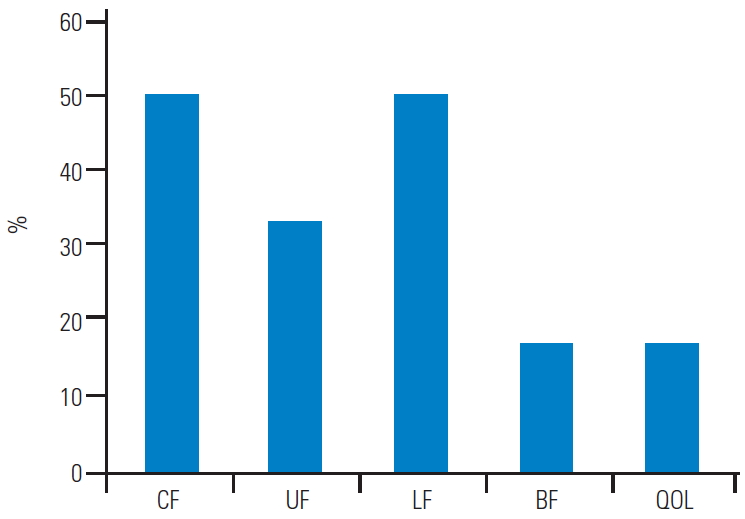
No patient showed increased C1/2 segmental instability after the surgery. The mean pre- and postoperative JOA scores were 8.6 and 11.7, respectively. The mean recovery rate was 40.2%. The effective rate in the JOACMEQ was 50% for the cervical spine function, 33% for the upper extremity function, 50% for the lower extremity function, 17% for the bladder function, and 17% for the quality of life. No major complication that seemed to be unique to C1 laminoplasty was observed over a period of about 4 years follow-up.
C1 laminectomy has been the standard procedure for decompression at the C1 level [1,2]. Discussion has been had regarding whether fusion surgery or decompression surgery is a better treatment for compressive myelopathy with pseudotumor at the upper cervical level. However, the methodology of decompression surgery has hardly been discussed. Recently, there have been some reports of spontaneous anterior arch fracture after C1 laminectomy [3-8]. Anterior arch fragility following C1 laminectomy has also been recognized using a finite element analysis [6]. In addition, a case of dynamic paraspinal muscle impingement causing acute hemiplegia after C1 laminectomy was recently reported [9]. Historically, cervical laminoplasty has been developed to avoid some issues after cervical laminectomy, such as laminectomy scar membrane at the middle and lower cervical levels. Considering the historical background and based on the findings of the previous reports, it may therefore be better to change C1 laminectomy to another method, such as C1 laminoplasty.
We have performed C1 laminoplasty without fusion in some patients with compressive myelopathy without obvious instability at the C1 level. C1 laminoplasty might be superior to C1 laminectomy with regard to maintaining the original C1 anatomical shape, preventing compression from the posterior by muscle impingement, and ensuring an adequate bone-grafting site around the C1 posterior part if additional salvage fusion surgery is necessary afterward.
The purpose of this study is to evaluate the radiographic and clinical results of C1 laminoplasty without fusion for patients with compressive myelopathy without obvious instability at the C1 level.
All the procedures performed in studies involving human participants were in accordance with the ethical standards of the institutional and/or national research committee and with the 1964 Helsinki declaration and its later amendments or comparable ethical standards. Informed consent was obtained from all the individual participants included in this study. This study was approved by the ethics committee of Kyushu University Hospital (IRB approval no., 28-324).
A total of eight patients (seven males, one female) who underwent C1 laminoplasty between January 2010 and March 2018 were retrospectively reviewed. The indications of C1 laminoplasty, same as those of C1 laminectomy, are summarized subsequently. Compressive myelopathy at the C1 level was confirmed using magnetic resonance imaging (MRI). Obvious instability, which was defined as movement exceeding 3 mm at the atlas-dens interval (ADI), was denied using dynamic lateral X-ray. In this series, C1 laminoplasty was performed on patients who satisfied the abovementioned points. Contraindications of C1 laminoplasty are patients with great instability, bone anomaly, and anomaly of the vertebral artery.
C1 laminoplasty was performed as follows: First, we expose the C1 posterior arch, perform fenestration at OŌĆōC1 and C1ŌĆō2, pass through a T-saw under the C1 posterior arch in case using T-saw, cut the center of the posterior arch using a T-saw (six cases) or high-speed drill (two cases), make gutters at the bilateral sides using high-speed drill with 3 mm diamond bar, open the posterior arch, and finally piece together the split arches using a hydroxyapatite (HA) spacer with suture (Fig. 1). The C1 posterior arch has much cortical bone than the subaxial laminae. It is difficult to make gutters; so, care must be taken not to cause incidental fracture. In case with multiple stenosis at subaxial laminae, double-door laminoplasty involving placement of HA spacer was performed.
The mean age, preoperative diagnosis, operated level, estimated blood loss (EBL), operation time (OT), segmental instability at the C1/2 before and after surgery, bone union of gutters, anteroposterior (AP) diameter of spinal canal at the C1 level after surgery, clinical results, and follow-up (FU) period were reviewed. Patients with less than 1 year of FU were excluded from this study. The thickness of the pseudotumor was measured before and after surgery, and the difference in the size was calculated. Peri- and postoperative complications were also investigated. Radiographic evaluation was performed at 1 year or later after the surgery. Clinical evaluation was performed at preoperation, 1 year after the surgery, and final FU. If revision surgery was needed, that time was considered as the final FU.
Instability of the C1/2 was evaluated using dynamic lateral X-ray on the picture archiving and communication systems before and after surgery. Segmental instability was defined as movement exceeding 3 mm at the ADI [8]. Bone union of the gutters and that between the HA spacer and posterior elements were assessed using computed tomography (CT) during FU. Bone union was defined as the bridging of the gap of the gutter with time (Fig. 2). The AP diameter of the spinal canal at the C1 level was measured between the posterior surface of the dens and the anterior surface of the HA spacer after surgery using CT (Fig. 3). Clinical results were evaluated using the Japanese Orthopaedic Association (JOA) score [10] and the HirabayashiŌĆÖs recovery rate [11]. In addition, the JOA Cervical Myelopathy Evaluation Questionnaire (JOACMEQ) was used to evaluate the clinical results as patient-based outcomes in patients with complete data [12]. The JOACMEQ has several domains, including cervical spine function, upper extremity function, lower extremity function, bladder function, and quality of life. The effectiveness of the treatment based on the JOACMEQ was judged following the methods determined by the JOA (Table 1).
A total of seven patients (six males, one female) who underwent C1 laminoplasty were ultimately included. One patient with less than one year FU was excluded. The mean age of the patients at the time of surgery was 72 years old. The mean FU period after surgery was 50 months (range, 22ŌĆō78 months). Cervical ossification of the posterior longitudinal ligament was demonstrated in one patient, and cervical spondylotic myelopathy was demonstrated in six patients. Atlantoaxial anterior subluxation and retroodontoid pseudotumor were revealed in five patients. There were some overlaps in the diagnoses. The treated level was as follows: C1ŌĆō6 in two cases, C1 and C3ŌĆō6 in three cases, C1 and C3ŌĆō5 in one case, and C1 in one case. The mean EBL was 269 g (range, 40ŌĆō734 g). The mean OT was 211 minutes (range, 163ŌĆō270 minutes). No patient showed an obvious increase in C1/2 segmental instability after the surgery.
Adequate decompression was observed in all patients using CT, and the mean C1-level spinal column AP diameter was 23 mm. Sufficient decompression was also confirmed in MRI (Fig. 4). Bone union of the gutters was accomplished in five of seven cases during FU (Table 2). For the remaining two patients, the gutter on one side was fused. The mean thickness of the pseudotumor before and after surgery was 8.7 mm and 9.3 mm, respectively.
The mean JOA scores before surgery, one year after surgery, and final FU were 8.6, 12.2, and 11.7, respectively. The mean recovery rates at 1 year after surgery and final FU were 42.9% and 40.2%, respectively (Table 3). According to the JOA evaluation system for the effectiveness of treatment as determined by the JOACMEQ, the effective rate was 50% for the cervical spine function, 33% for the upper extremity function, 50% for the lower extremity function, 17% for the bladder function, and 17% for the quality of life (Fig. 5). The original anatomical shape as the bone loop of C1 was maintained through contact with the HA spacer in all cases; however, apparent bone union between the HA spacer and posterior elements could not be confirmed. There were no major peri- or postoperative complications that seemed to be unique to C1 laminoplasty during the FU.
One patient required additional fusion surgery (Magerl and Brooks procedure) due to neurological deterioration caused by an increase in the size of the pseudotumor at 22 months after C1 laminoplasty. The secureness of an adequate bone-grafting site around C1 was confirmed during salvage surgery. Four years have passed since salvage fusion surgery, and the patient has acquired solid bone union and is living well.
We investigated the radiographic and clinical results of C1 laminoplasty for the patients with compressive myelopathy at the C1 level. Though one case required revision surgery, our results indicated that C1 laminoplasty might be a useful alternative procedure to C1 laminectomy based on the middle-term FU.
Generally, treatment for C1 compressive myelopathy is considered as fusion with instrumentation surgery, decompression surgery without fusion, or decompression and fusion with instrumentation surgery, depending on the condition of the patients. Most patients with instability at the C1/2 level are usually treated by fusion surgery with or without decompression. However, fusion surgery for patients without instability at the C1/2 level is controversial [2,13,14].
Previous reports have recommended fusion surgery as the first choice for retroodontoid pseudotumor causing myelopathy [14-17]. However, C1 laminectomy without fusion has been reported to be a good procedure for patients without instability at the C1/2 level [1,2]. In addition, C1 laminoplasty has also been reported as a good procedure for patients with cervical myelopathy associated with retroodontoid pseudotumor without obvious C1ŌĆō2 instability [13]. Decompression procedures, including laminectomy and laminoplasty, have some benefits over fusion surgery, such as a maintained range of motion, a reduced risk of vertebral artery injury, and absence of pain at the site of bone graft harvest. C1 laminoplasty is performed instead of C1 laminectomy whenever possible in our institution for patients with compressive myelopathy at the C1 level without obvious instability.
In this study, five patients had retroodontoid pseudotumor. One of them needed additional fusion surgery during FU due to neurological deterioration caused by an increase in the size of the retroodontoid pseudotumor. This patient showed pre-existing bone union of C2/3 at the first surgery. The size of the retroodontoid pseudotumor might have increased due to the mechanical load applied to the adjacent level. However, no apparent increase in the size of the retroodontoid pseudotumor was observed in the other four patients. The clinical results of these patients improved and maintained based on the JOA scores. C1 laminoplasty may therefore be suitable as a decompression procedure. However, a previous report described retroodontoid pseudotumor with myelopathy in a diffuse idiopathic skeletal hyperostosis patient with decreased cervical mobility [18]. Even if there is no obvious instability at the C1/2 level, close attention should be paid in patients with pre-existing subaxial ankylosis.
C1 laminoplasty might provide adequate decompression as that of laminectomy. Previous reports have found that the normal AP diameter at the level of the atlas ranges from 16 to 20 mm [19]. In this study, the mean canal AP diameter after C1 laminoplasty was 23 mm, suggesting this procedure achieves adequate decompression at the level of the atlas.
C1 laminoplasty might have some benefits over laminectomy. Recently, a few cases of spontaneous C1 anterior arch fracture due to C1 laminectomy without obvious trauma were reported [1-6]. Most of these patients complained of neck pain. Four of them underwent fusion surgery, two required C1/2 or C1ŌĆō3 fusion, another two required O-C fusion, and one underwent the infusion of bone morphogenetic protein-2 at the fracture site followed by the placement of a halo vest for 3 months. While most cases were treated conservatively using a neck collar, if surgery was required after C1 laminectomy, then all such patients required fusion surgery. Unfortunately, one case in the current series underwent reoperation with fusion surgery using the Magerl technique. An adequate bone-grafting site at the C1 posterior arch was observed intraoperatively, and the patient has acquired solid bone union after revision surgery. C1 laminoplasty might therefore be superior to laminectomy due to the fact that it provides an adequate bone-grafting site. This merit might lead to successful salvage fusion surgery. Even in cases of primary fusion surgery, various methods for obtaining an adequate bone-grafting site have been reported, such as C1 domelike laminotomy, posterior C1ŌĆō2 polyaxial screwŌĆōrod fixation [20], and C1 laminoplasty with spacer and titanium miniplate screw fixation [21]. C1 laminoplasty is a simple and useful decompression procedure for securing an adequate bone-grafting site if subsequent additional salvage fusion surgery is necessary.
The incidence and risk factors of anterior arch fracture of the atlas following C1 laminectomy were recently reported [7]. In that study, the authors mentioned that the anterior arch fracture after C1 laminectomy was not uncommon (14.2%) and a large inferior facet angle and the presence of subaxial ankylosis were risk factors. Based on the findings of the patients who underwent reoperation in our series and previously reported data [7], fusion surgery might be better than decompression surgery for patients with subaxial ankylosis and/or large inferior facet angle. Shimizu et al. [6] suggested that C1 laminoplasty may be a prophylactic surgical intervention for anterior arch fracture. In the case of elderly patients with low activity concomitant to small inferior facet angle, C1 laminoplasty might be an option. To obtain further information regarding the association between C1 laminoplasty and prophylaxis of spontaneous anterior arch fracture, a larger number of cases and a biomechanical study similar to that conducted by Shimizu et al. [6] are needed.
Several limitations associated with this study warrant mention. First, this study examined a small number of cases. Thus, it is necessary to accumulate cases in the future. Second, this study was only an observational study. Hence, a comparative study with C1 laminectomy should be done.
C1 laminoplasty can obtain an adequate bone-grafting site around the C1 posterior part with HA spacer and suture without any screw or miniplate. This fact was confirmed in the case of reoperation in this series. In addition, no case of dynamic paraspinal muscle impingement causing neurological deterioration like that in the past literature was found in this series [9]. Consequently, C1 laminoplasty is a simple and better decompression procedure with possibilities and usefulness to replace C1 laminectomy in that it can prevent compression from the posterior tissue and obtain an adequate bone-grafting site around the C1 posterior part.
Fig.┬Ā1.
The surgical procedures of C1 laminoplasty. (A) Exposure and cutting the laminar. (B) Making the gutter. (C) Splitting the laminar. (D) Piece together using a hydroxyapatite spacer.

Fig.┬Ā3.
The anteroposterior diameter of the spinal canal at the C1 level was measured between the posterior surface of the dens and the anterior surface of the hydroxyapatite spacer after the surgery as indicated by the white arrow.
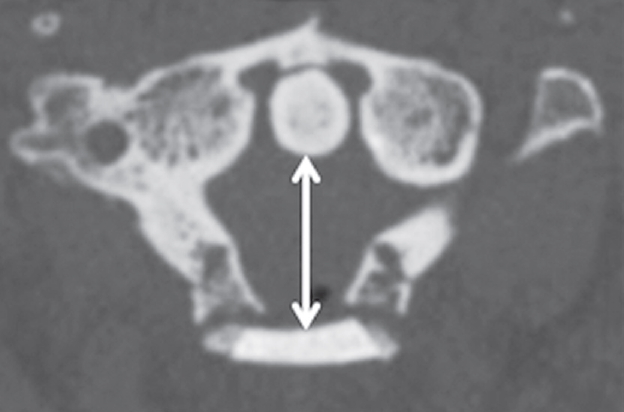
Fig.┬Ā4.
(A, B) MRI compared before and after the surgery. Sufficient decompression was confirmed by MRI after the surgery. MRI, magnetic resonance imaging.
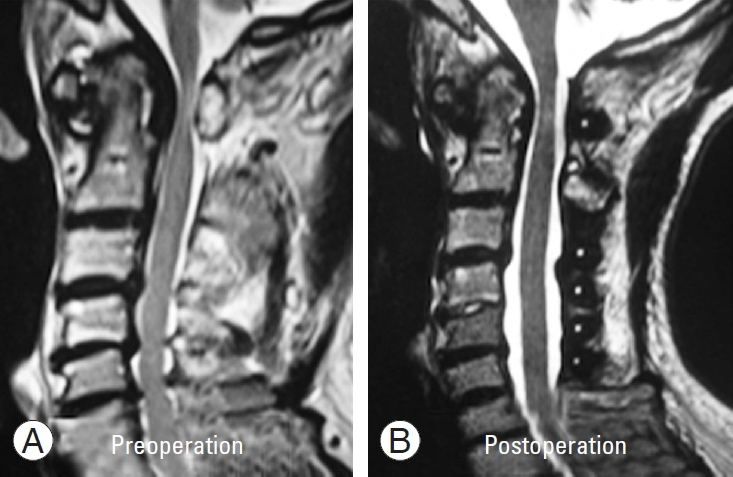
Fig.┬Ā5.
The therapeutic effective rate calculated according to Table 1. The therapeutic effective rate of the BF and QOL tended to be lower than those of the CF, UF, or LF. CF, cervical spine function; UF, upper extremity function; LF, lower extremity function; BF, bladder function; QOL, quality of life.
Table┬Ā1.
Therapeutic effect of treatment
Table┬Ā2.
Summary of the cases in this study
Table┬Ā3.
The JOA score and recovery rate of the patients
Recovery rate=(postoperative JOA scoreŌĆōpreoperative JOA score)/(17a)ŌĆōpreoperative JOA score)├Ś100%.
JOA, Japanese Orthopaedic Association; FU, follow-up.
References
1. Takemoto M, Neo M, Fujibayashi S, et al. Clinical and radiographic outcomes of C1 laminectomy without fusion in patients with cervical myelopathy that is associated with a retro-odontoid pseudotumor. Clin Spine Surg 2016 29:E514ŌĆō21.


2. Kakutani K, Doita M, Yoshikawa M, et al. C1 laminectomy for retro-odontoid pseudotumor without atlantoaxial subluxation: review of seven consecutive cases. Eur Spine J 2013 22:1119ŌĆō26.




3. OŌĆÖShaughnessy BA, Salehi SA, Ali S, Liu JC. Anterior atlas fracture following suboccipital decompression for Chiari I malformation: report of two cases. J Neurosurg Spine 2004 1:137ŌĆō40.


4. Hirano Y, Sugawara A, Mizuno J, Takeda M, Watanabe K, Ogasawara K. Spontaneous C1 anterior arch fracture as a postoperative complication of foramen magnum decompression for Chiari malformation type 1. Surg Neurol Int 2011 2:138.



5. Baghdassarian A, Piatt JH Jr, Giordano K. Fracture of the anterior arch of atlas after minor trauma of the immature spine postlaminectomy. Pediatr Emerg Care 2014 30:340ŌĆō2.


6. Shimizu T, Otsuki B, Fujibayashi S, et al. Spontaneous anterior arch fracture of the atlas following C1 laminectomy without fusion: a report of three cases and finite element analysis. J Orthop Sci 2016 21:306ŌĆō15.


7. Shimizu T, Otsuki B, Fujibayashi S, et al. Incidence and risk factors of anterior arch fracture of the atlas following C1 laminectomy without fusion. Spine (Phila Pa 1976) 2018 43:667ŌĆō74.


8. Allam E, Zhou Y. Bipartite atlas or Jefferson fracture?: a case series and literature review. Spine (Phila Pa 1976) 2015 40:E661ŌĆō4.


9. Notani N, Miyazaki M, Yoshiiwa T, Ishihara T, Kanezaki S, Tsumura H. Dynamic paraspinal muscle impingement causing acute hemiplegia after C1 posterior arch laminectomy: a case report. Medicine (Baltimore) 2017 96:e9264.



10. Japanese Orthopaedic Association. Scoring system for cervical myelopathy. J Jpn Orthop Assoc 1994 68:490ŌĆō530.
11. Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976) 1981 6:354ŌĆō64.


12. Fukui M, Chiba K, Kawakami M, et al. An outcome measure for patients with cervical myelopathy: Japanese Orthopaedic Association Cervical Myelopathy Evaluation Questionnaire (JOACMEQ): part 1. J Orthop Sci 2007 12:227ŌĆō40.



13. Suetsuna F, Narita H, Ono A, Ohishi H. Regression of retroodontoid pseudotumors following C-1 laminoplasty: report of three cases. J Neurosurg Spine 2006 5:455ŌĆō60.


14. Chikuda H, Seichi A, Takeshita K, et al. Radiographic analysis of the cervical spine in patients with retroodontoid pseudotumors. Spine (Phila Pa 1976) 2009 34:E110ŌĆō4.


15. Sono T, Onishi E, Matsushita M. Radiographic risk factors and surgical outcomes for retroodontoid pseudotumors. J Spinal Disord Tech 2014 27:E193ŌĆō8.


16. Yamaguchi I, Shibuya S, Arima N, Oka S, Kanda Y, Yamamoto T. Remarkable reduction or disappearance of retroodontoid pseudotumors after occipitocervical fusion: report of three cases. J Neurosurg Spine 2006 5:156ŌĆō60.


17. Jun BY. Complete reduction of retro-odontoid soft tissue mass in os odontoideum following the posterior C1-C2 tranarticular screw fixation. Spine (Phila Pa 1976) 1999 24:1961ŌĆō4.


18. Jun BY, Yoon KJ, Crockard A. Retro-odontoid pseudotumor in diffuse idiopathic skeletal hyperostosis. Spine (Phila Pa 1976) 2002 27:E266ŌĆō70.


19. Sawada H, Akiguchi I, Fukuyama H, Kameyama M, Koyama T. Marked canal stenosis at the level of the atlas. Neuroradiology 1989 31:346ŌĆō8.











