 |
 |
- Search
| Asian Spine J > Volume 16(5); 2022 > Article |
|
Abstract
Purpose
Overview of Literature
Methods
Results
Notes
Author Contributions
Yasuaki Imajo gathered and analyzed data. Norihiro Nishida, Masahiro Funaba, Yuji Nagao, and Hidenori Suzuki gathered data. Takashi Sakai was an advisor. All authors read and approved the final manuscript.
Acknowledgments
Fig.┬Ā1
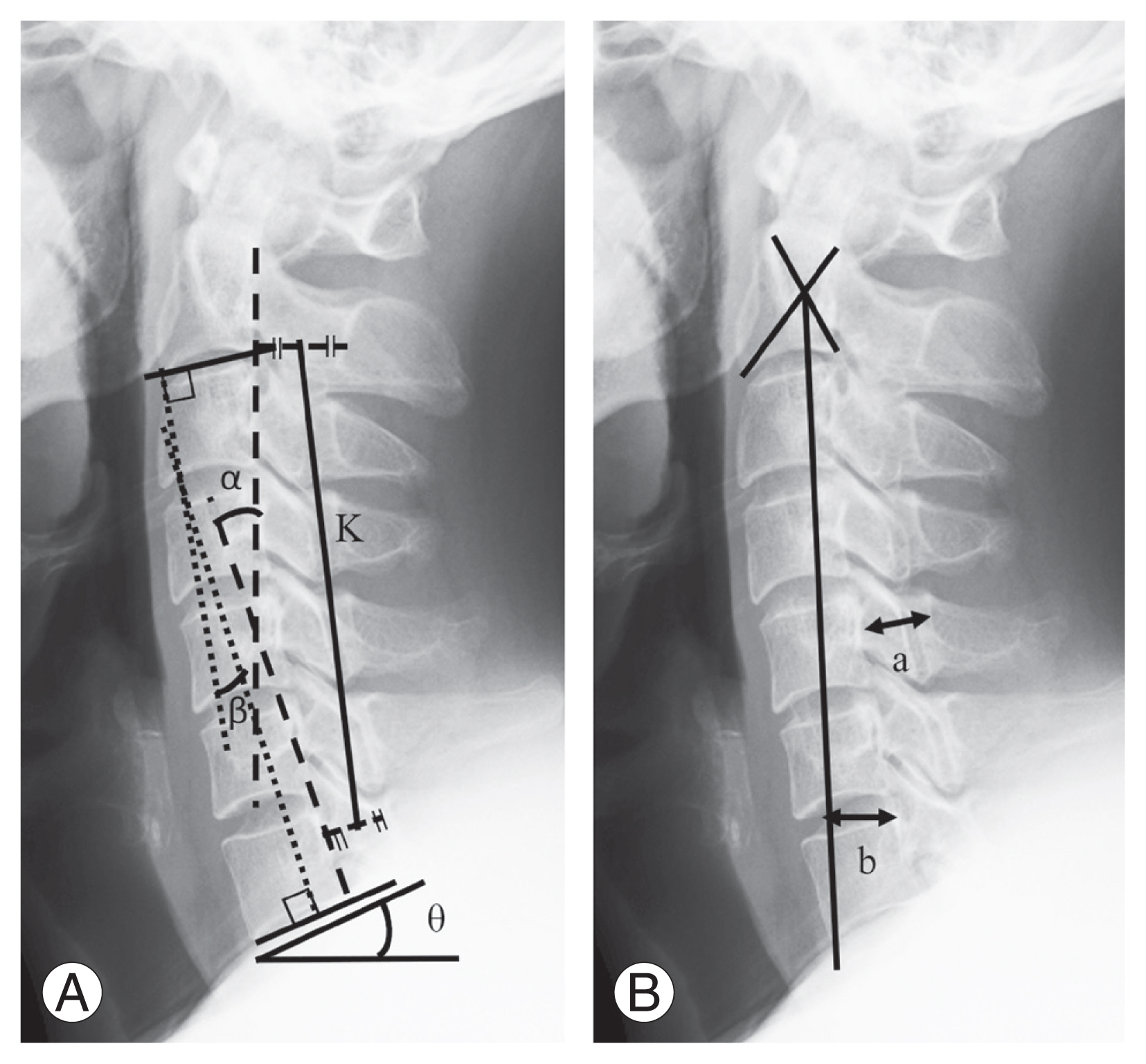
Fig.┬Ā2
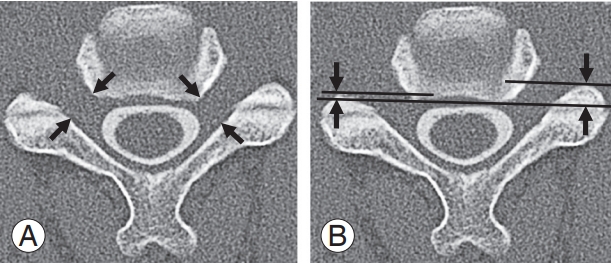
Fig.┬Ā3
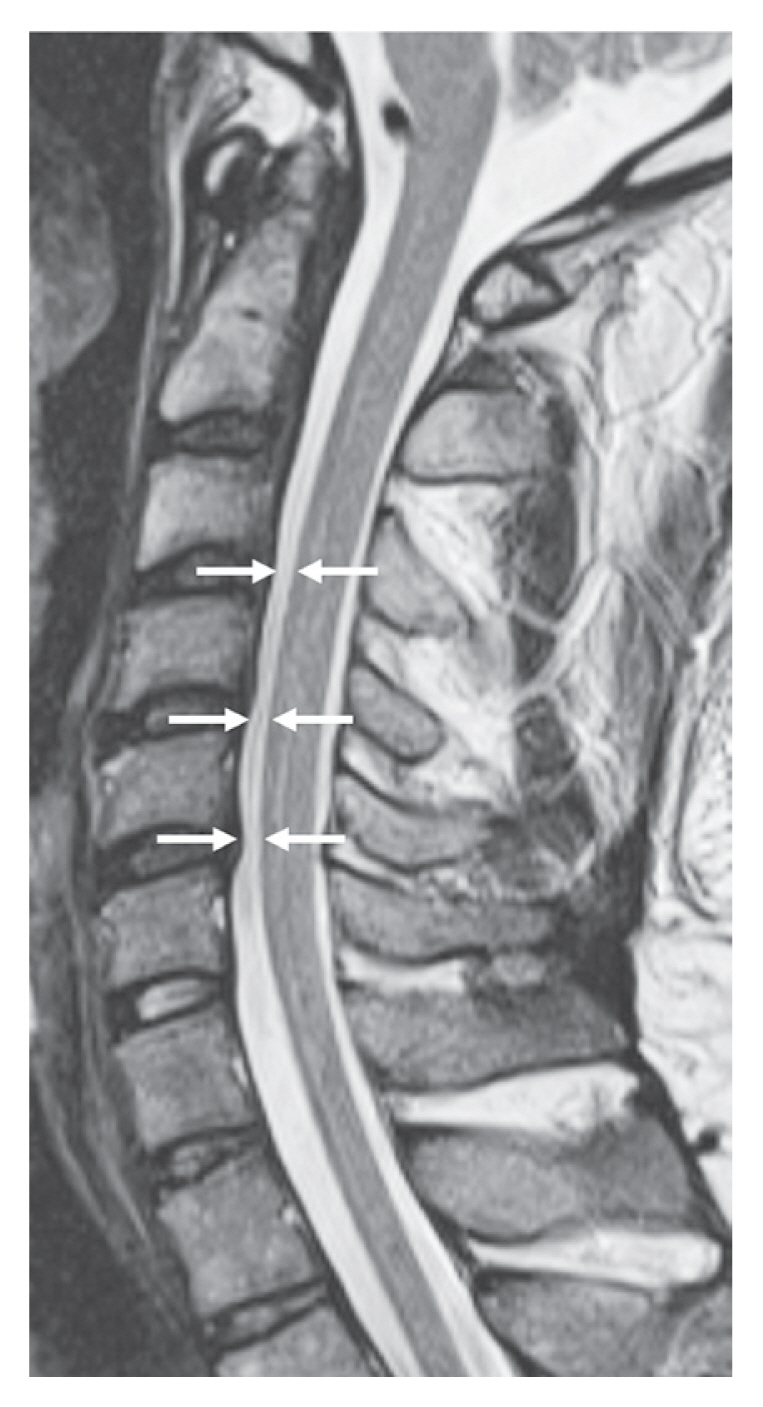
Table┬Ā1
| Variable | Definitions |
|---|---|
| ╬▒ | The angle between parallel lines to the posterior surface of the C2 and C7 vertebral bodies. |
| ╬▓ | The angle between the C2 and C7 lower endplates. |
| SVA | The distance between the C2 plumb line and the posterior superior endplate of C7. |
| T1 slope | The angle between the horizontal plane and the T1 upper endplate. |
| C5 canal | The diameter of the canal at the C5 vertebral level. |
| KŌĆōline | A straight line that connects the midpoints of the spinal canal at C2 and C7 |
| ╬│ | The intervertebral range at the C4ŌĆōC5 intervertebral levels was assessed using lateral radiographs in flexion and extension positions. |
| ╬┤ | The intervertebral range at the and C5ŌĆōC6 intervertebral levels was assessed using lateral radiographs in flexion and extension positions. |
Table┬Ā2
Table┬Ā3
| Variable | Anterior and posterior approach | Anterior approach | ||||
|---|---|---|---|---|---|---|
|
|
|
|||||
| Group1 (n=9) | Group 2 (n=51) | p-value | Group 1 (n=5) | Group 2 (n=28) | p-value | |
| Plain radiography | ||||||
|
|
||||||
| ŌĆā╬▒ (┬░) | 10.3┬▒10.4 | 10.4┬▒12.7 | 0.98 | 6.6┬▒12.1 | 9.3┬▒12.5 | 0.66 |
|
|
||||||
| ŌĆā╬▓ (┬░) | 12.3┬▒12.2 | 12.1┬▒14.6 | 0.97 | 6.6┬▒11.9 | 10.9┬▒13.8 | 0.52 |
|
|
||||||
| ŌĆāAlignment | 0.21 | |||||
|
|
||||||
| ŌĆāŌĆāStraight | 0 of 9 | 2 of 50 | 0.16 | 0 of 5 | 1 of 28 | |
|
|
||||||
| ŌĆāŌĆāLordosis | 7 | 29 | 3 | 15 | ||
|
|
||||||
| ŌĆāŌĆāKyphosis | 0 | 17 | 0 | 11 | ||
|
|
||||||
| ŌĆāŌĆāSigmoid | 2 | 2 | 2 | 1 | ||
|
|
||||||
| ŌĆāKŌĆōline ( ŌłÆ ) | 1 | 9 | 1.00 | 1 | 6 | 1.00 |
|
|
||||||
| ŌĆāPre C2ŌĆōC7 SVA (mm) | 24.1┬▒9.3 | 21.3┬▒10.6 | 0.48 | 19.8┬▒10.2 | 21.6┬▒11.0 | 0.72 |
|
|
||||||
| ŌĆāPost C2ŌĆōC7 SVA (mm) | 37.1┬▒18.4 | 23.1┬▒13.2 | 0.01* | 31.0┬▒15.1 | 21.6┬▒11.0 | 0.10 |
|
|
||||||
| ŌĆā╬öC2ŌĆōC7 SVA (mm) | 13.1┬▒16.8 | 2.2┬▒8.5 | 0.004* | 11.2┬▒18.2 | 1.0┬▒8.2 | 0.047* |
|
|
||||||
| ŌĆāPre T1 slope (┬░) | 26.3┬▒4.5 | 24.3┬▒7.6 | 0.47 | 26.3┬▒4.1 | 24.5┬▒7.5 | 0.67 |
|
|
||||||
| ŌĆāPost T1 slope (┬░) | 25.2┬▒6.3 | 23.6┬▒8.5 | 0.62 | 23.3┬▒2.0 | 23.4┬▒7.5 | 0.98 |
|
|
||||||
| ŌĆā╬öT1 slope (┬░) | ŌłÆ1.2┬▒5.2 | ŌłÆ0.2┬▒6.2 | 0.66 | ŌłÆ2.9┬▒4.8 | ŌłÆ0.1┬▒6.9 | 0.44 |
|
|
||||||
| ŌĆāPre T1 slopeŌĆō╬▓ (┬░) | 15.7┬▒14.3 | 11.5┬▒10.1 | 0.30 | 14.4┬▒17.8 | 11.3┬▒11.0 | 0.61 |
|
|
||||||
| ŌĆā╬│ (┬░) | 12.2┬▒5.2 | 9.6┬▒5.0 | 0.17 | 12.1┬▒5.7 | 8.9┬▒4.7 | 0.20 |
|
|
||||||
| ŌĆā╬┤ (┬░) | 8.9┬▒3.7 | 7.3┬▒4.0 | 0.28 | 7.5┬▒3.0 | 7.4┬▒4.1 | 0.96 |
|
|
||||||
| ŌĆāC5 canal (mm) | 14.0┬▒1.2 | 14.4┬▒1.3 | 0.45 | 14.2┬▒1.4 | 14.7┬▒1.2 | 0.44 |
|
|
||||||
| Computed tomography | ||||||
|
|
||||||
| ŌĆāSAP at C5 level (mm) | ||||||
|
|
||||||
| ŌĆāŌĆāAffected side | 6.3┬▒1.6 | 6.3┬▒2.2 | 0.99 | 6.8┬▒1.5 | 6.6┬▒2.1 | 0.85 |
|
|
||||||
| ŌĆāŌĆāNormal side | 6.4┬▒1.6 | 5.2┬▒2.0 | 0.08 | 6.7┬▒1.5 | 5.2┬▒2.0 | 0.13 |
|
|
||||||
| ŌĆāWIF at C4ŌĆōC5 level (mm) | ||||||
|
|
||||||
| ŌĆāŌĆāAffected side | 2.4┬▒1.1 | 2.3┬▒0.7 | 0.75 | 2.6┬▒1.3 | 2.4┬▒0.7 | 0.59 |
|
|
||||||
| ŌĆāŌĆāNormal side | 2.5┬▒1.0 | 2.8┬▒1.3 | 0.58 | 2.7┬▒1.3 | 2.9┬▒1.3 | 0.69 |
|
|
||||||
| Magnetic resonance imaging | ||||||
|
|
||||||
| ŌĆāNo. of levels of compression | 2.9 (2ŌĆō4) | 1.6 (0ŌĆō3) | 0.001* | 3.0 (2ŌĆō4) | 1.4 (0ŌĆō3) | 0.002* |
|
|
||||||
| ŌĆāThe presence of HIA (%) | 4 of 9 (44) | 20 of 49 (41) | 1.0 | 2 of 5 (40) | 10 of 27 (37) | 1.0 |
Values are presented as mean┬▒standard deviation, number, number (range), or number (%), unless otherwise stated.
╬▒, C2ŌĆōC7 curvature; ╬▓, C2ŌĆōC7 cobb angle; Pre, preoperative; Post, postoperative; SVA, sagittal vertical axis; ROM, range of motion; ╬│, ROM at the C4ŌĆōC5 intervertebral level; ╬┤, ROM at the C5ŌĆōC6 intervertebral level; SAP, superior articular process; WIF, width of the intervertebral foramen; HIA, high-intensity area.
Table┬Ā4
| Variable | Group 1 (n=4) | Group 2 (n=23) | p-value |
|---|---|---|---|
| Plain radiography | |||
| ŌĆā╬▒ (┬░) | 15.0┬▒6.5 | 11.9┬▒13.1 | 0.64 |
| ŌĆā╬▓ (┬░) | 19.5┬▒9.2 | 13.7┬▒15.8 | 0.49 |
| ŌĆāAlignment | 0.15 | ||
| ŌĆāŌĆāStraight | 0 of 4 | 1 of 20 | |
| ŌĆāŌĆāLordosis | 4 | 14 | |
| ŌĆāŌĆāKyphosis | 0 | 6 | |
| ŌĆāŌĆāSigmoid | 0 | 1 | |
| ŌĆāKŌĆōline (ŌłÆ) | 0 | 3 | 1.00 |
| ŌĆāPre C2ŌĆōC7 SVA (mm) | 29.4┬▒5.0 | 21.0┬▒11.3 | 0.17 |
| ŌĆāPost C2ŌĆō7 SVA (mm) | 44.8┬▒21.6 | 25.1┬▒15.8 | 0.04* |
| ŌĆā╬öC2ŌĆōC7 SVA (mm) | 15.4┬▒17.4 | 3.6┬▒8.8 | 0.04* |
| ŌĆāPre T1 slope (┬░) | 26.4┬▒5.5 | 24.1┬▒7.2 | 0.56 |
| ŌĆāPost T1 slope (┬░) | 27.0┬▒9.0 | 23.9┬▒9.8 | 0.56 |
| ŌĆā╬öT1 slope (┬░) | 0.6┬▒5.7 | ŌłÆ0.2┬▒5.3 | 0.78 |
| ŌĆāPre T1 slopeŌĆō╬▓ (┬░) | 7.0┬▒4.7 | 11.3┬▒10.8 | 0.45 |
| ŌĆā╬│ (┬░) | 12.3┬▒5.3 | 10.6┬▒5.3 | 0.56 |
| ŌĆā╬┤ (┬░) | 10.7┬▒4.1 | 7.3┬▒3.9 | 0.13 |
| ŌĆāC5 canal (mm) | 13.8┬▒1.1 | 14.0┬▒1.4 | 0.81 |
| Computed tomography | |||
| ŌĆāSAP at C5 level (mm) | 0.76 | ||
| ŌĆāŌĆāAffected side | 5.4┬▒1.4 | 5.8┬▒2.3 | |
| ŌĆāŌĆāNormal side | 6.2┬▒2.1 | 5.1┬▒1.9 | 0.39 |
| ŌĆāWIF at C4ŌĆōC5 level (mm) | 0.92 | ||
| ŌĆāŌĆāAffected side | 2.2┬▒1.1 | 2.3┬▒0.8 | |
| ŌĆāŌĆāNormal side | 2.4┬▒0.7 | 2.6┬▒1.2 | 0.72 |
| Magnetic resonance imaging | |||
| ŌĆāNo. of levels of compression | 2.8 (2 to 3) | 2.0 (0 to 3) | 0.13 |
| ŌĆāThe presence of HIA (%) | 2 of 4 (50) | 10 of 22 (45.5) | 1.0 |
| ŌĆāPre D at C4ŌĆōC5 level (mm) | 0.6┬▒0.7 | 0.8┬▒0.9 | 0.93 |
| ŌĆāPost D at C4ŌĆōC5 level (mm) | 1.8┬▒1.3 | 2.3┬▒1.0 | 0.41 |
Values are presented as mean┬▒standard deviation, number, number (range), or number (%), unless otherwise stated.
╬▒, C2ŌĆōC7 curvature; ╬▓, C2ŌĆōC7 cobb angle; Pre, preoperative; Post, postoperative; SVA, sagittal vertical axis; ROM, range of motion; ╬│, ROM at the C4ŌĆōC5 intervertebral level; ╬┤, ROM at the C5ŌĆōC6 intervertebral level; SAP, superior articular process; WIF, width of the intervertebral foramen; HIA, high-intensity area; D, distance between posterior edge of C4ŌĆōC5 disc and anterior aspect of spinal cord.






