 |
 |
- Search
| Asian Spine J > Volume 17(2); 2023 > Article |
|
Abstract
The current study was carried out systematically by conducting a review of the literature. The purpose of this study was to conduct a systematic review of the literature to determine the effects of brace wearing on sagittal parameters in adolescents with idiopathic scoliosis (AIS). In this study, PubMed/MEDLINE (National Library of Medicine), Scopus, Ovid, CINAHL, PEDro, Google Scholar, and the Cochrane Library were accessed and searched using the patient, intervention, comparison, outcome, and study design model. We included studies that looked at the effects of brace treatment on sagittal spinopelvic parameters in AIS patients over the age of 18. The studies were chosen for their cross-sectional, retrospective, or prospective observational designs, and they were published in English. Review articles, case reports, case study designs, and conference abstracts were excluded from consideration. The methodological quality of the remaining articles was assessed using the Newcastle Ottawa Scale. A total of 12 studies were chosen, and 995 participants were evaluated, with 3 (25%) and 9 (75%) having high and moderate quality, respectively. The studies were classified based on the length of follow-up. Long-term, short-term, and immediate effects of brace wearing on sagittal spinopelvic parameters were reported in four, five, and three studies, respectively. The results of nine studies showed a significant decrease in Cobb angle after wearing the brace, which contradicted the findings of the other two. The cervical and sagittal pelvic parameters, thoracic kyphosis (TK), lumbar lordosis (LL), spinopelvic parameters, and sagittal balance were all evaluated in the intended studies, yielding varying results. According to the available literature, wearing a brace flattens the TK and LL. According to this systematic review, brace treatment may affect sagittal spinopelvic parameters in adolescents with AIS, particularly in TK and LL. The cervical and pelvic parameters yielded inconclusive results. This study backs up the idea that brace design and structure can influence sagittal parameter changes. The limitations of this study include different methods of parameter measurement, variations in the brace types and wear time, varying follow-up duration, and differences in participant characteristics.
Adolescent idiopathic scoliosis (AIS) is a complex three-dimensional axial skeleton deformity characterized by lateral displacement of a series of vertebrae and vertebral rotation [1]. In AIS, the alignment of the spinal column in the sagittal plane is influenced, resulting in instability and buckling under self-gravity pressure [2,3].
Brace treatment has been the most common nonsurgical treatment for AIS with mild to moderate curves over the last 50 years [4]. The primary goal of brace treatment in AIS is to prevent or minimize curve progression and provide spinal stabilization for adolescents with skeletal immaturity during their growth period until they reach skeletal maturity [4–6]. According to recent studies, this treatment failure is accompanied by a lack of in-brace frontal curve correction, low brace compliance, and a high body mass index. However, the majority of AIS research has concentrated on the frontal plane rather than the sagittal plane. A growing body of literature has emphasized the significance of sagittal-plane parameters and brace treatment outcomes in AIS. Sagittal parameters of interest include cervical sagittal parameters, thoracic kyphosis (TK), lumbar lordosis (LL), and pelvic parameters (e.g., pelvic incidence [PI], pelvic tilt [PT], and sacral slope [SS]).
Thoracic hypokyphosis is the most common sagittal malalignment seen in AIS. During the pubertal developmental stage, it follows the asymmetric growth of the anterior and posterior spinal columns [7,8]. According to Ylikoski [2], curve progression in the frontal plane is determined by TK severity, with curves with mild TK progressing faster than those with high TK. Furthermore, pelvic alignment is strongly related to sagittal spinal alignment [9]. To maintain an energy-efficient upright posture in patients with spinal sagittal malalignment, compensatory abnormal PT is usually adapted [10,11]. Pelvic anteversion can result in sagittal-plane spinal malalignment due to a thoracic curve to the spinal rotation and hip axis. It may have a negative biomechanical impact on the apical region, exacerbating axial instability and curve progression [3]. AIS progression and development are linked to sagittal-plane spinal malalignment and altered pelvic posture. As a result, failure to pay attention to sagittal parameters during brace treatment may result in treatment failure or further curve progression.
According to the Scoliosis Research Society, the coronal plane Cobb angle may not describe all scoliosis features [12], and other three-dimensional parameters, such as Cobb angle stabilization, are just as important. As a result, monitoring the Cobb angle is insufficient for tracking the scoliosis condition. The purpose of this study was to review recent research on the effects of brace treatment on the head to sagittal pelvic parameters in AIS.
This systematic review was performed following the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) 2020 guidelines [13], outlined in Fig. 1. The protocol of this review was registered with PROSPERO on December 24, 2020 (International Prospective Register of Systematic Reviews, http://www.crd.york.ac.uk/PROSPERO/; # CRD42020222360). As this is a systematic review of published articles, no ethical approval and patient consent were required.
The inclusion criteria included studies assessing the effects of brace treatment on sagittal spinopelvic parameters in AIS, focusing on individuals with AIS, aged ≤18 years, treated with a brace and no other previous treatment, having a cross-sectional, retrospective, or prospective observational design, and publishing in English. However, review studies, case studies, conference abstracts, and articles with no available full text were excluded.
A systematic computerized search was conducted in PubMed/MEDLINE (National Library of Medicine), Scopus, Ovid, CINAHL, PEDro, Google Scholar, and the Cochrane Library using the population, intervention, comparison, outcome, and study design (PICOS) model in the current study (Table 1). In this regard, the studies published in English between April 2000 and April 2021 (April 2000–April 2021) were investigated using the combined keywords in PubMed: [(Scolios*{tiab}) or (“Spinal deformity” {tiab})] and [(Orthotic device”{Mesh} or Orthotic*{tiab}) or Brace*{tiab})] and [(“Cobb angle” {tiab}) or (Sagittal and Balance {tiab}) or (Sagittal and Alignment {tiab}) or (Sagittal and Profile* {tiab}) or (Sagittal and Parameter* {tiab})] and [(Adolescent*{tiab}) or (Teen*{tiab}) or (Youth*{tiab}) not (Surgery*)]. Keywords were searched individually and then combined with the initial search strategy. Changes were made to the basic search strategy for each of the other databases as needed. Additionally, eligible studies were identified through citation tracking and reference lists sifting through selected studies and relevant systematic reviews. A manual keyword search on the internet was also performed. Two reviewers (F.Gh. and H.R.) independently conducted a computerized literature search in the aforementioned bibliographic online databases. The reference lists of relevant studies and the key journals in the topic field were evaluated. Endnote Reference manager software (Clarivate, Philadelphia, PA, USA) was used to collect all potentially relevant studies [14].
Duplicate studies were removed automatically and manually; potentially relevant studies were chosen by two reviewers (F.Gh. and T.B.) after separately screening titles and abstracts. At each stage, the reviewers independently evaluated identified studies to determine whether they were eligible, ineligible, or potentially eligible. The full texts were then reviewed following the inclusion/exclusion criteria. Any disagreement between the reviewers was resettled through a consensus meeting among these authors. Additionally, if the title and abstract did not provide sufficient information, a full-text review was conducted. Before conducting the review process, the eligibility criteria were piloted and based on PICOS. The PRISMA flow diagram summarizes the entire study selection process (Fig. 1).
The full texts of eligible studies were reviewed by two reviewers (F.Gh. and T.B.), and relevant outcome information from each study was extracted. The extracted data included the first author’s name, study design, gender, age, Risser stage, Cobb angle at the start of brace treatment, brace type, prescribed brace-wearing time, follow-up duration, and outcome measures, as well as the year of publication and number of patients. Sagittal spinopelvic parameters are classified as cervical parameters (e.g., cervical lordosis [CL], C2 slope angle [C2S], and C2–7 sagittal vertical axis [CSVA]), TK, LL, PI, PT, and SS, which were evaluated as primary outcome measures.
Two reviewers (F.Gh. and T.B.) independently appraised the scores of the full texts using the Newcastle Ottawa Scale [15,16] based on the Cochrane Collaboration’s endorsement to assess the quality of observational studies in its 2011 handbook [17]. This 10-item tool was created to examine participant selection and study design, comparability of groups, and exposure/outcome determination. Each item in the quality assessment tool is scored zero (missing or insufficient data) or one (sufficient data are available), resulting in an average score for this tool ranging between 0 and 10. The scores of 7–10, 4–6, and 0–3 indicate a high-, moderate-, and low-quality study, respectively. Each scoring was hidden from the reviewers. In the event of disagreement, the third reviewer (M.K.) commented on the discussion.
Following the initial literature search, 453 titles were obtained. After screening their title/abstract, 12 studies met the inclusion criteria, two of which were conducted ambispectively, while one, seven, and two had prospective, retrospective, and cross-sectional designs, respectively.
Table 2 summarizes the characteristics of the eligible studies. Long-term, short-term, and immediate follow-up studies are shown in dark gray, medium gray, and light, respectively. The intended studies had a total sample size of 995 people between the ages of 10 and 16. Furthermore, in six studies, the daily time spent wearing a brace ranged from 8 to 23 hours [7,9,18–21]. The follow-up period for the retrospective and prospective studies was 6–24 months (short term) [7,9,11], while it ranged from 4 to 48 months for the retrospective ones [3,19–24]. A brace was prescribed for the Chêneau [20,21,23–25], Milwaukee [3,9,25], SpineCor [7], Charleston bending [25], nighttime brace [11,19], Sforzesco [18], Boston bracing system [22], elastic belt [3], Griffet Thévenot Barral (GTB) [25], Lyonnais [25], and thoracolumbosacral orthosis (TLSO) [11]. Except for three studies, which included only female patients, all of the studies included both male and female participants [3,18,20].
In this systematic review, we investigated the effects of bracing on sagittal spinopelvic parameters in adolescents with AIS. According to the findings of this systematic review, brace treatment may alter the head-to-pelvis parameters of adolescents with AIS, particularly in TK and LL. In general, it appears that the brace type is important when considering the sagittal-plane parameters of the spine. The use of underarm braces may lead to flatback deformity. Further TK reduction in hypokyphosis patients is counterproductive to the brace’s goal of restoring the spine to a more normal alignment. In this regard, the forces within a brace must be adjusted to reduce the adverse effect on sagittal profiles. As a result, wearing a brace with a dynamic scoliosis pad, the location of which can be adjusted by an orthotist based on the curve characteristics, may provide a better result. The findings of this review are discussed in greater detail below.
Several studies have recently proposed cervical parameters to determine the sagittal balance of AIS [26–29]. Lower cervical segments (C4–C7) have a greater sagittal-plane range of motion (flexion/extension) than upper segments (C2–C4) in the cervical spine [30]. Cervical spine mobility increases to maintain neutral alignment and the horizontal gaze because of the changes in thoracolumbar alignment [31]. Cervical misalignment (e.g., reduced CL) significantly contributes to headaches and neck pain, thereby lowering the quality of life [32]. A high-quality study found a gradual decrease in CL during treatment with a Chêneau brace [20]. This implies that, even though the Chêneau brace lacks a superstructure and a neck section like the Milwaukee brace, it has a significant effect on CL. Given the relationship between the thoracic and cervical regions, changes in TK can result in changes in CL. A moderate-quality study, however, found no significant change when examining the immediate effect of a Chêneau type brace on cervical sagittal parameters [24].
C2S is the angle between the lower endplate of C2 with the horizontal plane [33]. In a high-quality study, no significant change was found in the effect of wearing the Chêneau brace on C2S [20]. The findings do not correspond to a study of moderate quality, demonstrating a significant decrease [24].
The CSVA is an important parameter for evaluating the sagittal alignment of the cervical spine. It is defined as the distance between the upper posterior corner of C7 and a perpendicular line drawn from the middle of C2 [34]. In an asymptomatic case, the shape of C2–C7 is not always lordotic, and it should not be used as a normal reference in X-ray analysis [31]. In this regard, contradictory findings have been obtained; a high-quality study found no significant change in CSVA during brace treatment [20], while a moderate-quality study discovered a significant reduction [24].
C0–C1 and C1–C2 angles are assumed between the line passing through the midpoints of the C1 anterior and posterior arches with the McRae line and the line tangential to the inferior edge of the C2 body [35]. The C2-pelvic angle is the angle formed by a line drawn from the C2 centroid to the femoral heads (FH) and another drawn from the FH to the center of the S1 endplate [36]. A study of moderate quality assessed the changes in these three parameters following brace treatment and found no significant difference [24]. It appears that surgical intervention has a greater impact on these parameters than brace treatment. More information on the effect of brace treatment on these parameters would assist researchers in establishing a higher degree of accuracy in this matter. T1–CL mismatch was also assessed in a study of moderate quality and it was found to be significantly reduced after wearing a brace [24]. Furthermore, the distance between the C7 plumb line and the central sacral perpendicular line is denoted as the C7-central sacral vertebral line (C7-CSVL) [37]. According to a moderate-quality study [22], this parameter significantly decreased from the start of brace treatment to 2 years later.
The cervical–thoracic pelvic angle, defined as the angle between a line from the C2 centroid to FH and a line from FH to the center of T1, is a global angular measure of cervical sagittal balance that is correlated with the C2–C7 plumb line [36]. A study of moderate quality found a significant decline in this parameter [24]. Changes in sagittal spinopelvic parameters within the brace can demonstrate this phenomenon.
A high-quality study proposed that the brace treatment had a significant effect only on CL [20]. A moderate-quality study, however, found that wearing a brace had no effect on CL, upper-cervical parameters, or horizontal gaze maintenance [24]. Furthermore, despite causing minor changes in the lower cervical spine posture, the brace treatment does not result in alignment changes.
Although braces are effective in reducing scoliosis curves, they can cause TK to decrease and a flat back to develop. According to the findings of this systematic review, wearing a brace may have a negative impact on the patients’ TK as well as applying abnormal antikyphotic forces to the thoracic spine. However, different studies have used a variety of methods to assess TK (e.g., angle measurement between T1 and T12, T4 and T12, and T5 and T12). Previous research has found a strong link between thoracic hypokyphosis and decreased pulmonary function in patients with AIS [38–40]. The antikyphotic effect of the brace, however, should not be regarded as an absolute negative complication. This problem is attributed in some patients to a reduction of kyphosis angle above 40° at the start of treatment to its normal range (30°–35°) after using a brace in some patients [7]. Paying attention to this result in AIS patients with thoracic hypokyphosis is critical so that the brace does not exacerbate the effects of hypokyphosis. As a result, keeping the TK angle within the normal range during brace treatment is a critical issue that should be addressed in a clinical setting.
According to a high-quality study, the TK angle significantly decreases six months after wearing the SpineCor brace [7]. The decrease in kyphosis angle indicates the brace’s antikyphotic effect on the sagittal-plane alignment in the short term. Some AIS patients have hyperkyphosis (kyphosis angle >45°), which should be concurrently improved with scoliosis control, and the kyphosis angle should return to normal. According to two moderate-quality studies [18,24], the TK significantly decreases after wearing Sforzesco and Chêneau braces [18,24]. Furthermore, the TK remained constant in the normal range in two moderate-quality studies that measured the TK angle in the T1–T12 region [23,25] and another that did not mention the TK angle-specific region [14].
The TK was determined in six studies by measuring the angle of the T4–T12. A moderate-quality study that looked at the short-term effect of the Sforzesco brace found no significant difference [18]. According to some studies, wearing a Chêneau brace significantly decreases the TK, resulting in more hypokyphosis than the normal and flat back position [20,21]. According to a high-quality study, the rate of hypokyphosis remains constant for up to 1 year after treatment ends [20]. Another high-quality study discovered that 11% of patients developed a flat thoracic back after treatment [21]. As a result, the anterior pad of the Chêneau brace appears to be ineffective in dealing with the flat back syndrome, particularly in the rib hump area. Using the Milwaukee brace reduces TK in patients, according to a moderate-quality study [9]. Despite the patient’s hyperkyphosis at the start of the treatment (mean TK: 55.9°±15.3°), brace use reduces kyphosis to normal (mean TK: 38.5°±6.4°).
The TK was determined in the T5–T12 region in two moderate-quality studies, which revealed a significant decrease [3,22]. In terms of the T1 slope angle (T1S), or the angle between the upper endplate of T1 and the horizontal plane [34], inconsistent results have been obtained. A high-quality study found that wearing a brace did not affect T1S [20]. A moderate-quality study, however, found that wearing a brace causes a significant reduction in T1S [24]. According to the authors of a review study, C7 or T1 slope is an important parameter that clinicians can use to compare treatment outcomes in patients with spinal pathologies [31]. Further research into the long-term outcomes of brace treatment in AIS would be fruitful in this area.
The LL angle is usually slight in scoliosis patients, but it can be further reduced by wearing a brace [11]. The shear forces produced by the brace along the spine may cause LL reduction [20]. Because the skeletal system is a closed chain, changes in one part affect the normal balance in the others. As a result of their interrelationship, the lumbar and thoracic spine geometries should be globally examined [23]. Hypokyphosis can result in hypolordosis as a form of compensation and possibly the lowest energy consumption [23]. Following the reduction in TK, the corrective force on scoliotic curves in patients can be applied more effectively [9].
Some studies assessed LL using L1–L5 vertebrae, measuring the angle between the upper endplate of L1 and the lower endplate of L5. In this regard, four moderate-quality studies revealed that bracing significantly reduces LL [3,9,22,23]. Two studies of moderate quality, however, referred to the unchanged LL [18,19]. According to a moderate-quality study [3], using the Milwaukee brace reduces the LL, whereas the elastic belt does not affect the lordosis angle. The differences in results can be attributed to structural differences between the two orthoses. The stimulating effect of the neck ring on the mandible, causing an “upward extension” reflex reaction in the trunk, has been attributed to the significant LL reduction following treatment with the Milwaukee brace. This “upward extension” can have the effect of a “pull strength,” resulting in a flat spine. A moderate-quality study found a concomitant decrease in LL of 11.5° in patients with a decrease in the maximum TK of more than 10° [22].
Preliminary research on pelvic alignment in scoliosis patients has suggested that the alignment has a significant effect on sagittal spinal balance. As a result, the pelvic position can affect the LL and TK [41,42]. Furthermore, changes in kyphosis and lordosis have an impact on pelvic parameters [9]. The changes in the spine caused by scoliosis cause definite changes in the pelvic parameters to maintain the spinopelvic sagittal balance. In the sagittal plane, the main pelvic parameters are PI, PT, and SS.
The PI is a reliable criterion for determining SS and LL variations [43]. The increased PI is linked to overall changes in AIS patients’ sagittal alignment and is thought to be a risk factor for progressing scoliotic curvature. The PI is an important morphological parameter that is significantly higher in AIS patients than in normal adolescents [3,41,42,44]. Some studies (two high-quality and five moderate-quality studies) have found that the PI remains unchanged after wearing a brace [20,21]. However, a significant decrease in the PI was discovered in two moderate-quality studies [18,25]. According to previous research, the PI is a relatively constant criterion that slightly improves from the bipedalium stage to skeletal maturity. The hypothesis in the case of patients with a change in the PI is that the PI decreases when the brace exerts a prolonged force on the sacral caudal and anterior iliac crest [21].
The mean vertical torsion of the two surface normal (or tangential planes) on the right and left dimples is the pelvic inclination. The positive and negative pelvic inclination indicate a mean vertical component that is upward or downward, respectively [7]. Only in a high-quality study did the effect of wearing a SpineCore brace on pelvic inclination show a significant reduction [7].
Changes in the PT are significantly related to the changes in LL. As a result, patients whose LL has flattened while wearing a brace experience compensatory retroversion with increased PT [11]. One high-quality and five moderate-quality studies demonstrated the ineffectiveness of PT bracing [9,18,22–24]. The findings contradict those of one high-quality study and two moderate-quality studies which suggested a significant increase in the parameter after bracing [22,25]. According to a moderate-quality study, wearing a Boston brace can increase PT by 3.8°, resulting in pelvic retroversion or a decrease in anteversion [22]. As a result, anteversion decreases as a compensatory mechanism to maintain a stable posture, and as a result, energy consumption decreases by changing the sagittal balance. As a result, the brace should place the pelvic joint in retroversion to more effectively correct lumbar scoliosis.
The horizontal distance (mm) between the C7 plumb line and the superior posterior corner of the sacral endplate is known as the sagittal vertical axis (SVA) [22]. The global alignment measured by the SVA becomes closer to the trunk’s central axis after wearing the brace. The majority of patients have a negative baseline balance that becomes positive after using the brace. Three studies have looked at the effect of brace wearing on SVA in patients with idiopathic scoliosis. A high-quality [21] and a moderate-quality [22] brace showed a significant decrease in the criterion after long-term brace use. It is unclear whether the compensatory change is caused by decreasing LL because it is a maneuver to maintain a stable posture to reduce energy consumption [22]. However, a study of moderate quality found that the SVA does not change [23].
The spinosacral angle (SSA) is the angle formed by the upper sacral endplate and the line connecting the endplate’s center to the C7 vertebral body [46]. The SSA assesses global kyphosis as well as sagittal spinal alignment, which is determined by the position of the C7 and SS [47,48]. According to a moderate-quality study, bracing significantly reduces this parameter [23]. This reduction is related to the anterior translation of the SVA and SS flattening, indicating that the brace improves global kyphosis in people with scoliotic thoracic curvature [23].
The SS, the angle between the sacral plate and horizontal line [49], was investigated in two high-quality studies [20,21] and three moderate-quality studies [9,18,25], with no significant change found. Changes in the LL are correlated with the PT, SS, TK, and Cobb angles, according to a moderate-quality study [11]. Additionally, a moderate-quality study found a positive relationship between spinopelvic parameters [8]. According to the abovementioned direct correlation, the SS and PI are reduced when the LL, Cobb angle, and TK are reduced due to the compensatory function of the pelvis.
The changes in T1SPI and T9SPi, which are the angles between the perpendicular plumb line and the line connecting the centroid of the T1 or T9 vertebral body and the bicoxofemoral axis, were assessed in a moderate-quality study [50,51]. The findings indicated that there was no statistically significant difference [23].
The trunk shift is calculated by plotting the CSVL and calculating the deviation from the midpoint of the two widest rib cage points along a horizontal parallel line [52]. A study of moderate quality highlighted a significant increase in trunk shift in patients through immediate and long-term evaluation [22].
The normal spine’s sagittal balance is the most efficient physiological alignment of the spine by muscular forces. In other words, it is possible to achieve it by balancing external forces (for example, gravity) and trunk muscular response [53]. The sagittal balance is measured by two lines, one of which, the A-line, connects the midpoint of C7 perpendicular to the radiograph’s vertical margin. The B-line is drawn perpendicular to the radiograph’s vertical margin from the upper posterior corner of S1. As a result, A=B represents a neutral balance [54]. According to a high-quality study [21], the Chêneau brace may improve sagittal balance by applying posterior pressure to the rib hump, resulting in significant forward translation of the SVA.
This study had some significant limitations. For starters, the vertebrae level considered for evaluating TK and LL varied across studies. This limitation adds to our understanding of the effect of bracing on the TK and LL of adolescents with AIS. Second, 11 of the included studies used retrospective designs, which resulted in selection bias. Thirdly, there was no control group (AIS patients without a brace) in included studies to compare bracing effects on sagittal spinopelvic parameters of AIS cases to patients without a brace. Fourthly, brace compliance is an important factor that influences bracing outcomes in AIS. The lack of objective data on daily brace-wearing time limits the study. Clinicians and researchers would be able to detect differences in compliance between the brace treatment failure and success groups if they were able to objectively monitor brace wear. Despite these limitations, this study provides insight into the significance of sagittal spinopelvic parameters when managing AIS with a brace. This study raises the question of whether better sagittal alignment in a brace leads to better clinical outcomes and fewer complications. Large prospective controlled trials may provide more conclusive evidence.
Since some studies did not examine all sagittal parameters, no specific result regarding the effects of brace wearing can be obtained. According to this systematic review, wearing a brace flattens the TK and LL regardless of the type of scoliosis curve, which is more common in patients with a thoracic curve. The sagittal alignment of the spine influences the development and progression of scoliosis as well as the correctability of frontal plane deformity. Furthermore, bracing has opposing effects on cervical and pelvic sagittal parameters. As a result, these parameters should be evaluated in studies focusing on the effectiveness of the brace. More research is needed to gain a complete picture of the effect of brace wearing on the parameters.
Acknowledgments
The authors appreciate the Iran University of Medical Sciences for supporting this research (grant number: 19239).
Notes
Author Contributions
Conception and idea: M. Kamali, F. Ghorbani, H. Ranjbar, M. Kamyab, T. Babaee, H. Razavi, P. Sharifi; intellectual content: M. Kamali, H. Ranjbar, T. Babaee; data analysis and interpretation: F. Ghorbani, T. Babaee, L. Janani; literature search and data extraction: F. Ghorbani, H. Razavi; manuscript preparation, writing, and revision: F. Ghorbani, H. Razavi; manuscript editing: P. Sharifi; manuscript editing and review: M. Kamali, H. Ranjbar, T. Babaee; supervision: M. Kamali, H. Ranjbar, M. Kamyab, T. Babaee, L. Janani; and approval of final manuscript: M. Kamali, H. Ranjbar, M. Kamyab, T. Babaee, P. Sharifi, L. Janani.
Fig. 1
PRISMA (Preferred Reporting Items for Systematic Reviews and MetaAnalyses) flow diagram 2020.
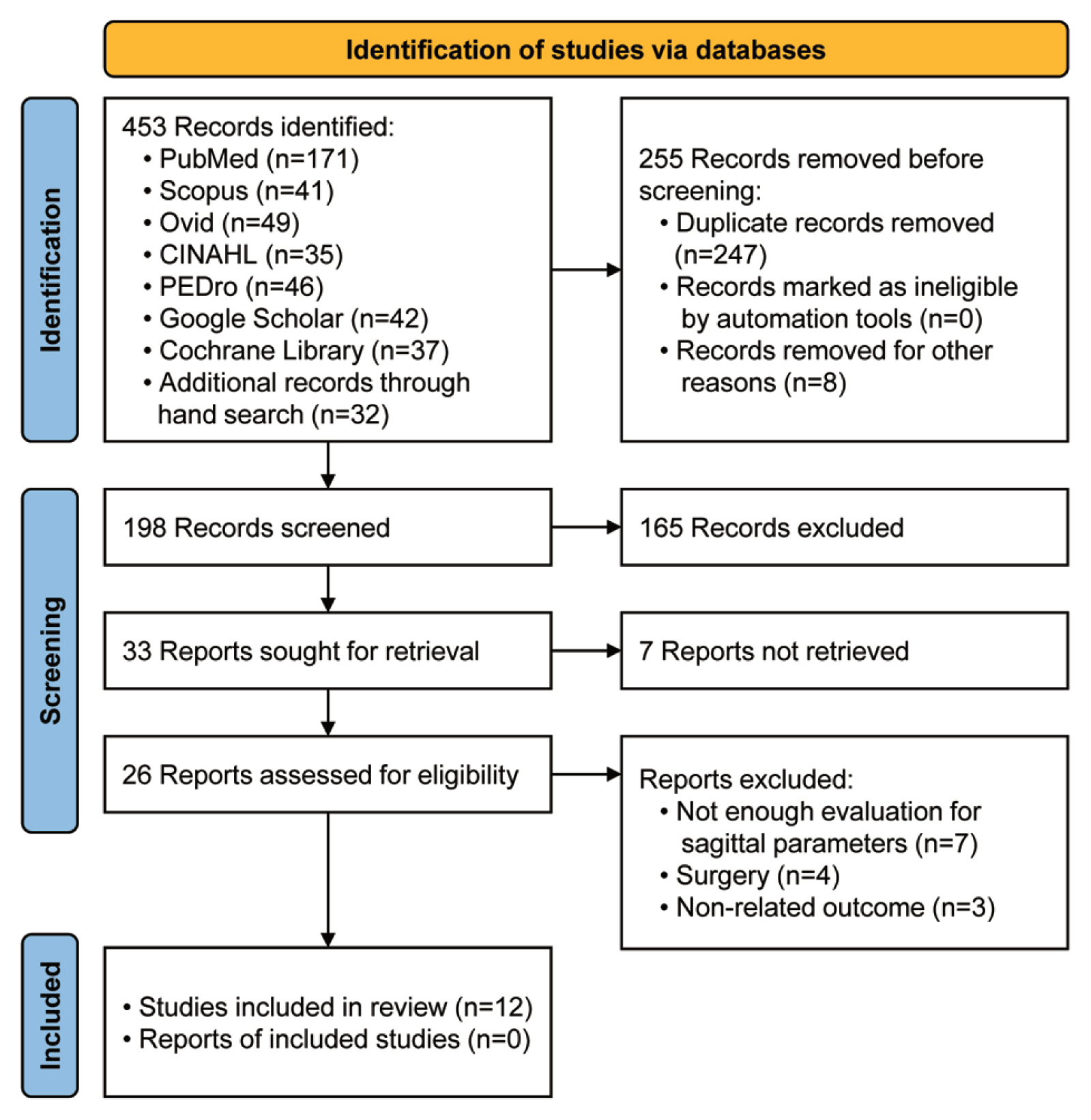
Table 1
Eligibility criteria based on the PICOS model
Table 2
Characteristics of included studies
| References (quality) | No. of patients (no. of men) | Age of total group (yr), mean (range) | Initial Risser stage, mean (range) | Type of brace | Prescribed wear-time (hr/day), mean (range) | Measurement method | Initial cobb angle (°), mean (range) | Follow-up, mean (range) | Selected quotation of conclusion |
|---|---|---|---|---|---|---|---|---|---|
| Zhang et al. [20] (2020) (high)a) | Retrospective; sample: 275 (0) | 12.74±1.21 (11–16) | (0–2) | Chêneau brace | 20 (12–23) | X-rays | 29.02±8.51 | (>2 yr) | “CL, TK, and LL decreased gradually and significantly during long-term bracing treatment, which lead to the aggravation of “flat back” in AIS patients. Nevertheless, pelvic parameters have not changed significantly in the global statistics.” |
| Cheung et al. [22] (2019) (moderate)a) | Retrospective; sample: 265 (40) | 12.53±1.17 (10.0–15.9) | (0–2) | Boston brace | - | X-rays | 31.0±3.8 | 3.9±1.3 yr (>2 yr) | “Brace treatment leads to flatback deformity with thoracic hypokyphosis and lumbar hypolordosis. Changes in the thoracic spine are associated with similar changes in the lumbar spine. Increased sacral slope, reduced pelvic tilt, and pelvic incidence are associated with reduced lordosis in the lumbar spine after bracing.” |
| Lateur et al. [19] (2016) (moderate)a) | Retrospective single-center; sample: 142 (25) | 11.6 (7–14) | Risser 0/1: 93; Risser 2: 27; Risser 3: 22 | Night-time brace | (8–10 non-stop; night-long) | EOS imaging system | 15.5 (10–25) | 45 mo (10–92 mo) | “The present study confirmed the efficacy of non-operative treatment by night-time brace in mild progressive idiopathic scoliosis (<25°) in a large majority of cases. A night-time brace thus seems to be an effective option for the treatment of adolescent scoliosis, ensuring a safe curve of around 20°.” |
| Fang et al. [21] (2015) (high)a) | Retrospective; sample: 32 (3) | 12.9±0.9 (11.1–14.5) | (0–2) | Chêneau brace | Minimum 23 | X-rays | 30.6 | 24.4±12.5 mo | “This study reveals the high variability of the effect of brace treatment on sagittal alignment. Chêneau brace treatment may influence sagittal global balance.” |
| Saeedi et al. [9] (2020) (moderate)b) | Retrospective and prospective; sample: 25 (2) | 12.7±1.6 (10–15) | - | Milwaukee brace | 23 | X-rays | 31.8±5.9 (22–44) | 17.1±12.5 mo (6–24 mo) | “Our study results show significant associations between the sagittal pelvic parameters and the spinal parameters during the brace treatment of adolescents with idiopathic scoliosis.” |
| Vergari et al. [11] (2019) (moderate)b) | Retrospective and prospective; sample: 42 (15) | 13±2 | (Risser sign ≤2) | TLSO (30); night-time brace (12) | - | EOS imaging system | 29.2±12.1 (16–61) | <9 mo | “Analysis of sagittal alignment from head to pelvis showed that bracing further flattened the patients’ backs and induced large compensating reorientations of the pelvis..” |
| Almansour et al. [23] (2019) (moderate)b) | Retrospective single-center; sample: 38 (9) | 12.6±2 (10–16) | (0–2) | Chêneau brace | - | EOS imaging system | 31.4±6.4 (19–41) | 4 mo | “The impact of the brace in this study on the sagittal profile was variable, including the loss of thoracic kyphosis and lumbar lordosis.” |
| Diab et al. [7] (2017) (high)b) | Prospective; sample: 9 (3) | 16.89±2.15 (12–20) | (Risser sign >2) | SpineCor brace | 20 | X-rays; 3D Formetric II system | (20–40) | 6 mo | “The SpineCor brace with exercise as well as exercise alone comparing pre to post test were beneficial in reducing thoracic hyperkyphosis, lumbar lordosis, pelvic inclination as well as trunk imbalance in the short term, but comparing between groups, only the SpineCor brace with exercise improved thoracic hyperkyposis.” |
| Donzelli et al. [18] (2016) (moderate)b) | Cross-sectional (prospective database); sample: 16 (0) | 14.01 | - | Sforzesco brace | 23 | EOS imaging system | 38.20±15.42 | - | “The Sforzesco brace mostly modifies the middle of the spine and preserves the sagittal balance.” |
| Pepke et al. [24] (2021) (moderate)c) | Retrospective single-center; sample: 93 (23) | 13.3±2.5 | (0–2) | Chêneau brace | - | Conventional radiography, EOS imaging system | M curve: 30.2±8.0; S curve: 22.9±6.7 | Immediate | “The impact of the brace lead to loss of LL in all AIS patients of this study cohort. Loss of TK was noticed only in normokyphotic patients and was unchanged in hypokyphotic patients. No pelvic compensation was needed during brace treatment. In-brace patients revealed small changes of the lower cervical parameters such as T1-Slope and C2-slope, but without alteration of kyphotic CL. The upper cervical spine did not reveal any changes. Therefore, the influence of brace therapy on the lower cervical spine is marginal and not existent on the upper cervical spine.” |
| Courvoisier et al. [25] (2013) (moderate)c) | Cross-sectional study; sample: 30 (7) | 11 (8–14) | (0–4) | Cheneau brace (18); Milwaukee (5); GTB (3); Lyonnais (2); Charleston (2) | - | EOS imaging system | 28±15 | Immediate | “The Cobb angle was significantly improved. It also showed a significant hypolordotic effect. However, the results showed a high variability of the brace treatment effect in almost every parameter.” |
| Jiang et al. [3] (2010) (moderate)c) | Retrospective; sample: 28 (0) | 14.0 (12–16) | 1.8 (0–4) | Elastic orthotic belt; Milwaukee brace | - | X-rays | 29.6 (20–44) | Immediate | “Although Milwaukee brace leads to significant decreased TK in AIS patients, the change of TK is small. Elastic orthotic belt could result in a more severe thoracic hypokyphosis compared with Milwaukee brace.” |
Table 3
Quality assessment of studies
| Quality assessment criteria | Long-term | Short-term | Immediate | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
|
|
|
||||||||||
| 1. Zhang et al. [20] (2020) | 2. Cheung et al. [22] (2019) | 3. Lateur et al. [19] (2016) | 4. Fang et al. [21] (2015) | 5. Vergari et al. [11] (2019) | 6. Saeedi et al. [9] (2019) | 9. Almansour et al. [23] (2019) | 7. Diab et al. [7] (2017) | 8. Donzelli et al. [18] (2016) | 10. Pepke et al. [24] (2021) | 12. Courvoisier et al. [25] (2013) | 11. Jiang et al. [3] (2010) | |
| 1. Representativeness of the exposed cohort | 1 | 1 | 0 | 1 | 1 | 1 | 1 | 0 | 0 | 1 | 1 | 0 |
|
|
||||||||||||
| 2. Selection of the non-exposed cohort | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
|
|
||||||||||||
| 3. Ascertainment of exposure | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
|
|
||||||||||||
| 4. Precision of exposure dose ascertainment | 1 | 0 | 1 | 1 | 0 | 1 | 0 | 1 | 1 | 0 | 0 | 0 |
|
|
||||||||||||
| 5. Ascertainment of exposure done prospectively or retrospectively | 0 | 0 | 0 | 0 | 1 | 0 | 0 | 1 | 1 | 0 | 0 | 0 |
|
|
||||||||||||
| 6. Demonstration that outcome of interest was not present at start of study or baseline assessment | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
|
|
||||||||||||
| 7. Adjustment for confounding (rendering comparability of cohorts on the basis of the design or analysis) | 0 | 0 | 0 | 1 | 1 | 0 | 0 | 1 | 0 | 0 | 0 | 1 |
|
|
||||||||||||
| 8. Assessment of outcome | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 | 1 |
|
|
||||||||||||
| 9. Was follow-up long enough for outcomes to occur? | 1 | 1 | 1 | 1 | 0 | 1 | 0 | 0 | 0 | 0 | 0 | 0 |
|
|
||||||||||||
| 10. Adequacy of follow-up of cohorts | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | 0 | 0 | 0 | 0 |
|
|
||||||||||||
| Total | 7 | 6 | 6 | 8 | 6 | 6 | 4 | 7 | 5 | 4 | 4 | 4 |
|
|
||||||||||||
| Quality | High-quality | Moderate | Moderate | High-quality | Moderate | Moderate | Moderate | High-quality | Moderate | Moderate | Moderate | Moderate |
Table 4
The clinical determinants of studies
| Radiological parameters | Level of measurement | References | Brace effect | Mean difference | Statistical analysis p-value |
|---|---|---|---|---|---|
| Cobb angle | The uppermost and lowermost vertebrae in the curve (°) | Zhang et al. [20] | Decrease | Pre–post: 29.02±8.51 to 25.66±6.92 | Not provided |
| Cheung et al. [22] | Increase | 5.4±11.1 | <0.001 | ||
| Fang et al. [21] | No change | −3.3±12.0 | 0.13 | ||
| Vergari et al. [11] | Decrease | Pre–post: 29.2±12.1 to 19.1±9.8 | 0.000 (in-brace<pre-brace) | ||
| Donzelli et al. [18] | Decrease | 5.72 ± 5.50 | 0.0008 | ||
| Saeedi et al. [9] | Decrease | Pre–post: 31.8±5.9 to 22.5±6.9 | <0.001 | ||
| Cheung et al. [22] | Increase | 16.9±10.2 | <0.001 | ||
| Donzelli et al. [18] | Decrease | 10.30±7.60 | 0.001 | ||
| Almansour et al. [23] | Decrease | T: 10.6±6.0; TL: 16.5±5.5; L: 12.4±6.7 | 0.0001 | ||
| Courvoisier et al. [25] | Decrease | −6 | 0.001 | ||
| Pepke et al. [24] | Decrease | Pre: 30.2 ±8.0 to 19.8±9.4; post: 22.9±6.7 to 19.0±7.7 | <0.001 | ||
| Lateur et al. [19] | Increase | Pre–post: 15.5 to 16.3 | 0.04 | ||
| Cervical parameters | CL (°) | Zhang et al. [20] | Decrease | Pre–post: 14.13±7.15 to 8.94±5.33 | 0.021 |
| Pepke et al. [24] | No change | Pre–post: 10.7±13.6 to 10.5±13.9 | 0.877 | ||
| C2 slope angle (°) | Zhang et al. [20] | No change | - | >0.05 | |
| Pepke et al. [24] | Decrease | Pre–post: 26.8±8.8 to 24.1±9.1 | 0.001 | ||
| C2–7 SVA (mm) | Zhang et al. [20] | No change | - | >0.05 | |
| Pepke et al. [24] | Decrease | Pre–post: 25±9.9 to 22.1±8.2 | 0.003 | ||
| SVA off-set (=C7-SVA) (mm) | Zhang et al. [20] | No change | - | >0.05 | |
| C7-central sacral vertebral line shift (mm) | Cheung et al. [22] | Decrease | 2.3±13.9 | 0.008 | |
| Cheung et al. [22] | Decrease | 2.3±13.9 | 0.002 | ||
| C0C1 (=C0C1 angle) (°) | Pepke et al. [24] | No change | Pre–post: 2.6±7.4 to 1.7±11.6 | 0.696 | |
| C1C2 (=C1C2 angle) (°) | Pepke et al. [24] | No change | Pre–post: −30.3±12.9 to −9.8±13.4 | 0.674 | |
| T1–CL (=T1–CL mismatch) (°) | Pepke et al. [24] | Decrease | Pre–post: 26.2±11.5 to 23.1±11.9 | 0.032 | |
| CPA (=C2-pelvic angle) (°) | Pepke et al. [24] | No change | Pre–post: 6.9±8.9 to 7.8±9.6 | 0.287 | |
| CTPA (=cervical-thoracic pelvic angle) (°) | Pepke et al. [24] | Decrease | Pre–post: 2.7±1.3 to 2.2±1.1 | 0.000 | |
| Trunk shift (mm) | Cheung et al. [22] | Increase | 4.6±13.0 | <0.001 | |
| Cheung et al. [22] | Increase | 4.6±13.0 | <0.001 | ||
| TK | T1 slope angle (T1S) (°) | Zhang et al. [20] | No change | - | >0.05 |
| Pepke et al. [24] | Decrease | Pre–post:16.3±9 to13.5±8.6 | 0.001 | ||
| T1–T12 TK (°) | Diab et al. [7] | Decrease | 8.66 | 0.000 | |
| Donzelli et al. [18] | Decrease | 2.7 | 0.04 | ||
| Donzelli et al. [18] | Decrease | 5.7 | 0.01 | ||
| Almansour et al. [23] | No change | 2.3±8.3 | 0.095 | ||
| Courvoisier et al. [25] | No change | −2 | 0.14 | ||
| Pepke et al. [24] | Decrease | Pre–post: 32.8±14 to 26.4±13.3 | 0.000 | ||
| T4–T12 TK (°) | Zhang et al. [20] | Decrease | Pre–post: 24.35±7.54 to 19.02±7.12 | 0.001 | |
| Fang et al. [21] | Decrease | −7.1±10.8 | <0.01 | ||
| Donzelli et al. [18] | No change | 2.1 | NS | ||
| Saeedi et al. [9] | Decrease | Pre–post: 55.9±15.3 to 38.5±6.4 | <0.001 | ||
| Donzelli et al. [18] | No change | −0.4 | NS | ||
| Almansour et al. [23] | Decrease | 2.6±6.3 | 0.017 | ||
| Pepke et al. [24] | Decrease | Pre–post: 26.2±12.3 to 23.2±10.6 | 0.000 | ||
| Not mentioned | Lateur et al. [19] | No change | - | NS | |
| T5–T12 TK (°) | Cheung et al. [22] | Decrease | −4.3±8.2 | <0.001 | |
| Cheung et al. [22] | Decrease | −3.4±7.6 | <0.001 | ||
| Jiang et al. [3] | Elastic belt: decrease; Milwaukee: decrease | Belt: 10.4; Milwaukee: 3.5 | El astic belt: <0.05; Milwaukee: <0.05 | ||
| Maximum kyphosis (°) | Cheung et al. [22] | Decrease | −4.3±9.3 | <0.001 | |
| Cheung et al. [22] | Decrease | −5.5±10.0 | <0.001 | ||
| T2T5 (=T2T5 angle) (°) | Pepke et al. [24] | Decrease | Pre–post: 13.5±8.2 to 11.1±7.4 | 0.004 | |
| T5T12 (=T5T12 angle) (°) | Pepke et al. [24] | Decrease | Pre–post: 21.5±11.4 to 19.2±9.4 | 0.002 | |
| TL (=thoraco-lumbar alignment) (°) | Pepke et al. [24] | Decrease | Pre–post: −2±9.3 to −0.5±7.9 | 0.042 | |
| LL | L1–S1 LL (°) | Zhang et al. [20] | Decrease | - | 0.005 |
| Fang et al. [21] | Decrease | −7.1±8.2 | <0.01 | ||
| Vergari et al. [11] | Decrease | Pre–post: −58.2±12.5 to 52.5±10.8 | 0.04 (in-brace>pre-brace) | ||
| Diab et al. [7] | Decrease | 6.8 | 0.000 | ||
| Donzelli et al. [18] | No change | 1.1 | NS | ||
| Donzelli et al. [18] | Decrease | 7.6 | 0.0008 | ||
| Almansour et al. [23] | Decrease | 3.8±7.5 | 0.004 | ||
| Courvoisier et al. [25] | Decrease | 8 | 0.001 | ||
| Pepke et al. [24] | Decrease | Pre–post: −54.3±17.2 to −48±20.1 | 0.011 | ||
| Not mentioned | Lateur et al. [19] | No change | - | NS | |
| L1–L5 LL (°) | Cheung et al. [22] | Decrease | −5.6±12.0 | <0.001 | |
| Donzelli et al. [18] | No change | 0.4 | NS | ||
| Saeedi et al. [9] | Decrease | Pre–post: 56.7±8.8 to 50.6±9.4 | 0.006 | ||
| Cheung et al. [22] | Decrease | −3.8±11.2 | <0.001 | ||
| Donzelli et al. [18] | Decrease | 4.7 | 0.0005 | ||
| Almansour et al. [23] | Decrease | 2.6±6.7 | 0.020 | ||
| Jiang et al. [3] | Elastic belt: no change; Milwaukee: decrease | Belt: -; Milwaukee: 3.0 | Elastic belt: >0.05 Milwaukee: <0.05 | ||
| L1L4 (=L1L4 angle) (°) | Pepke et al. [24] | Decrease | Pre–post: −24.7±10.5 to −19.3±12.7 | 0.000 | |
| L4S1 (=L4S1 angle) (°) | Pepke et al. [24] | No change | Pre–post: −34.8±12.6 to −33.5±13.9 | 0.480 | |
| Pelvic parameters | PI (°) | Zhang et al. [20] | No change | Pre–post: 38.44±18.72 to 32.13±23.44 | >0.05 |
| Cheung et al. [22] | No change | 1.9±20.1 | 0.134 | ||
| Fang et al. [21] | No change | 2.3±7.9 | 0.11 | ||
| Donzelli et al. [18] | No change | 3.8 | NS | ||
| Saeedi et al. [9] | No change | Pre–post: 49.2±16.4 to 51.8±16.0 | 0.57 | ||
| Cheung et al. [22] | No change | 0.4±18.5 | 0.867 | ||
| Donzelli et al. [18] | Decrease | 5.3 | 0.04 | ||
| Almansour et al. [23] | No change | 1.7±6.3 | 0.109 | ||
| Jiang et al. [3] | Elastic belt: no change; Milwaukee: no change | - |
Elastic belt: >0.05 Milwaukee: >0.05 |
||
| Courvoisier et al. [25] | Decrease | −4 | 0.003 | ||
| Pepke et al. [24] | No change | Pre–post: 49.7±14.1 to 49.1±14.1 | 0.211 | ||
| Pelvic inclination (°) | Diab et al. [7] | Decrease | 4.5 | 0.001 | |
| Pelvic tilt (°) | Zhang et al. [20] | No change | - | >0.05 | |
| Cheung et al. [22] | Increase | 3.8±13.6 | <0.001 | ||
| Fang et al. [21] | Increase | 3.8 ± 6.4 | 0.002 | ||
| Donzelli et al. [18] | No change | 1.4 | NS | ||
| Saeedi et al. [9] | No change | Pre–post: 10.9±7.5 to 11.1±7.5 | 0.29 | ||
| Cheung et al. [22] | No change | −0.5±12.6 | 0.531 | ||
| Donzelli et al. [18] | Increase | −3.8 | 0.023 | ||
| Almansour et al. [23] | No change | −1.6±4.9 | 0.057 | ||
| Courvoisier et al. [25] | Increase | −4 | 0.001 | ||
| Pepke et al. [24] | No change | Pre–post: 10.3±6.7 to 11.1±7.5 | 0.144 | ||
| Pelvic obliquity (mm) | Almansour et al. [23] | No change | 0.3±2.5 | 0.446 | |
| PI–LL (=PI–LL mismatch) | Pepke et al. [24] | Decrease | Pre–post: −5.9±12.5 to −1.9±12.1 | 0.000 | |
| Sacral slope (°) | Zhang et al. [20] | No change | - | >0.05 | |
| Cheung et al. [22] | Decrease | −2.0±14.5 | 0.028 | ||
| Fang et al. [21] | No change | −1.5±6.9 | 0.23 | ||
| Donzelli et al. [18] | No change | −2.8 | NS | ||
| Saeedi et al. [9] | No change | Pre–post: 38.3±10.8 to 37.7±8.6 | 0.74 | ||
| Cheung et al. [22] | No change | 0.9±13.8 | 0.386 | ||
| Donzelli et al. [18] | Decrease | 3.4 | 0.003 | ||
| Almansour et al. [23] | Decrease | 3.3±6.5 | 0.004 | ||
| Courvoisier et al. [25] | No change | 0 | 0.82 | ||
| Pepke et al. [24] | Decrease | Pre–post: 41.1±10 to 38.8±10 | 0.002 | ||
| SVA (mm) | Cheung et al. [22] | Decrease | 18.7±34.6 | <0.001 | |
| Cheung et al. [22] | Increase | 23.1±34.9 | <0.001 | ||
| Almansour et al. [23] | No change | −1.6±31.6 | 0.752 | ||
| Spinopelvic parameters | T1SPi (=T1 spinopelvic inclination) (°) | Almansour et al. [23] | No change | −0.06±4.0 | 0.921 |
| T9SPi (=T9 spinopelvic inclination) | Almansour et al. [23] | No change | 0.07±4.7 | 0.930 | |
| SSA (=spinosacral angle) (°) | Almansour et al. [23] | Decrease | 2.4±6.2 | 0.019 | |
| Sagittal balance | Measurement of the sagittal balance includes two lines. The A-line is drawn from the midpoint of C7 perpendicular to the vertical margin of the radiograph. The B-line is drawn from the upper posterior corner of S1 perpendicular to the vertical margin of the radiograph. | Fang et al. [21] | Increase | 13.8±32.1 | 0.02 |
References
1. Weinstein SL, Dolan LA, Cheng JC, Danielsson A, Morcuende JA. Adolescent idiopathic scoliosis. Lancet 2008;371:1527–37.


2. Ylikoski M. Growth and progression of adolescent idiopathic scoliosis in girls. J Pediatr Orthop B 2005;14:320–4.


3. Jiang J, Qiu Y, Mao S, Zhao Q, Qian B, Zhu F. The influence of elastic orthotic belt on sagittal profile in adolescent idiopathic thoracic scoliosis: a comparative radiographic study with Milwaukee brace. BMC Musculoskelet Disord 2010;11:219.




4. Shah SA. Nonoperative treatment for adolescent idiopathic scoliosis. Semin Spine Surg 2015;27:27–32.

5. Bidari S, Kamyab M, Ahmadi A, Ganjavian MS. Effect of exercise on static balance and Cobb angle during the weaning phase of brace management in idiopathic scoliosis and hyperkyphosis: a preliminary study. J Back Musculoskelet Rehabil 2019;32:639–46.


6. Weinstein SL, Dolan LA, Wright JG, Dobbs MB. Effects of bracing in adolescents with idiopathic scoliosis. N Engl J Med 2013;369:1512–21.



7. Diab R, Abdallah A, Embaby E. Spinopelvic alignment with SpineCor brace use in adolescent idiopathic scoliosis: an assessment. Int J Ther Rehabil 2017;24:83–8.

8. Catanzano AA Jr, Esposito VR, Dial BL, et al. Staying ahead of the curve: the use of spinopelvic parameters to predict curve progression and bracing success in adolescent idiopathic scoliosis. Spine Deform 2020;8:1213–22.



9. Saeedi M, Kamyab M, Babaee T, Behtash H, Ganjavian MS. The effects of bracing on sagittal spinopelvic parameters and Cobb angle in adolescents with idiopathic scoliosis: a before-after clinical study. Turk J Phys Med Rehabil 2020;66:452–8.



10. Berthonnaud E, Dimnet J, Roussouly P, Labelle H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech 2005;18:40–7.


11. Vergari C, Courtois I, Ebermeyer E, et al. Head to pelvis alignment of adolescent idiopathic scoliosis patients both in and out of brace. Eur Spine J 2019;28:1286–95.



12. Negrini S, Donzelli S, Aulisa AG, et al. 2016 SOSORT guidelines: orthopaedic and rehabilitation treatment of idiopathic scoliosis during growth. Scoliosis Spinal Disord 2018;13:3.




13. Page MJ, McKenzie JE, Bossuyt PM, et al. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg 2021;88:105906.


15. Stang A. Critical evaluation of the Newcastle-Ottawa scale for the assessment of the quality of nonrandomized studies in meta-analyses. Eur J Epidemiol 2010;25:603–5.



16. Margulis AV, Pladevall M, Riera-Guardia N, et al. Quality assessment of observational studies in a drug-safety systematic review, comparison of two tools: the Newcastle-Ottawa Scale and the RTI item bank. Clin Epidemiol 2014;6:359–68.


17. Wells GA, Shea B, O’Connell D, et al. The Newcastle-Ottawa scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Ottawa (ON): Ottawa Hospital Research Institute; 2011.
18. Donzelli S, Zaina F, Lusini M, et al. The three dimensional analysis of the Sforzesco brace correction. Scoliosis Spinal Disord 2016;11(Suppl 2): 34.




19. Lateur G, Grobost P, Gerbelot J, Eid A, Griffet J, Courvoisier A. Efficacy of nighttime brace in preventing progression of idiopathic scoliosis of less than 25°. Orthop Traumatol Surg Res 2017;103:275–8.


20. Zhang Z, Ma X, Yin J, et al. Alterations of sagittal alignment and thoracic cage parameters after long-term bracing in adolescents with idiopathic scoliosis. Orthop Traumatol Surg Res 2020;106:1257–62.


21. Fang MQ, Wang C, Xiang GH, Lou C, Tian NF, Xu HZ. Long-term effects of the Cheneau brace on coronal and sagittal alignment in adolescent idiopathic scoliosis. J Neurosurg Spine 2015;23:505–9.

22. Cheung J, Chong C, Cheung P. Underarm bracing for adolescent idiopathic scoliosis leads to flatback deformity: the role of sagittal spinopelvic parameters. Bone Joint J 2019;101-B:1370–8.

23. Almansour H, Pepke W, Bruckner T, Diebo BG, Akbar M. Three-dimensional analysis of initial brace correction in the setting of adolescent idiopathic scoliosis. J Clin Med 2019;8:1804.



24. Pepke W, El Zeneiny A, Almansour H, Bruckner T, Hemmer S, Akbar M. Influence of Cheneau-brace therapy on lumbar and thoracic spine and its interdependency with cervical spine alignment in patients with adolescent idiopathic scoliosis (AIS). J Clin Med 2021;10:1849.


25. Courvoisier A, Drevelle X, Vialle R, Dubousset J, Skalli W. 3D analysis of brace treatment in idiopathic scoliosis. Eur Spine J 2013;22:2449–55.




26. Ames CP, Blondel B, Scheer JK, et al. Cervical radiographical alignment: comprehensive assessment techniques and potential importance in cervical myelopathy. Spine (Phila Pa 1976) 2013;38(22 Suppl 1): S149–60.

27. Ames CP, Smith JS, Eastlack R, et al. Reliability assessment of a novel cervical spine deformity classification system. J Neurosurg Spine 2015;23:673–83.


28. Lamartina C, Berjano P. Classification of sagittal imbalance based on spinal alignment and compensatory mechanisms. Eur Spine J 2014;23:1177–89.



29. Bess S, Protopsaltis TS, Lafage V, et al. Clinical and radiographic evaluation of adult spinal deformity. Clin Spine Surg 2016;29:6–16.


30. Karandikar N, Vargas OO. Kinetic chains: a review of the concept and its clinical applications. PM R 2011;3:739–45.



31. Ling FP, Chevillotte T, Leglise A, Thompson W, Bouthors C, Le Huec JC. Which parameters are relevant in sagittal balance analysis of the cervical spine?: a literature review. Eur Spine J 2018;27(Suppl 1): 8–15.



32. Patwardhan AG, Khayatzadeh S, Havey RM, et al. Cervical sagittal balance: a biomechanical perspective can help clinical practice. Eur Spine J 2018;27(Suppl 1): 25–38.



33. Protopsaltis TS, Ramchandran S, Tishelman JC, et al. The importance of C2 slope, a singular marker of cervical deformity, correlates with patient-reported outcomes. Spine (Phila Pa 1976) 2020;45:184–92.


34. Xing R, Liu W, Li X, Jiang L, Yishakea M, Dong J. Characteristics of cervical sagittal parameters in healthy cervical spine adults and patients with cervical disc degeneration. BMC Musculoskelet Disord 2018;19:37.




35. Choi BW, Park JB, Kang JW, Kim DG, Chang H. Influence of atlantoaxial fusion on sagittal alignment of the occipitocervical and subaxial spines in os odontoideum with atlantoaxial instability. Asian Spine J 2019;13:556–62.




36. Protopsaltis T, Bronsard N, Soroceanu A, et al. Cervical sagittal deformity develops after PJK in adult thoracolumbar deformity correction: radiographic analysis utilizing a novel global sagittal angular parameter, the CTPA. Eur Spine J 2017;26:1111–20.



37. Shetty AP, Suresh S, Aiyer SN, Kanna R, Rajasekaran S. Radiological factors affecting post-operative global coronal balance in Lenke 5 C scoliosis. J Spine Surg 2017;3:541–7.



38. Newton PO, Faro FD, Gollogly S, Betz RR, Lenke LG, Lowe TG. Results of preoperative pulmonary function testing of adolescents with idiopathic scoliosis: a study of six hundred and thirty-one patients. J Bone Joint Surg Am 2005;87:1937–46.

39. Kearon C, Viviani GR, Kirkley A, Killian KJ. Factors determining pulmonary function in adolescent idiopathic thoracic scoliosis. Am Rev Respir Dis 1993;148:288–94.


40. Upadhyay SS, Mullaji AB, Luk KD, Leong JC. Relation of spinal and thoracic cage deformities and their flexibilities with altered pulmonary functions in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 1995;20:2415–20.


41. Lafage V, Schwab F, Skalli W, et al. Standing balance and sagittal plane spinal deformity: analysis of spinopelvic and gravity line parameters. Spine (Phila Pa 1976) 2008;33:1572–8.

42. Roussouly P, Gollogly S, Berthonnaud E, Dimnet J. Classification of the normal variation in the sagittal alignment of the human lumbar spine and pelvis in the standing position. Spine (Phila Pa 1976) 2005;30:346–53.


43. Legaye J, Duval-Beaupere G, Hecquet J, Marty C. Pelvic incidence: a fundamental pelvic parameter for three-dimensional regulation of spinal sagittal curves. Eur Spine J 1998;7:99–103.




44. Le Huec JC, Aunoble S, Philippe L, Nicolas P. Pelvic parameters: origin and significance. Eur Spine J 2011;20(Suppl 5): 564–71.




45. Betsch M, Rapp W, Przibylla A, et al. Determination of the amount of leg length inequality that alters spinal posture in healthy subjects using rasterstereography. Eur Spine J 2013;22:1354–61.




46. Zeng Z, Hai Y, Bi Y, Wang B, Liu M, Liu Y. Characteristics of sagittal spinopelvic alignment in asymptomatic Han Chinese adults. Exp Ther Med 2018;16:4107–13.



47. Mac-Thiong JM, Labelle H, Berthonnaud E, Betz RR, Roussouly P. Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J 2007;16:227–34.




48. Roussouly P, Pinheiro-Franco JL. Biomechanical analysis of the spino-pelvic organization and adaptation in pathology. Eur Spine J 2011;20(Suppl 5): 609–18.




49. Vrtovec T, Janssen MM, Likar B, Castelein RM, Viergever MA, Pernus F. A review of methods for evaluating the quantitative parameters of sagittal pelvic alignment. Spine J 2012;12:433–46.


50. Yang M, Yang C, Xu Z, et al. Role of T1 pelvic angle in assessing sagittal balance in outpatients with unspecific low back pain. Medicine (Baltimore) 2016;95:e2964.



51. Legaye J, Duval-Beaupere G. Sagittal plane alignment of the spine and gravity: a radiological and clinical evaluation. Acta Orthop Belg 2005;71:213–20.

52. Shigematsu H, Cheung JP, Bruzzone M, et al. Preventing fusion mass shift avoids postoperative distal curve adding-on in adolescent idiopathic scoliosis. Clin Orthop Relat Res 2017;475:1448–60.











