Management of Patients with Ischemic Heart Disease in Spine Surgery
Article information
Abstract
In ischemic heart disease (IHD), the myocardium does not receive enough blood and oxygen. Although the IHD-related mortality rate is decreasing, the risk remains and is a major predictor of cardiac complications following noncardiac surgery. Given the increase in the older population, the number of patients with spinal diseases requiring surgery is increasing. Among these patients, those with underlying IHD or a high risk of cardiac complications before and after surgery are also increasing. Given that cardiac complications following spinal surgery are associated with delayed patient recovery and even death, spinal surgeons should be knowledgeable about overall patient management, including medication therapy in those at high risk of developing perioperative cardiac complications for successful patient care. Before surgery, the underlying medical conditions of patients should be evaluated. Patients with a history of myocardial infarction should be checked for a history of surgical treatments, and the anticoagulant dose should be controlled depending on the surgery type. In addition, the functional status of patients must be examined before surgery. Functional status can be assessed according to the metabolic equivalent of task (MET). More preoperative cardiac examinations are needed for patients who are unable to perform four METs in daily because of the high risk of postoperative cardiac complications. Patients with a history of IHD require appropriate preoperative management and further postoperative evaluation. When considering surgery, spinal surgeons should be knowledgeable about patient care before and after surgery.
Introduction
In coronary heart disease, also called coronary-artery disease (CAD) or ischemic heart disease (IHD), the myocardium is not supplied with sufficient blood and oxygen. IHD can be classified into unstable angina pectoris caused by chronic CAD and acute coronary syndrome (ACS). ACS cases are divided into patients with unstable angina and those with acute myocardial infarction (MI). Moreover, patients with acute MI can be further classified into those with acute MI with or without ST-segment elevation based on electrocardiogram (ECG) findings [1–3].
Although the mortality rate of IHD is declining because of the development of various medical technologies, IHD still has the highest mortality rate worldwide [4]. Moreover, given the increase in the older population, the number of patients with spinal diseases and those undergoing spine surgery is rising [5,6].
IHD is a major predictor of cardiac complications following general noncardiac surgery [4,7]. Even among patients with a history of CAD who underwent spine surgery, IHD was associated with a high probability of developing MI following surgery [8].
Since the occurrence of cardiac complications following spine surgery can delay recovery and increase the likelihood of death, spinal surgeons who consider spine surgery for successful spinal care should have knowledge of the perioperative management of patients with IHD.
The 2014 American College of Cardiology (ACC)/American Heart Association (AHA) and European Society of Cardiology (ESC)/European Society of Anesthesiology (ESA) guidelines summarized the perioperative evaluation and management methodologies for patients undergoing noncardiac surgery. Several articles have also outlined the management of patients undergoing noncardiac surgery, including orthopedic surgery, among patients with underlying IHD [9,10]. However, no studies have provided the specific management of patients with IHD requiring spine surgery. Thus, this study performed a literature search to summarize the points to consider in patients with IHD requiring spine surgery, with a focus on the 2014 ACC/AHA guidelines, 2014 ESC/ESA guidelines, and their updated contents. The latest announcements related to cardiovascular complications before and after surgery for the above patient group were also summarized.
Materials and Methods
The management of cardiovascular complications in patients undergoing noncardiac surgery was mainly organized following the 2014 ACC/AHA guidelines, 2014 ESC/ESA guidelines, and their updated contents. Spinal surgery-related articles were searched in the Medline, Embase, and Google Scholar databases for articles published until April 2022.
Results
In this review, 355 articles discussed the management of perioperative risk when considering noncardiac surgery in patients with underlying IHD. Among them, 33 articles were selected in the summary (Fig. 1).
1. Preoperative management
1) Identification of underlying conditions
Various factors among the latest predictors related to the risk of developing cardiovascular complications before and after noncardiac surgeries are summarized in Table 1 [5,7,11,12]. Spinal surgeons treating patients with underlying IHD must broadly examine not only IHD but also insulin-dependent diabetes, other cardiac diseases, kidney diseases, cerebrovascular diseases, and preoperative anemia. If spine surgery is required for these underlying conditions, cardiac risk calculation may be used to alert patients to the potential for cardiovascular complications before and after the surgery.
2) Review of IHD medical history, symptoms, and functional status
The incidence of major cardiac complications following noncardiac surgery is associated with a history of CAD. The longer the time between the occurrence of MI and noncardiac surgery, the lower the postoperative rate of MI. Noncardiac surgeries in patients with a history of MI who have not undergone coronary revascularization surgery should be performed >60 days following MI to reduce the risk of cardiovascular complications before and after the surgery [7].
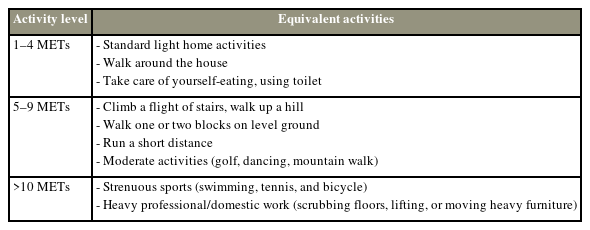
The preoperative functional status assessment of patients allows for the prediction of the risk of developing perioperative and long-term cardiovascular complications. This assessment can be referenced when deciding whether to add a stress test during elective surgery [7]. Functional abilities, also known as exercise tolerance, can be expressed as the metabolic equivalent of task (MET).
One MET is the basal oxygen consumption, or oxygen consumed at rest, of a 40-year-old 70-kg man. Functional ability is categorized as excellent (>10 METs), good (7–10 METs), moderate (4–6 METs), poor (<4 METs), or unknown. Patients unable to perform four METs daily have increased risks of postoperative heart and organ diseases. Patients unable to climb stairs, climb hills, walk at 4 miles per hour on flat surfaces, or do heavy house chores may have high risks of cardiac complications before and after surgery; thus, preoperative examination and preparation are crucial [7,9,10] (Table 2).
Spinal surgeons must review the functional level and symptoms of patients before deciding on spinal surgery and consider additional explanations and tests in patients who show IHD-related symptoms because of the high risk of developing perioperative cardiac events in patients who (1) had a history of unstable angina or recent acute MI, (2) were unable to perform activities of ≥4 METs, or (3) exhibited preoperative IHD symptoms such as chest pain and difficulty breathing, which have the highest correlation with major cardiac complications.
3) Preoperative cardiac examination
To screen for heart conditions such as IHD, arrhythmia, and left ventricular failure, preoperative cardiac tests are usually conducted using a resting 12-lead and exercise ECG. In addition, noninvasive cardiac investigations, such as pharmacological stress testing and dobutamine stress echocardiogram (DSE), can be applied. In 2019, Bovonratwet et al. [5] described DSE to measure the risk of cardiovascular complications in patients scheduled for spine surgery with a high risk for such complications.
The 2014 ACC/AHA guidelines discourage routine preoperative coronary angiography, noting that the indications for preoperative coronary angiography are generally similar to those identified in non-surgical situations [7]. Spinal surgeons should know about the additional tests needed for patients at high risk of perioperative cardiac events and must explain them to patients in advance.
2. Perioperative revascularization and timing of surgery
In patients with underlying IHD scheduled for spine surgery, the type of revascularization surgery, stent used in the revascularization surgery, and antiplatelet drug used following the surgery should be checked depending on whether revascularization surgery was performed at the time of MI occurrence. By contrast, patients at high risk of a perioperative cardiac event scheduled for spine surgery may require prophylactic revascularization before the surgery. These cases need appropriate management by checking the type of revascularization and the stent used [7].
To alleviate coronary vessel obstruction, percutaneous coronary intervention, which refers to balloon angioplasty or atherectomy, is performed commonly with the simultaneous use of a coronary stent. Two coronary stents are currently used clinically: the bare-metal stent (BMS), which is made of stainless steel or cobalt chromium, and the drug-eluting stent (DES), which is designed to deliver drug to the coronary vessels. When using a stent, the potential side effects of thrombus formation, which causes severe morbidity and mortality, should be considered. Stent thrombosis can be prevented through dual antiplatelet therapy (DAPT), which involves the use of dual antiplatelet agents, including aspirin and P2Y12 inhibitor inhibitors (clopidogrel, ticagrelor, and prasugrel) in patients with coronary-artery stents [13,14].
In patients who have undergone BMS, antiplatelet therapy can be discontinued after maintenance for at least 4–6 weeks. In the case of DES, DAPT is recommended for at least 12 months, and non-urgent noncardiac surgeries should be postponed during this period. For patients likely to require invasive or surgical procedures within 12 months following procedure, BMS implantation or balloon angioplasty should be considered instead of DES [7].
3. Perioperative medication management
Patients with underlying IHD are administered antiplatelet agents, beta-blockers, renin–angiotensin–aldosterone system (RAAS) inhibitors, calcium channel blockers, nitrates, and lipid-lowering medications [1]. In addition to the above, spine surgeons considering spine surgery should check all other medications taken by the patient and should provide the necessary patient education before the surgery.
First, the use of antithrombotic agents is the most closely related to surgery. The 2018 second Stent and Surgery Consensus statement report suggested that the risks of bleeding and thrombus formation should be considered to determine the timing of performing the surgery and discontinuing and resuming the antithrombotic medications depending on the type of surgery. According to this report, major spine surgery among orthopedic surgeries is classified as having a moderate risk of bleeding [14]. In orthopedic surgery with a typical moderate risk of bleeding, aspirin is usually maintained when adjusting for antithrombotic agents. P2Y12 inhibitors, such as clopidogrel, should be discontinued 5 days before surgery and resumed at an effective dose within 24–72 hours after surgery. The discontinuation of anticoagulants such as non-vitamin K-antagonist oral anticoagulants is recommended 24–96 hours before surgery and resumed 48–72 hours after surgery [15]. In 2019, Epstein [16] summarized the discontinuation days of anticoagulant, antiplatelet, and non-steroidal anti-inflammatory drugs (NSAIDs) before the spine surgery. They suggested discontinuing warfarin 5 days before surgery, and apixaban, a factor Xa inhibitor, 2 days before surgery. Rivaroxaban should be discontinued 3 days before the surgery, and aspirin should be discontinued for 7–10 days before the surgery. Finally, clopidogrel should be discontinued 5 days before the surgery, and NSAIDs should be discontinued for 1–10 days, depending on the drug [16]. It is important not only to discontinue anticoagulants before the surgery but also to restart their administration after the surgery. Furthermore, administering clopidogrel at a loading dose after the surgery is encouraged.
The dosage control of aspirin differs in medication management between surgery with a general moderate risk of bleeding and spine surgery. Continuous use before and after surgery is recommended for surgery with a moderate risk of bleeding [17]. However, earlier discontinuation of medication is suggested to prevent the development of postoperative epidural hematoma and paralysis symptoms in spine surgery [17,18]. Some studies have suggested that aspirin therapy is relatively stable in patients with spine surgery before and after surgery [19]; thus, the results of future studies may lead to the revision of guidelines regarding aspirin use.
Spine surgeons should also know about medications classified as appropriate to use continuously before and after the surgery, including beta-blockers, statins, and RAAS inhibitors. Beta-blockers are used to relieve symptoms and reduce the risk of MI and death in patients with stable IHD (Table 3). They also lower myocardial oxygen demand by reducing the heart rate, ventricular contractility, and systemic blood pressure. According to the 2014 ACC/AHA guidelines for statins, (1) statin administration should be continued for patients who are currently taking statins and scheduled for noncardiac surgery, (2) it may be reasonable to start administering statins before and after the surgery in patients undergoing vascular surgery, and (3) patients scheduled for high-risk surgery should be administered statins following guideline-directed medical therapy before and after the surgery. RAAS inhibitor therapy includes angiotensin-converting enzyme inhibitors (ACEI) and angiotensin receptor blockers (ARBs). According to the 2014 ACC/AHA guidelines, (1) the perioperative use of ACEIs or ARBs may be reasonable, and (2) if ACEIs or ARBs are discontinued before the surgery, it is logical to restart treatment when it is postoperatively feasible. RAAS inhibitor therapy is recommended to prevent MI or death in patients with IHD [7].
Finally, NSAIDs, commonly used for spinal and joint pains, increase the risk of MI or death in patients with IHD and are generally recommended to be avoided [20]. However, this rule is not implemented very well in reality. In 2020, Yang et al. [21] reported a relatively high incidence of postoperative gastrointestinal and cardiovascular complications in patients undergoing spine surgery; therefore, more attention should be paid to selecting appropriate NSAIDs for postoperative pain or symptoms that persist after the surgery.
4. Perioperative surveillance
Several studies have reported that cardiac complications occur in 0.21%–6.7% of cases following spine surgery [5,22–24]. MI was suggested as a main factor for readmissions within 90 days after spine surgery [25–28]; thus, even when spine surgery is performed successfully, postoperative management is crucial for patients with underlying IHD. Spinal surgeons should consider the occurrence of IHD, such as MI, even after surgery completion.
The 2014 ACC/AHA guidelines recommend (1) measuring troponin I levels or (2) taking an ECG if any signs or symptoms are suggestive of myocardial ischemia or MI [7]. Whether cardiac complications occur following spine surgery must be decided early by monitoring signs of cardiovascular ischemia in patients with continuous ECG and checking any troponin I elevations. The mortality rate resulting from cardiac complications following spine surgery may be reduced by implementing these appropriate measures in the event of cardiac complications.
Discussion
Several studies have discussed the preoperative assessment and perioperative management when considering noncardiac surgery in patients with underlying IHD [9,29,30]. However, these studies have limitations because they were based on previous guidelines and did not pertain only to spine surgery. The present study is meaningful in that it summarized the management of patients with IHD who are scheduled for spine surgery, unlike patients with IHD who are considering noncardiac surgery or orthopedic surgery.
Several studies have reported risk factors for cardiovascular complications following spine surgery, including old age, diabetes, underlying heart disease, and anemia [5,11,24,31–33]. In 2021, Ton et al. [34] reported valid factors among modifiable risk factors (MRFs) for postoperative complications in 297,579 patients who underwent lumbar spine fusion surgery. The MRFs included alcohol use, tobacco and nicotine use, malnutrition, dyslipidemia, and primary hypertension. Among these MRFs, patients with dyslipidemia showed a remarkably high incidence of MI within 90 days following lumbar fusion [34]. In some cases, pre-/perioperative management is not possible in patients with a history of IHD. In situations requiring emergency surgery, such as spinal cord injury or cauda equina syndrome, surgical treatment should be preceded to enhance the overall prognosis of patients despite the high risk of heart-related complications. Anticoagulant-related bleeding tendency is high; thus, volume control and additional blood transfusion may be required after the surgery.
In patients with underlying IHD scheduled for spine surgery, checking correctable factors, including dyslipidemia, and adjusting them in advance will reduce cardiovascular complications after the surgery.
Patients with a history of IHD need adequate preoperative care and a cautious preoperative evaluation. Regarding patient care, additional tests are needed in patients considered at high risk for heart-related complications before and after surgery by identifying not only IHD history but also other related underlying conditions and assessing the preoperative symptoms and functional status of the patient.
Conclusions
Spinal surgeons are encountering an increasing number of patients with underlying IHD. These patients are at significantly higher risk for perioperative morbidity and mortality. To minimize cardiac complications for spine surgery and promote the rapid recovery of patients after the surgery, spinal surgeons should be aware of the overall management direction of patients with IHD. In addition, patients at risk of cardiac complications should not be missed, and the need for cardiac counseling should be determined for optimal preoperative and postoperative management. Preoperatively, the patient’s underlying disease and medications must be accurately evaluated, and for patients with underlying IHD, measures such as functional status evaluation and anticoagulant dosage adjustment are required to reduce the risk of cardiac complications before and after the surgery. Depending on the type of anticoagulants used, the recommended discontinuation period before surgery may differ. Cardiac complications must be detected early after spinal surgery using cardiac markers and ECG monitoring.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Funding
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education (No., RS-2023-00246711) and the Korea government (MSIT). (No., 2021R1F1A1059969).
Author Contributions
Conceptualization: DHK, SYS; data curation: MGS, CWK; formal analysis: MGS, CWK; funding acquisition: DHK, SYS; methodology: MGS; project administration: DHK; visualization: CWK, SYS; writing–original draft: MGS, HGK; writing–review & editing: CWK, HGK; and final approval of the manuscript: all authors.