|
 |
- Search
| Asian Spine J > Volume 18(1); 2024 > Article |
|
Abstract
Study Design
A newly proposed scoring tool was designed to assist in the clinical management of adult thoracolumbar spinal tuberculosis (TB).
Purpose
To formulate a comprehensive yet simple scoring tool to guide decision-making in the management of adult thoracolumbar spinal TB.
Overview of Literature
Spine surgeons have differing consensus in defining the threshold grade for clinico-radiological parameters when deciding between operative or conservative treatment for adult thoracolumbar spinal TB. Currently, the void in decision-making from the lack of well-defined guidelines is compensated by the surgeon’s experience in treating these patients. To the best of our knowledge, no scoring system holistically integrates multiple facets of spinal TB to guide clinical decision-making.
Methods
The RAND/University of California, Los Angeles appropriateness method was employed among an expert panel of 10 spine surgeons from four apex tertiary care centers. Vital characteristics that independently influenced treatment decisions in spinal TB were identified, and a scoring tool was formulated. Points were assigned for each component based on their severity. The cutoff scores to guide clinical management were determined from the receiver operating characteristic curve based on the retrospective records of 151 patients treated operatively or non-operatively with improved functional outcomes at the 1-year follow-up.
Results
The components of the comprehensive spinal TB score (CSTS) are pain, kyphosis angle, vertebral destruction, and neurological status. A score classification of <5.5, 5.5–6.5, and >6.5 was established to guide the patient toward conservative, conservative/operative, and operative management, respectively.
Conclusions
The CSTS was designed to reflect the essential indicators of mechanical stability, neurological stability, and disease process stabilization in spinal TB. The scoring tool is devised to be practical and serve as a common language in the spine community to facilitate discussions and decision-making in thoracolumbar spinal TB. The validity, reliability, and reproducibility of this tool must be assessed through multicenter long-term studies.
Tuberculosis (TB) is an endemic disease of the developing world and contributes substantially to the socioeconomic and healthcare burden of the nation. Extrapulmonary TB accounts for 3% of the total TB burden, with spinal TB alone contributing to 50% of osteoarticular TB cases [1,2]. The endemicity of spinal TB poses a broad spectrum of presentations, including complicated spinal TB patterns and atypical presentations. This has eluded researchers from creating a comprehensive classification encompassing the entire spinal TB spectrum to guide clinical management [3]. The success of multidrug chemotherapy and observations of the Medical Research Council (MRC) trial led to the introduction of the “middle path regimen” where surgical intervention was reserved for only a subset of patients being primarily treated with anti-tubercular therapy (ATT) [4,5]. The indications for surgery were the lack of response to chemotherapy, recurrent diseases, severe neurological deficit, static or progressive neurological deficit on ATT, deformity, debilitating pain, and instability. These clinicoradiological entities have been described in isolation but often exist in combination with varying grades of severity. Spine surgeons have differing consensus in defining the threshold grade for these clinicoradiological parameters when deciding between operative or conservative treatment. Currently, the void in decision-making from the lack of well-defined guidelines is compensated by the surgeon’s experience in treating these patients. Thus, to assist clinical decision-making, a scoring system that holistically includes these clinicoradiological entities and gives due weighting to their severity strata is needed.
To our knowledge, no scoring system holistically integrates multiple facets of spinal TB to guide management. Thus, this study was undertaken to formulate a comprehensive score to assist clinical decision-making by observing the treatment response in cases of spinal TB.
The RAND/University of California, Los Angeles appropriateness method was used to establish a consensus on the factors and their weighting for a scoring system designed to guide management in adult thoracolumbar spinal TB. A review of English literature was conducted using PubMed, Scopus, and Embase. All relevant articles pertaining to the management of thoracolumbar spinal TB with multiple citations and popularity among the spine community were reviewed by the lead author to prepare a survey questionnaire consisting of open-ended questions. Ten fellowship-trained spine surgeons from four apex tertiary care centers were surveyed to find common ground among treatment algorithms for all stages of spinal TB and identify clinical and radiological characteristics that independently played a vital role in clinical decision-making.
Based on the survey response, a preliminary scoring instrument (PSI) was drafted to encompass pivotal clinicoradiological characteristics that guided decision-making. The PSI was subjected to four rounds of appropriateness rating, with a non-anonymized discussion between the rounds. Through these rounds, the PSI was scrutinized to address existing loopholes, include missing vital factors, omit less relevant factors, and make modifications in the scoring stratification. During these rounds, the experts rated the factors and their severity scores on the 9-point appropriateness scale. The factors with median scores in the 1–3 range were classified as “inappropriate,” 4–6 as “uncertain,” and 7–9 as “appropriate.” A median of 3.5 or 6.5 was considered in the higher appropriateness category, i.e., 4–6 and 7–9, respectively. “Disagreement” occurred when ≥3 panelists provided ratings in each extreme (1–3 and 7–9). However, all indications rated “with disagreement,” whatever the median, were classified as “uncertain.” Through an iterative process, terminologies and the weighting of scores allotted to the severity strata were modified for various criteria through the rounds. Only those factors with a median rating of ≥7 with “no disagreement” of consensus among the experts in the fourth round were incorporated into the scoring system. Conversely, factors with a median rating of <7 or rated “with disagreement” of consensus in the fourth round were eliminated [6]. The final scoring tool, i.e., the comprehensive spinal TB score (CSTS), was then applied to different case scenarios to address any remaining limitations, and necessary modifications were made before unanimously agreeing to it.
The scoring tool was then applied retrospectively against a cohort of 151 adult patients with thoracolumbar spinal TB who had been managed at the institute between 2017 and 2021 (Table 1). All 151 patients had been managed operatively or non-operatively as deemed appropriate by the lead author and showed significant improvements in the Visual Analog Scale (VAS), Oswestry Disability Index, Frankel’s grading, and muscle power analysis at 1-year follow-up; thus, management received by this cohort was referenced as the gold standard. The retrospective scores obtained were then plotted against the operative or non-operative management received by these patients in a receiver operating characteristic (ROC) curve to know the utility of the TB score for the prediction of management and determine cutoff scores to guide clinical decision-making.
The approval of Ethics Committee of Grant Government Medical College and Sir JJ Group of Hospitals, Mumbai was obtained for this study (IRB approval no., IEC/PG/437/June/2021). Written Informed consent was obtained from the patients for participation in the study and for publication of the data emerging from it.
The classification was built using four major components that were rated “appropriate”: pain, kyphosis angle, vertebral body destruction, and neurological deficit secondary to a compressive element. The individual components were scored in order of their increasing severity. A higher sum of the individual component scores weighed in favor of operative management. The following factors were rated either “uncertain” or “inappropriate” and rejected during the formulation of the scoring system (Table 2).
Pain is the most common symptom of spinal TB and can be debilitating sometimes. The pain severity was quantified using the VAS score. The VAS was split into three segments of increasing order of severity, and the score segments 1–3, 4–6, and 7–10 were assigned 1, 1.5, and 2 points, respectively.
Angular kyphosis due to tubercular spinal destruction disturbs the biomechanics of the spine and affects global sagittal balance. The nonphysiological loading of spinal elements can result in the progression of deformity, decompensated spinal balance, late-onset neurological deficit, mechanical back pain, and adjacent segment degeneration. Any angulation in the spine <30° is well tolerated and hence assigned 0 points [7,8]. Further kyphosis of 30°–49°, 50°–80°, and >80° were assigned 1, 2, and 3 points, respectively. The junctional levels in the spine are subject to higher loads than other spinal regions and hence qualify for an additional 1 point.
Vertebral destruction leads to angular collapse, shortening, and induces spinal column instability. An increasing number of vertebrae or spinal column destruction correlates well with a proportionate rise in spinal TB-related complications. Contiguous levels of partial vertebral body destruction were summed up into vertebral equivalents to quantify destruction better. Equivalents were calculated by eyeballing the imaging studies. Vertebral equivalents of <1, 1–2, 3, and ≥4 were scored 1, 2, 3, and 4 points, respectively. The posterior column acts as a spinal tension band, and its involvement qualifies for an additional 1 point.
Neurological insult is the most dreaded complication of spinal TB and adds to significant functional disability and dependency. Milder grades of neurological deficit result from edema, inflammatory cells, caseous material, or early granulation tissue and respond well to conservative management with ATT. Higher grades of neurological deficit have an inflammatory component along with mechanical compression caused by sequestrated bone or disc, thick fibrous bands, and bony bridges [9]. Therefore, scoring of the neurological status was done only in cases with concomitant spinal cord compression on magnetic resonance imaging (MRI) and was not extended to noncompressive neurological deficits. Neurological status was classified as normal, exaggerated reflexes or myelopathy without paresis, unaided ambulation with paresis, aided ambulation, and non-ambulatory were assigned 0, 1.5, 2, 3, and 4 points, respectively (Table 3).
The total score represents the severity of tubercular involvement of the spine, is determined by adding individual component scores, and ranges from 0 to 15. The principles of management in cervical, sacral, and pediatric spinal TB differ from the thoracolumbar region; thus, this scoring system should not be extended to them. In cases of multifocal involvement, each contiguous segment must be considered separately and managed according to its score. As patients with spinal TB undergo prolonged treatment with ATT, the scoring instrument must be utilized at various points to guide decision-making accordingly.
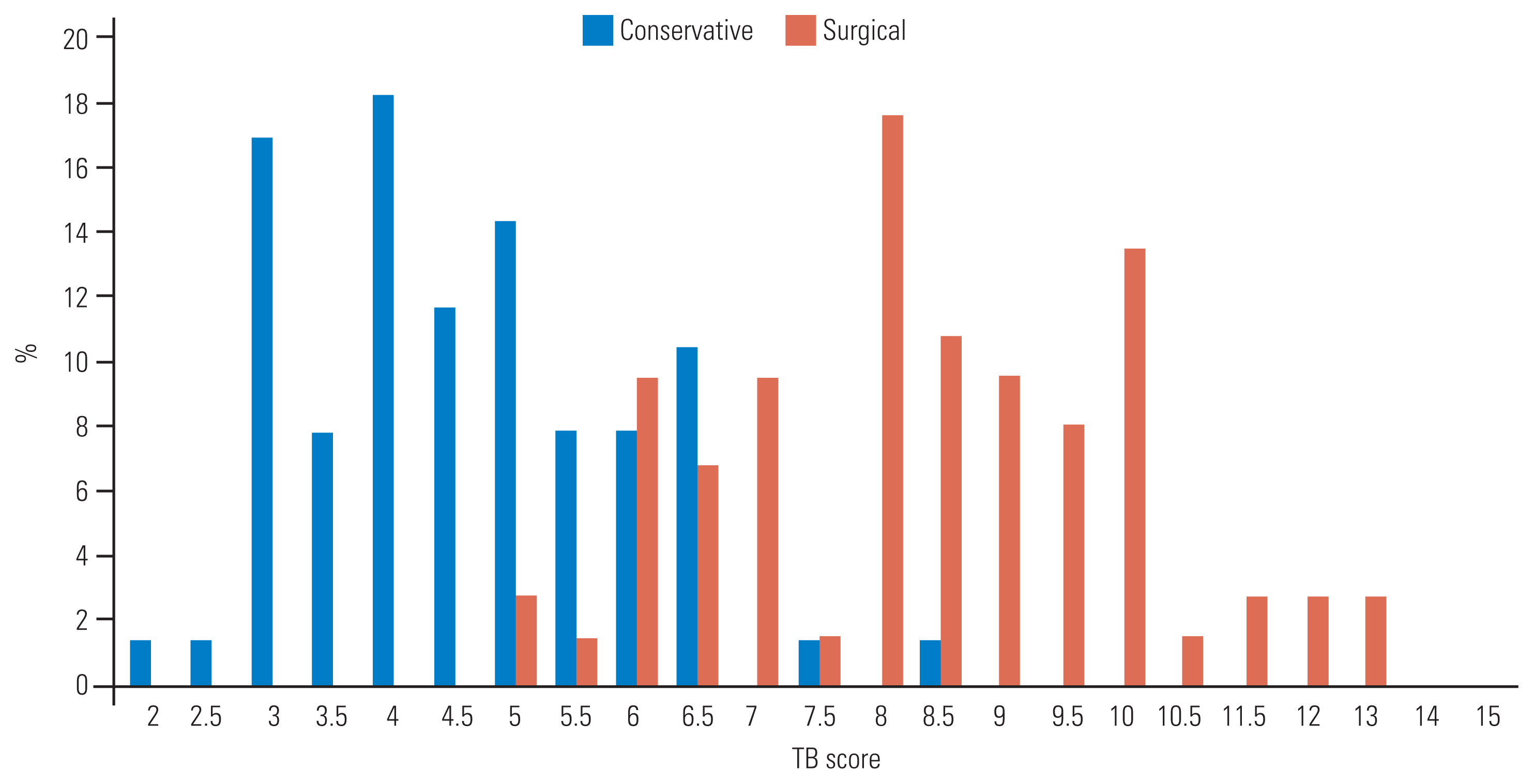
TB scores and the line of management received were studied. Most patients (n=62, 41.1%) had scores of 3.5–6, followed by 51 patients (33.8%) with scores of 6.5–9. Moreover, 21 patients (13.9%) had a score of 9.5–12, 15 (9.9%) had a score of 0–3, and two patients (1.3%) had a score of >12.5. The analysis of the CSTS distribution among the two groups using the chi-square test showed that patients with a lower score (mean 4.58±1.29) were managed well conservatively, whereas patients with a higher score (mean 8.40±1.78) were managed surgically. A significant association was established between the TB score and treatment modality (p<0.001) (Table 4).
Most patients with a score <5.5 had been treated conservatively, except for 2 patients (1.3%), who had a score of 5.0 and were treated operatively. Likewise, most patients with a score of >6.5 had received operative management. Two patients (1.3%) with a score of 7.5 and 8.5 were conservatively managed as they were not fit for surgery. A significant overlap in treatment modalities was seen from a score of 5.5–6.5; this overlapping area was termed an ambiguous zone. Of 26 patients (17.2%) lying in the ambiguous zone, 14 (18.2%) were managed conservatively, whereas 12 (16.2%) had undergone surgery (Fig. 1). The ROC curve was plotted to determine the cutoff between the operative and conservative groups with an area under the ROC curve of 0.96 (p<0.001). The sensitivity and specificity at a cutoff score of 5.5 were 95.9% and 79.2%, respectively. Similarly, the sensitivity and specificity at a cutoff score of 6.5 were 79.7% and 97.4%, respectively (Fig. 2, Table 5).
The CSTS is calculated by summing up the individual component scores with a score ranging from 0 to 15. By drawing an inference from the above data and analysis, we propose managing patients with scores <5.5 conservatively, scores of 5.5–6.5 of the ambiguous zone should be managed on an individual case basis at the discretion of the treating surgeon, and patients receiving a score of >6.5 should be managed surgically.
Despite the advances in spinal TB, certain clinical states pose a management dilemma. The existence of differing opinions among experts on the subject of spinal TB is proof of its complexity. Existing classifications do not look holistically into spinal TB, and the lacunae in these classifications represent the intricacies of the ever-evolving understanding of spinal TB.
The MRC trials that began in 1963 helped establish the acceptance of ambulatory chemotherapy as equally effective to radical debridement for treating spinal TB [10,11]. In 1975, the introduction of “middle path regimen” by Tuli [12] was a landmark event and formed the basis for most guidelines on managing spinal TB. Surgery was offered in cases with paraplegia, severe neurological deficits, and for patients who did not respond or worsened on a fair trial of conservative therapy [12]. Although its introduction was deemed quite successful, it still involved months of recumbency over plaster beds and years of compliance with plaster jackets and spinal braces. The indications for surgery were clouded by the lack of specifics and a high threshold for surgical intervention was advocated. In this treatment algorithm, surgery had an adjuvant role in specific clinical scenarios of spinal TB.
In 1985, Kumar [13] described an exhaustive 4-point classification system based on the site, lesion stage, associated lesions, and functional deficit for posterior spinal TB. Similarly, Ahuja et al. [14] devised the TB spine instability score for predicting instability in patients with spinal TB and intact neurology. However, these classifications cater only a tiny subset of patients with spinal TB in the clinical setting.
In 2001, Mehta and Bhojraj [15] developed a surgical guide for managing spinal TB. The classification segregated lesions mainly based on MRI characteristics; it included column involvement, extent of deformity, cord compression, instability, and patient-related factors. This classification mainly focused on selecting appropriate surgical strategies in patients with spinal TB requiring operative management [15].
The Gulhane Askeri Tip Akademisi classification of spinal TB, developed in 2008, was not used extensively because it only considered anterior column involvement, neglecting the posterior elements and atypical spinal TB presentations [16]. The classification system also groups clinicoradiological features with increasing grades of severity into different classes. This description creates a rigid set of findings in each class, which is not flexible to accommodate the possibility of a varied combination of observations in a patient.
In 2016, Kumar [9] attempted to guide clinical management in spinal TB based only on the grade of neurological involvement. However, this classification attempts to simplify the disease by ignoring the structural integrity of the spinal column, patient’s deformity, and symptom complex [9]. Pain was the most common symptom of our reference cohort. Srinivasa et al. [17] and Su et al. [18] noted similar observations in their study of patients with spinal TB. Hence, this was considered one of the key components in framing the score.
None of the existing classification systems has had widespread acceptance. While some failed to capture the entire spectrum of spinal TB patterns, others were lopsidedly based on surgical protocols, site of lesions or grading of paraplegia [9,13,15,16]. With a better understanding of the pathophysiology of spinal TB, advancements in ATT, and spinal fixation devices, some of these classifications have become outdated.
By drawing similarities from the spinal stability model of the thoracolumbar injury classification and severity scoring system, stability in spinal TB can be viewed in three dimensions, i.e., mechanical stability, represented by vertebral body destruction and kyphosis angle; neurological stability, represented by neurological status; and disease process stabilization represented by resolution of pain [19]. The metrics governing these are independent of one another and holistically represent spinal stability. The current scoring system has limited ability to guide management in a rare clinical case of an epidural abscess causing severe cord compression and neurological deficit without significant pain, vertebral body destruction, and kyphosis, as the total score does not qualify it for surgical decompression. In addition, the non-inclusion of cervical and sacral spinal TB, atypical presentations, and pediatric and geriatric spinal TB in the study limits the use of this scoring system in such cases.
The comprehensive scoring system employs objectification of the critical characteristics and provides numerical grades in order of severity. The assimilated score of these critical features guides clinical decision-making in the order of conservative, conservative/operative, and operative management as the score increases. Various other factors must be considered while zeroing down on a clinical decision. Factors including but not limited to comorbidities, concomitant spinal pathologies, subjective aspects, age, and pregnancy influence the treatment and prognosis. These factors have been omitted to keep the score simple, objective, and sufficiently comprehensive. This scoring guide should supplement decision-making and not be used as a stand-alone criterion for proposing spinal TB management. Further, large-scale, multicenter studies are needed to assess intra and inter-observer reliability, reproducibility, and validity and narrow down the ambiguous zone of the CSTS. Finally, future developments in spinal TB will bring a better understanding of the disease entity, and scoring systems should subsequently incorporate modifications to improve the accuracy of clinical guidance.
Notes
Author Contributions
Conceptualization: DVS, SSK; methodology: DVS, SSK; formal analysis and investigation: DVS, SSK, HKP, MBP; writing–original draft preparation: SSK, HKP; writing–review and editing: DVS, SSK, HKP, SAJ, MBP; resources: SSK, HKP, AC, EP, SAJ, TPV; supervision: DVS, AC, EP, SAJ, STN, MBP; and final approval of the manuscript: all authors.
Fig. 2
Receiver operating characteristic (ROC) curve to predict the utility of comprehensive spinal tuberculosis (TB) score in guiding management of adult thoracolumbar spinal TB. Diagonal segments are produced by ties.
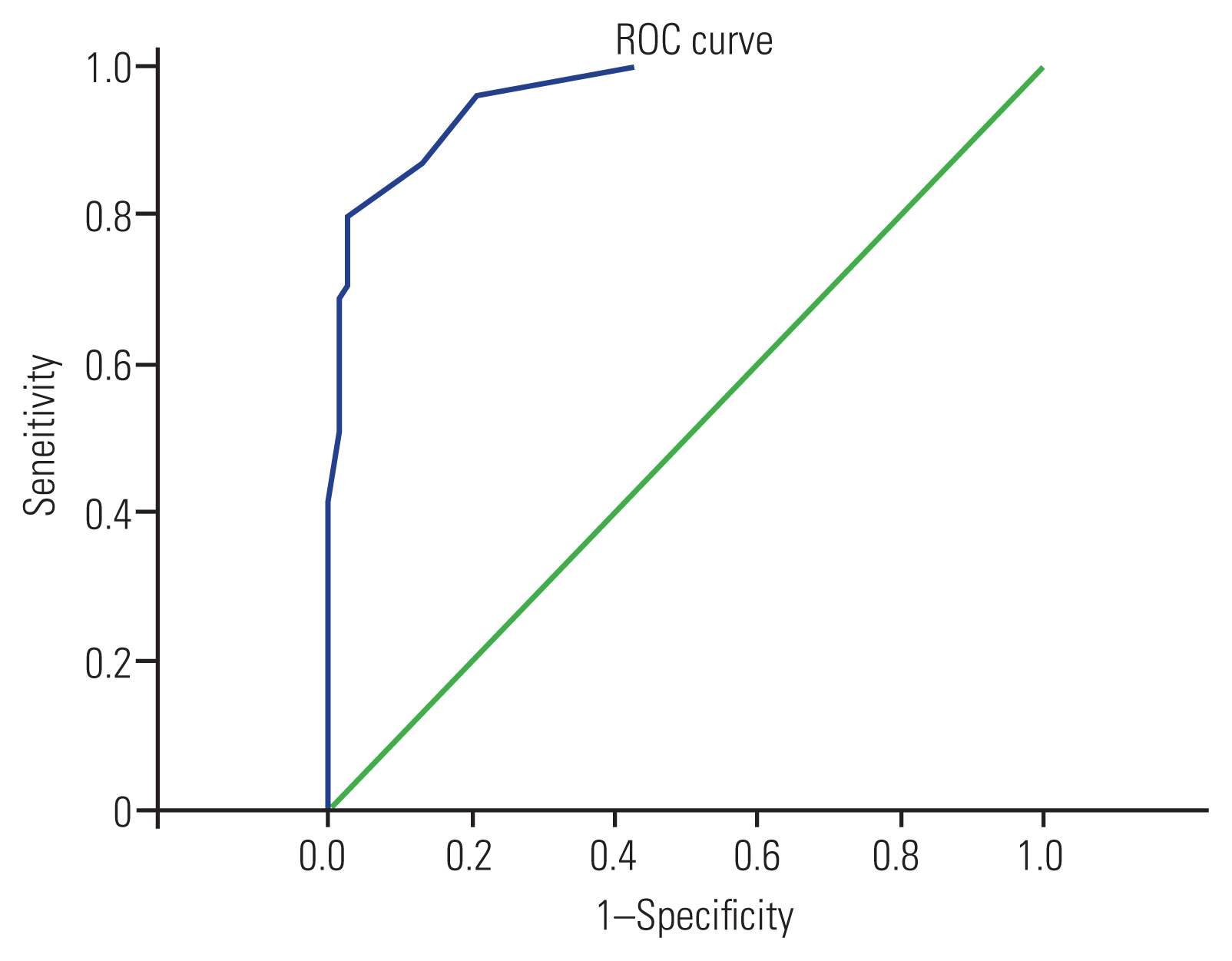
Table 1
Observations from the retrospective cohort of 151 managed cases of thoracolumbar spinal TB used as a gold standard reference for deducing the cut-off scores of comprehensive spinal TB score
| Variable | Value | p-value |
|---|---|---|
| Mean age of presentation (yr) | 36.9 | |
| Male:female ratio | 0.75:1 | |
| Male | 86 (57.0) | |
| Female | 65 (43.0) | |
| 21–30 yr (majority) | 40 (26.4) | |
| Operative group (N=74) | ||
| ODI | <0.001a) | |
| Preop | 80.1±10.5 | |
| Postop | 27.5±11.7 | |
| VAS | <0.001a) | |
| Preop | 7.2±2.1 | |
| Postop | 1.1±0.9 | |
| MRC | <0.001a) | |
| Preop | 25.3±18.7 | |
| Postop | 42.6±9.3 | |
| Frankel grade | <0.001b) | |
| A | ||
| Preop | 21 (28.4) | |
| Postop | - | |
| B | ||
| Preop | 6 (8.1) | |
| Postop | - | |
| C | ||
| Preop | 9 (12.2) | |
| Postop | 2 (2.7) | |
| D | ||
| Preop | 23 (31.1) | |
| Postop | 38 (51.4) | |
| E | ||
| Preop | 15 (20.3) | |
| Postop | 34 (45.9) | |
| Conservative group (N=77) | ||
| ODI | <0.001a) | |
| Preop | 53.8±15.2 | |
| Postop | 15.3±12.1 | |
| VAS | <0.001a) | |
| Preop | 5.4±2.5 | |
| Postop | 0.8±0.1 | |
| MRC | <0.001a) | |
| Preop | 46.9±7.8 | |
| Postop | 49.1±3.5 | |
| Frankel grade | <0.001b) | |
| A | ||
| Preop | 1 (1.3) | |
| Postop | - | |
| B | ||
| Preop | 1 (1.3) | |
| Postop | - | |
| C | ||
| Preop | 4 (5.2) | |
| Postop | - | |
| D | ||
| Preop | 71 (92.2) | |
| Postop | 3 (3.9) | |
| E | - | |
| Preop | - | |
| Postop | 74 (96.2) | |
Table 2
List of factors rated as ‘uncertain’ or ‘inappropriate’ using the RAND/University of California, Los Angeles appropriateness method
Table 3
Summary table including all elements of the comprehensive tuberculosis score
Table 4
Distribution of treatment modalities within multiple score classes of comprehensive spinal TB score
| Conservative | Surgical | Total | p-value | |
|---|---|---|---|---|
| TB score | ||||
| ≤3 | 15 (19.5) | - | 15 (9.9) | |
| 3.5–6 | 52 (67.5) | 10 (13.5) | 62 (41.1) | <0.001a) |
| 6.5–9 | 10 (13.0) | 41 (55.4) | 51 (33.8) | |
| 9.5–12 | - | 21 (28.4) | 21 (13.9) | |
| ≥12.5 | - | 2 (2.7) | 2 (1.3) | |
| Mean TB score | 4.58±1.29 | 8.40±1.78 | 6.45±2.46 | <0.001a) |
Table 5
Comparison of TB score between three score classes
| Conservative | Surgical | Total | p-value | |
|---|---|---|---|---|
| TB score | <0.001a) | |||
| <5.5 | 61 (79.2) | 2 (2.7) | 63 (41.7) | |
| 5.5–6.5 | 14 (18.2) | 13 (17.5) | 27 (17.8) | |
| >6.5 | 2 (2.6) | 59 (79.8) | 61 (40.5) |
References
1. Rajasekaran S, Soundararajan DC, Shetty AP, Kanna RM. Spinal tuberculosis: current concepts. Global Spine J 2018 8(4 Suppl): 96S–108S.




2. Kulchavenya E. Extrapulmonary tuberculosis: are statistical reports accurate? Ther Adv Infect Dis 2014 2:61–70.




4. A controlled trial of six-month and nine-month regimens of chemotherapy in patients undergoing radical surgery for tuberculosis of the spine in Hong Kong: tenth report of the Medical Research Council Working Party on Tuberculosis of the Spine. Tubercle 1986 67:243–59.


6. Fitch K, Bernstein SJ, Aguilar MD, et al. The RAND/UCLA appropriateness method user’s manual. Santa Monica (CA): RAND; 2001.
8. Rajasekaran S. Kyphotic deformity in spinal tuberculosis and its management. Int Orthop 2012 36:359–65.




9. Kumar K. Spinal tuberculosis, natural history of disease, classifications and principles of management with historical perspective. Eur J Orthop Surg Traumatol 2016 26:551–8.



10. A 15-year assessment of controlled trials of the management of tuberculosis of the spine in Korea and Hong Kong: thirteenth Report of the Medical Research Council Working Party on Tuberculosis of the Spine. J Bone Joint Surg Br 1998 80:456–62.

11. Mak KC, Cheung KM. Surgical treatment of acute TB spondylitis: indications and outcomes. Eur Spine J 2013 22(Suppl 4): 603–11.



12. Tuli SM. Results of treatment of spinal tuberculosis by “middle-path” regime. J Bone Joint Surg Br 1975 57:13–23.



13. Kumar K. A clinical study and classification of posterior spinal tuberculosis. Int Orthop 1985 9:147–52.



14. Ahuja K, Kandwal P, Ifthekar S, et al. Development of Tuberculosis Spine Instability Score (TSIS): an evidence-based and expert consensus-based content validation study among spine surgeons. Spine (Phila Pa 1976) 2022 47:242–51.

15. Mehta JS, Bhojraj SY. Tuberculosis of the thoracic spine: a classification based on the selection of surgical strategies. J Bone Joint Surg Br 2001 83:859–63.

16. Oguz E, Sehirlioglu A, Altinmakas M, et al. A new classification and guide for surgical treatment of spinal tuberculosis. Int Orthop 2008 32:127–33.




17. Srinivasa R, Furtado SV, Kunikullaya KU, Biradar S, Jayakumar D, Basu E. Surgical management of spinal tuberculosis: a retrospective observational study from a tertiary care center in Karnataka. Asian J Neurosurg 2021 16:695–700.