Lumbar Transforaminal Injection of Steroids versus Platelet-Rich Plasma for Prolapse Lumbar Intervertebral Disc with Radiculopathy: A Randomized Double-Blind Controlled Pilot Study
Article information
Abstract
Study Design
Double-blind randomized controlled pilot study.
Purpose
The purpose of this study was to compare outcomes of steroids with autologous platelet-rich plasma (PRP) administered by lumbar transforaminal injection (LTI) in patients with lumbar radiculopathy.
Overview of Literature
Degenerative disc disease of the lumbar spine is one of the most common conditions managed by spine surgeons in routine practice. Once conservative management fails, LTI is diagnostic and often therapeutic. Steroids are the gold standard drug used for LTI but have limitations and side effects.
Methods
In this single-center double-blind randomized controlled pilot study, 46 patients were recruited and randomized by the lottery method. The Visual Analog Scale (VAS) for leg pain, modified Oswestry Disability Index (mODI), and Short-Form 12 (SF-12) were assessed at 1 week, 3 weeks, 6 weeks, 6 months, and 1 year.
Results
Both groups were comparable in terms of demographics, preprocedure VAS scores, mODI, and SF-12 scores (p=0.52). At the 1-week follow-up, the steroid group had significantly better improvement than the PRP group (p=0.0001). At the 3-week follow-up, both groups showed comparable outcomes; however, the PRP group had better symptom improvement. At 6 weeks and 6 months, the PRP group had better outcomes (VAS, p<0.0001; ODI, p=0.02; SF-12, p=0.002). Moreover, 17 and 16 patients in the steroid and PRP groups underwent repeat LTI with steroids or surgery because of pain recurrence during follow-up. At 1 year, no difference in outcomes was observed.
Conclusions
PRP may be a useful alternative to steroids for LTI in lumbar radiculopathy. Although improvement was delayed and 1-year outcomes were comparable, the 6-week and 6-month outcomes were better with PRP than with LTI. Multiple PRP injections may be beneficial because of its autologous nature. However, further studies with a larger number of participants, longer follow-up, and repeat LTIs are warranted to draw definite conclusions.
Introduction
Chronic low back pain with or without lower extremity pain is one of the most common conditions encountered by spine surgeons [1]. Epidural injections are a common modality in managing chronic radicular leg pain and can be given by accessing the epidural space through different routes such as transforaminal, caudal, or interlaminar. Of these three routes, the transforaminal route is considered the best as it enables drug delivery close to the pathologic site, presumably onto the inflamed nerve root. Thus, a low amount of drugs is required [2]. Moreover, some authors have claimed that drug delivery directly at the anterior extradural space of the nerve root where the actual compression lies is possible [3,4].
The drugs used for transforaminal injections have been a topic of discussion. Specifically, steroids are the most commonly used drug, and among steroids, triamcinolone is the gold standard [5]. Other drugs that have shown promising results include steroids such as betamethasone, methylprednisolone, and etanercept [6], local anesthetics such as lignocaine and bupivacaine, and sodium hyaluronate/carboxymethyl cellulose solution [7]. Moreover, evidence showed positive results of using platelet-rich plasma (PRP) in treating discogenic back pain [8,9]. However, to the best of our knowledge, only one study has compared the outcome of lumbar transforaminal injections (LTIs) with steroids and PRP [10].
Thus, this study was conducted to compare the functional outcomes of steroids and PRP in patients with predominantly radicular pain caused by prolapse lumbar intervertebral disc (PIVD).
Materials and Methods
1. Study design and population
This double-blind randomized controlled pilot study was conducted at the Indian Spinal Injuries Center. The study was approved by the institutional ethics committee of Indian Spinal Injuries Center (Ref. ISIC/RP/2019/003). For being a pilot study, the sample size was calculated based on the “rule of 12” [11]. Two groups were employed: one group received injections of steroids (triamcinolone, steroid group) and PRP (prepared from the patient’s blood, PRP group) through the transforaminal route. The nature of the study was fully explained to all patients, and they provided informed consent before inclusion in the study. Patients aged >18 years and <60 years diagnosed with PIVD not responding to conservative management were included. PIVD was defined as those with radicular pain in the lower limb at a single dermatome and a positive straight leg-raising test correlating radiologically with findings of lumbar disc herniation/prolapse in the recent magnetic resonance imaging (MRI). Patients with pseudoradicular pain, red flags such as motor deficit or cauda equina syndrome, and history of spinal surgery of the affected segment, infiltration of the affected segment, spinal infection/spondylodiscitis, multilevel disc herniations, spinal/foraminal stenosis, myelopathy, spinal fracture, or coagulation disorders.
2. Platelet-rich plasma preparation
The PRP was prepared under sterile conditions in the operation theater using a standard PRP preparation kit. Specifically, 30 mL of blood was withdrawn from the patient, processed in the HARVEST Smart prep 2 machine to generate 3–5 mL of PRP in 15 minutes (Fig. 1), and then injected in the epidural space under sterile conditions.

Platelet-rich plasma (PRP) preparation. (A) Collection of blood from the patient. (B) Insertion of collected blood in PRP kit. (C) Kit insertion in Harvest Smart prep. (D) Final PRP formed.
For a double-blinded procedure, 30 mL of blood was withdrawn from all participants irrespective of the group; however, the blood of the steroid group was discarded. The preloaded syringe provided to the surgeon who performed the injection was covered with sterile autoclaved tapes. The same surgeon collected the data on all follow-ups, which were kept blind until after the statistical data analysis.
3. Procedure
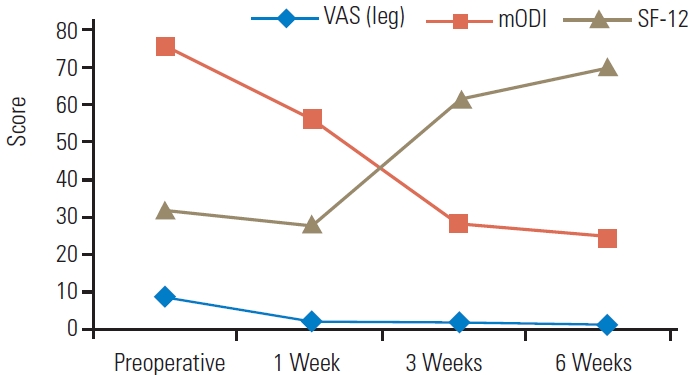
Randomization was done by the lottery method. After informed consent was obtained and the patient was placed in the prone position, the surgical area was prepped and draped. Thereafter, the C-arm was used to make the superior endplate of the respective of vertebra orthogonally (If L5 LTI was indicated, then the superior endplate of L5 was made orthogonal). Thereafter, the C-arm was rotated to visualize the Scotty dog view, and the foramen was targeted with a 22G spinal needle. First, a radiocontrast agent (Omnipaque; GE Healthcare, Chicago, IL, USA) was injected to confirm the accuracy of the needle position (Fig. 2); thereafter, 0.5 mL of 0.5% bupivacaine and 1 mL (40 mg) of steroid (triamcinolone) were injected in the steroid group, whereas 0.5 mL of 0.5% bupivacaine and 2 mL of PRP were injected in the PRP group [8]. A ganglionic injection technique was employed in our cases [12]. The procedure was considered effective if the patient reported pain relief of >75% compared with preprocedural pain [13].
C-arm images showing lumbar transforaminal injection technique. (A) Scotty-dog view with 22G spinal needle targeting the foramen. (B) Anteroposterior view with radiculogram. (C) Lateral view showing position of spinal needle and radiculogram.
Data collected for analysis included age, sex, level affected, modified Oswestry Disability Index (mODI), Visual Analog Scale (VAS) score for leg pain, and Short-Form 12 (SF-12) score before the procedure and 1 week, 3 weeks, 6 weeks, 6 months, and 1 year after the procedure, and the mODI, VAS, and SF-12 scores were recorded only from patients who had not undergone any second injection or another procedure. The scores at 6 months and 1 year were not statistically analyzed between the groups because a reasonable number of patients received additional LTI or surgery. Any complications associated with the procedure immediately and until 1 year of follow-up were also documented.
Statistical analysis was done using the Mann-Whitney U test. A p-value of <0.05 was considered significant.
Results
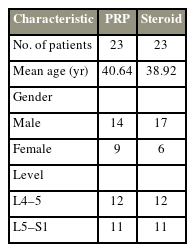
In this study, each group was composed of 23 patients. The demographic details are presented in Table 1. Both groups were comparable in terms of age, sex, and affected level. The PRP group was composed of 14 male and nine female patients with a mean age of 40.64 years, whereas the steroid group included 17 male and six female patients with a mean age of 38.92 years. The most common level affected were L4–L5 and L5–S1.
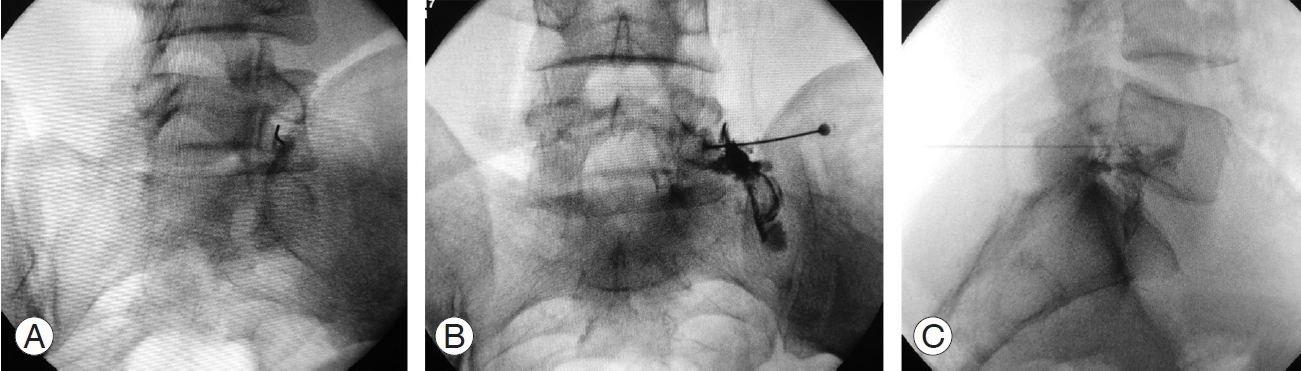
Three outcome measures were used in this study, namely, VAS for leg pain, mODI, and SF-12. The mean preprocedure mODI and SF-12 scale scores were comparable among the groups, with a p-value of >0.05 (0.52) (Fig. 3). At the 1-week follow-up, the steroid group showed better improvement in mean VAS, mODI, and SF-12 scale scores, and the results were statistically significant (p<0.0001) (Fig. 4). The PRP group showed better improvement in mean VAS, mODI, and SF-12 scale scores at the 3-week follow-up than at the 1-week follow-up, and the steroid group maintained improvement. The two groups showed no significant statistical difference in mean VAS, mODI, and SF-12 scale scores at the 3-week follow-up (Fig. 5).
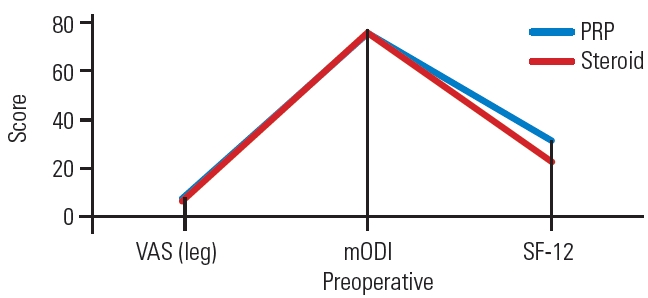
Pre-injection mean Visual Analog Scale (VAS), modified Oswestry Disability Index (mODI) and Short-Form 12 (SF-12) scores of steroids and plateletrich plasma (PRP) groups showing that both the groups were comparable.
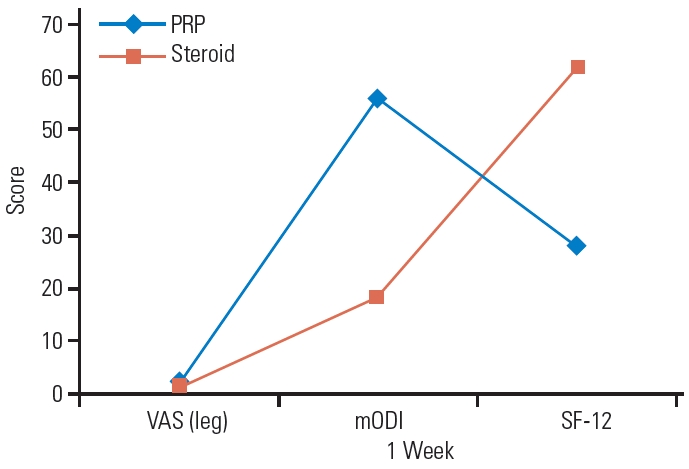
Visual Analog Scale (VAS), modified Oswestry Disability Index (mODI), and mean Short-Form 12 (SF-12) scores of steroids and platelet-rich plasma (PRP) groups at the 1-week follow-up.
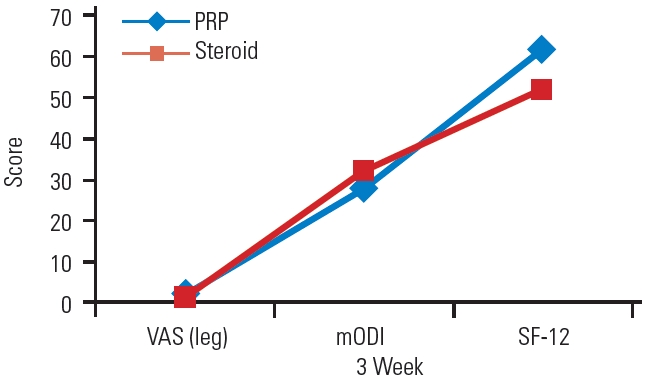
Visual Analog Scale (VAS), modified Oswestry Disability Index (mODI), and Short-Form 12 (SF-12) scores of platelet-rich plasma (PRP) and steroid groups at the 3-week follow-up.
At the 6-week follow-up, all mean scores of the three measures were better in the PRP group (Fig. 6), and the results were statistically significant (VAS, p<0.0001; ODI, p=0.02; SF-12, p=0.002).
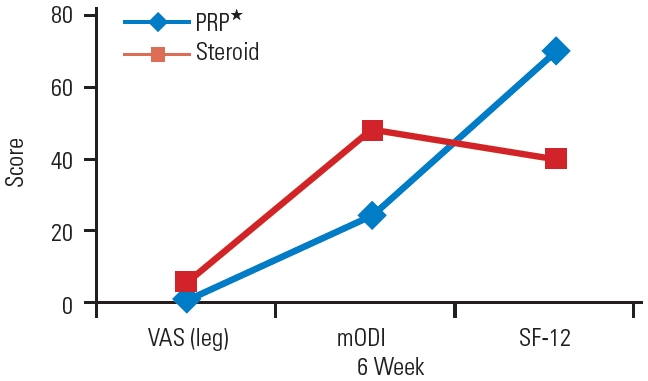
Mean Visual Analog Scale (VAS), modified Oswestry Disability Index (mODI), and Short-Form 12 (SF-12) scores of platelet-rich plasma (PRP) and steroid groups at the 6-week follow-up.
On comparing functional outcomes within the group at 1 week and 6 weeks, the steroid group showed a decline in functional improvement (Fig. 7). However, the PRP group did not show much improvement initially at 1 week but then had constant improvement over 6 weeks in all outcome scores (Fig. 8). At the 6-month follow-up, 39% of the patients in the steroid group continued to demonstrate improvement compared with 56% in the PRP group. At the 1-year follow-up, 26% of the patients in the steroid group and 30% in the PRP group demonstrated significant improvements in all three outcome measures when compared with their respective preprocedural values. The statistical comparison between the two groups for the 6-month and 1-year values was not performed because a substantial number of patients had undergone additional surgery. In the steroid group, nine patients received more LTIs, and eight patients underwent surgery at the 1-year follow-up. In the PRP group, seven patients received repeat LTIs, and nine underwent surgery. In the PRP group, seven patients received repeat injections of steroids; as this was a pilot study, no data are available about the safety of multiple PRP injections (although we assume it to be safe because of its autologous nature). No complications occurred in both groups at the 1-year follow-up.
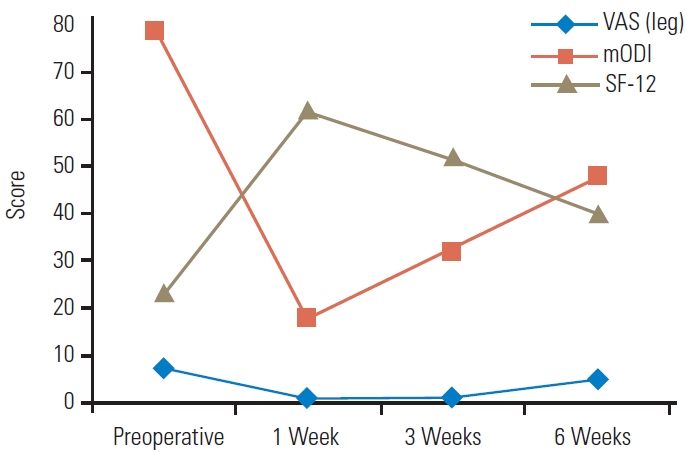
Progress of mean Visual Analog Scale (VAS), modified Oswestry Disability Index (mODI), and Short-Form 12 (SF-12) scores of steroid groups from 1 week to 6 weeks.
Discussion
Lumbar disc prolapse is a common cause of lower limb radicular pain. The cause of pain could be mechanical and/or inflammatory [14]. LTI has always been a preferred nonsurgical treatment option for clinicians in patients with radicular pain not responding to conservative treatment and it counters the inflammatory cause of pain [14]. However, clinicians are now employing various modifications of LTIs, and many studies are being conducted to determine the superiority of one procedure to another.
Vad et al. [4] in 2002 conducted a randomized controlled trial in which patients were randomly divided into two groups: one receiving steroids epidurally and the other saline at the trigger point. They found that after an average of 1.4 years of follow-up, a success rate of 84% was noticed in the steroid group compared with 48% in the saline group. They concluded that epidural steroids are one of the good options in the conservative treatment of radiculopathy.
In 1998, Fukusaki et al. [15] conducted a prospective study comparing the effect of epidural injection of steroids and local anesthetics with that of local anesthetics alone for radicular pain. They concluded that epidural steroids have no added advantage over local anesthetics.
The steroids have few limitations apart from routine procedure-related complications. Steroids should not be given for more than four injections in a year. More steroid injections can cause hypothalamic–pituitary–adrenal axis suppression and worsen osteoporosis [16]. Although many other drugs such as etanercept [6] and sodium hyaluronate/carboxymethyl cellulose solution [7] have promising results, none of them have become popular among spine surgeons.
PRP was also used for discogenic back pain and radicular pain [17]. PRP contains 150,000–300,000 platelets per microliter and 1,100 proteins including multiple growth factors. It also contains both inflammatory and anti-inflammatory cytokines including insulin-like growth factors 1 and 2, vascular endothelial growth factors, transforming growth factor-β, fibroblast growth factors, endothelial growth factors, and platelet-derived growth factors [18]. The current literature does not mention any definite preclinical evidence of its use in lumbar intervertebral disc prolapse. However, PRP has been advocated to promote tissue healing and regeneration. The increased levels of autologous growth factors and secretory proteins provided by concentrated platelets may enhance the healing process, particularly in degenerative tissues [19]. Anti-inflammatory cytokines, once activated, promote healing by altering the microenvironment and relieve pain [20]. Sufficient preclinical evidence shows that PRP induces extracellular matrix regeneration and cell proliferation. Formica et al. [21] and Nagae et al. [22] found less severe lesions in the nucleolus pulposus and annulus fibrosus histologically in the PRP group. MRI also confirmed the histological findings.
Autologous PRP has been widely used in patients with orthopedic conditions to help treat injuries to tendons, cartilage, ligaments, and muscles [18]. Bhatia and Chopra [17] conducted a pilot study using PRP administered via the interlaminar epidural route to treat pain in patients with prolapsed intervertebral discs and obtained favorable clinical outcomes. Akeda et al. [8] injected PRP into the discs of patients with chronic low back pain and degenerative disc disease in one or more lumbar segments. Improvement was seen in VAS scores, i.e., 7.1±1.2 to 1.8±2.0 (p<0.01), and it was sustained over 6 months. In an interesting case report, Lemper et al. [23] injected steroids in the lumbar spine of a patient with degenerative disc disease and radiculopathy. The patient became pregnant, and steroids were contraindicated considering her pregnancy. The patient was given PRP via interlaminar epidural injections for her pain, and she reported improvement in symptoms as early as 1 week after injection and was better at 3 months thereafter. She reported better pain relief with PRP than with steroids.
This double-blinded randomized controlled trial compared the outcomes of epidural steroids with those of PRP in single dermatomal lumbar radiculopathy caused by PIVD. The results of the follow-up of the PRP group were inferior to that in the steroid group after 1 week, comparable with the steroid group at 3 weeks, and better with the three outcome measures, i.e., VAS, mODI, and SF-12, at 6 weeks. Thus, we observed a peculiar trend in the improvement in the PRP group. Initially, there was not much improvement in pain, as seen at the 1-week follow-up; subsequently, improvement was increasing over time. The improvement even outwitted that in the steroid group. The possible explanation for such a trend is that PRP contains both inflammatory and anti-inflammatory mediators. The initial lesser effect was possibly caused by inflammatory mediators, followed by anti-inflammatory mediators at a later time. The effect seen in our participants was similar to that in the case reported by Lemper et al. [23]. PRP can be possibly given multiple times with no obvious complications because PRP is autologous in contrast to steroids that must not be given >4 times in a year. In addition, no risk of osteoporosis or any systemic side effects was documented as with steroids.
However, most of the studies mentioned short-term relief with one LTI. In the study by Arun-Kumar et al. [24], at the end of 6 months, only 20% of the patients had experienced pain relief. In the present study, 39% of the patients in the steroid group and 56% in the PRP group experienced significant pain relief at the 6-month follow-up. However, only 26% and 30% of the patients in the steroid and PRP groups, respectively, experienced pain relief at the end of 1 year. The patients having no pain relief in either group were managed with repeat LTIs with steroids or surgery. Repeat LTIs of steroids have been shown to improve outcomes. However, no studies have documented the outcomes and safety of repeat transforaminal PRP injections, although it can be considered safe considering its autologous nature.
To the best of our knowledge, only the study by Xu et al. [10] compared functional outcomes of steroids and PRP for lumbar radiculopathy. They compared PRP (n=61) and steroid (n=63) transforaminal injections using an ultrasound-guided technique. The follow-up duration was 1 year in both groups, and they did not find differences in outcomes between the two groups at 1 week, 1 month, 3 months, 6 months, and 1 year. By contrast, our study in which fluoroscopically guided LTIs were given showed better outcomes in the PRP group at 6 weeks. The results could not be compared at 6 months and 1 year because a significant number of patients underwent additional procedures because of pain recurrence.
This study has many limitations. First, this study included a small sample size and short follow-up. Second, since this was a pilot study, the outcomes of only one transforaminal PRP injection in the management of prolapse intervertebral disc were assessed. Such patients may require repeat injections and/or surgery if they do not respond to the treatment. Thus, many of the patients in the study had to be managed accordingly. Accordingly, it was not possible to study the long-term outcome after one transforaminal PRP injection and compare it with the group that received transforaminal steroid injections. Studies with longer a follow-up, larger number of participants, and repeat transforaminal injections are needed to establish the effects of PRP seen in our study. Third, particulate steroid (triamcinolone) was used in this study. Although concerns have been raised about the use of particulate steroids in epidural injections [25], some experts still prefer particulate steroids for lumbar transforaminal epidural injections because the pathophysiology of neurological deficits associated with spinal cord infarction remains unclear [26-28].
Conclusions
PRP is a useful alternative to steroids for LTIs in lumbar radiculopathy. Although improvement was delayed and 1-year outcomes were the same, 6-week and 6-month outcomes were better with PRP. Further multicenter studies with a larger number of participants, longer follow-up, and repeat LTIs are needed to draw a definite conclusion.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conception or design of the work: AG, HSC, VS, DN; acquisition, analysis, or interpretation of data: AG, HSC, VS, DN; creation of new software used in the work: AG, HSC, VS, DN; drafted the work or revised it critically for important intellectual content: AG, HSC, VS, DN; approved the version to be published: AG, HSC, VS, DN; and agree to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved: AG, HSC, VS, DN.