Outcomes of Balloon Kyphoplasty for Vertebral Compression Fractures in Patients with Diffuse Idiopathic Skeletal Hyperostosis at the Distal End or Adjacent Vertebra of the Fused Segments
Article information
Abstract
Study Design
A retrospective cohort study.
Purpose
To investigate the outcomes of balloon kyphoplasty (BKP) for vertebral compression fractures (VCFs) at the distal end or adjacent vertebra of the fused segments in patients with diffuse idiopathic skeletal hyperostosis (DISH).
Overview of Literature
Vertebral fractures in the midportion of the fused segments in patients with DISH are generally unstable; thus, immobilization is recommended. However, VCFs classified as type A in the AO classification are observed at the distal end and adjacent vertebra of the fused segments, and treatment strategies for VCFs associated with DISH remain controversial.
Methods
The outcomes of 72 patients who underwent BKP for VCFs between 2015 and 2021 were retrospectively investigated. Patients with DISH were assigned to group D (n=21), whereas those without DISH were assigned to group ND (n=51). Back pain, incidence of subsequent adjacent fractures, reoperation rates, and local kyphosis were statistically analyzed.
Results
VCFs in group D occurred at the distal end or adjacent vertebra of the fused segments, and no fractures occurred in the midportion of the fused segment. Back pain improved in both groups, with no significant differences between them. Subsequent adjacent fractures were observed in three of the 21 patients in group D and 11 of the 51 patients in group ND, with no significant difference between them. Reoperation was performed in one patient each in groups D and ND, with no significant difference between the groups. Postoperatively, local kyphosis progressed significantly in group D.
Conclusions
Although local kyphosis is more advanced in patients with DISH, BKP is effective for VCFs at the distal end or adjacent vertebra of the fused segments and may be useful in older patients with high complication rates.
Introduction
Diffuse idiopathic skeletal hyperostosis (DISH) is an ankylosing disorder of the spine characterized by the ossification of the anterior longitudinal ligament [1]. The prevalence of DISH in the general adult population varies greatly and ranges from 2.9% to 27.2%. This discrepancy could have been caused by variations in the study population characteristics, such as race, age, sex, prior history, and diagnostic techniques. Risk factors for DISH include being Caucasian, older, and male and having obesity, diabetes, hypertension, osteoarthritis, and so forth [2]. DISH-affected spines lose mobility and perform similarly to long bones. In patients with DISH, vertebral fractures in the midportion of the fused segments should be treated with posterior fixation because of the risk of pseudarthrosis and delayed paralysis [2,3]. However, DISH-associated fractures often occur not only in the midportion of the fused segments but also at the distal end or adjacent vertebra of the fused segments [2]. Although these fractures are thought to be more stable, such as vertebral compression fractures (VCFs), classified as type A in the AO classification, treatment strategies for VCFs at the distal end or adjacent vertebra of the fused segments remain controversial.
Balloon kyphoplasty (BKP) is a minimally invasive and widely used transpedicular cement augmentation procedure for the surgical management of typical VCFs [4]. Studies have reported that BKP for VCFs was associated with good results and low complication rates, with improved quality of life, function, mobility, and minimal pain [5,6]. However, to the best of our knowledge, no studies have reported on the efficacy and safety of BKP for VCFs in patients with DISH. Therefore, this study aimed to evaluate the outcomes of BKP for VCFs at the distal end or adjacent vertebra of the fused segments in patients with DISH. We hypothesized that VCFs in patients with DISH can be treated with BKP with good outcomes if the fracture occurs at the distal end or adjacent vertebra of the fused segments.
Materials and Methods
1. Participants and methods
This retrospective cohort study was approved by the Institutional Review Board of Fukuoka University Hospital (approval no., U21-11-019). Informed consent was obtained from all individual participants included in the study.
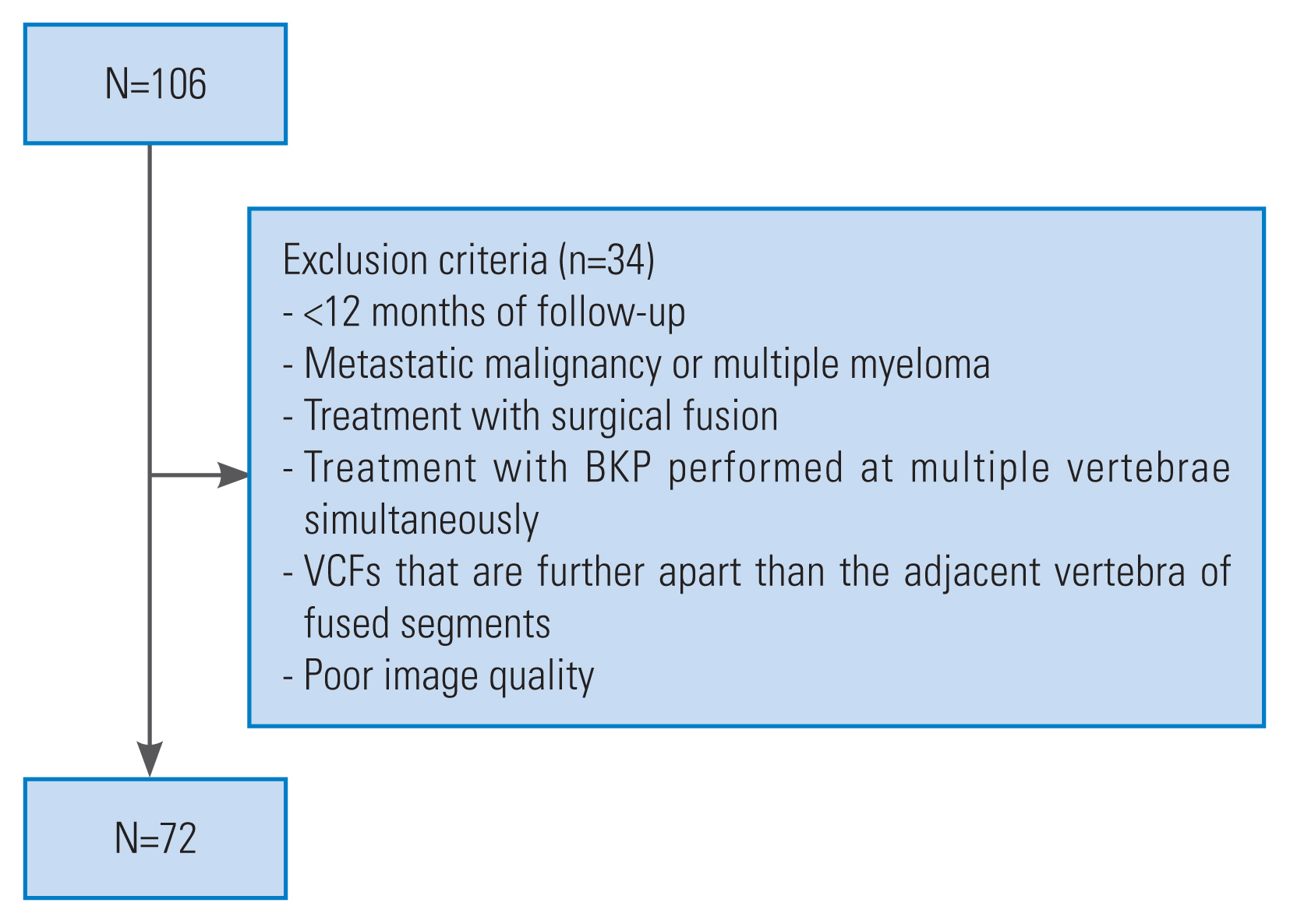
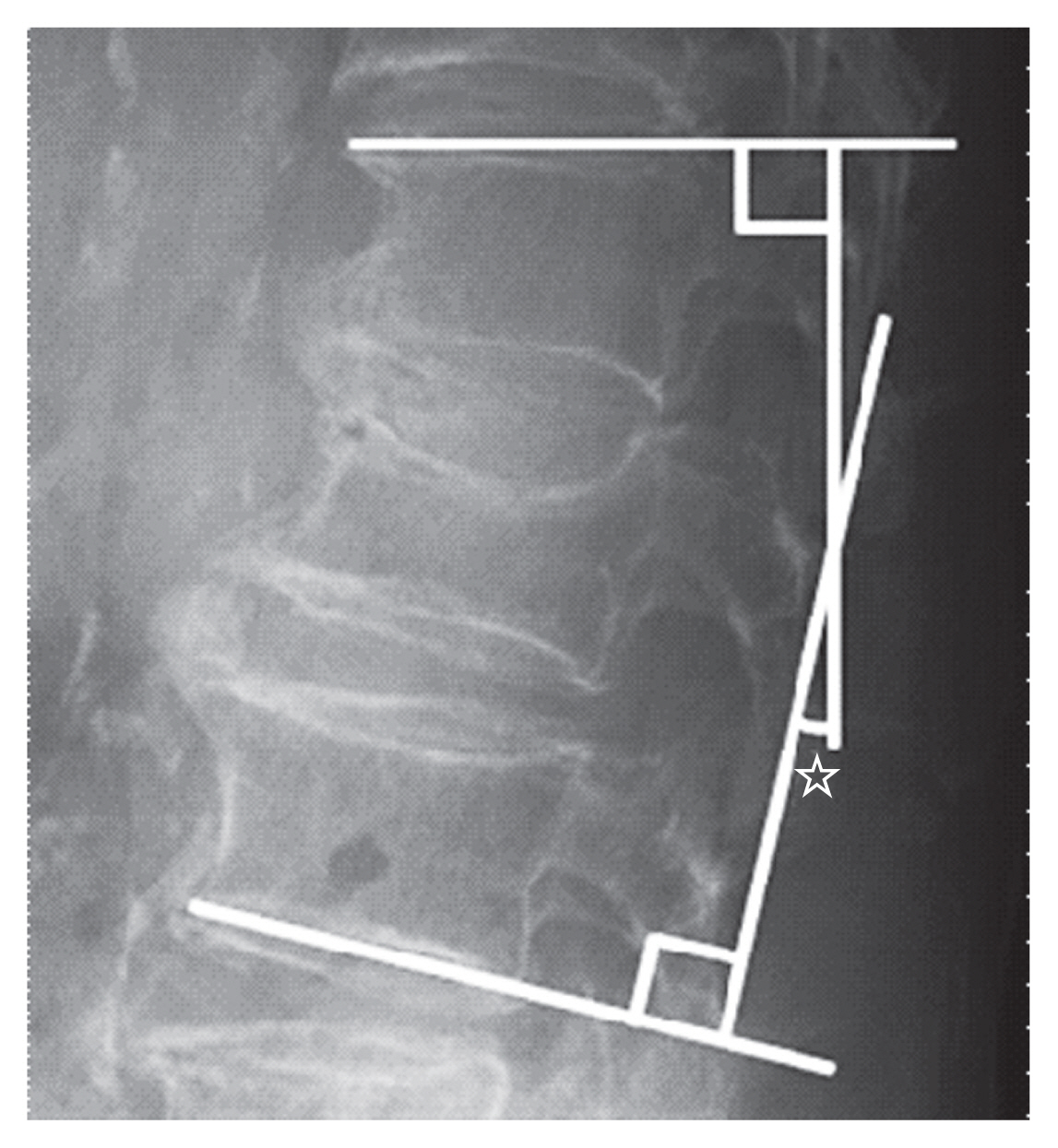
Surgical outcomes of 72 patients who underwent BKP for VCFs between 2015 and 2021 were assessed. All patients had a minimum follow-up of 12 months. BKP was indicated for VCFs in patients whose pain did not improve after conservative treatment. BKP was performed only for fractures with an AO classification of A; fractures with a classification of B or higher were treated with fixation. Radiography and magnetic resonance imaging were used to diagnose VCFs, and computed tomography was used to evaluate AO classification. According to the definition provided by Resnick et al. [1], DISH was defined as continuous anterior or lateral vertebral cross-linking and fusion of three or more intervertebral discs observed by radiography and computed tomography. Patients who had VCFs with DISH were assigned to group D, whereas those who had VCFs without DISH were assigned to group ND. The exclusion criteria were as follows: <12 months of follow-up, metastatic malignancy or multiple myeloma, treatment with surgical fusion, treatment with BKP performed simultaneously at multiple vertebrae, VCFs that are further apart than the adjacent vertebra of fused segments, and poor image quality (Fig. 1). All patients underwent surgery using the bilateral transpedicular approach. The patients were allowed to wear a rigid orthosis and began walking the day after surgery. Preoperative and postoperative images are shown in Fig. 2. Bone density measurements were taken preoperatively at the lumbar vertebra and proximal femur. Parathyroid hormone (PTH) was the primary recommendation for osteoporosis treatment; however, alternative treatments, such as denosumab or bisphosphonates, were considered for patients with side effects from PTH or who opted out of PTH. Each patient’s age, sex, follow-up period, time from injury to surgery, bone density at the lumbar vertebra, proximal femur, and fracture site were recorded. In group D, the positions of the fused vertebrae and fracture site (distal end or adjacent vertebra of the fused segments) were recorded. Back pain was investigated preoperatively, 3 months postoperatively, and at the final follow-up using a Numeric Rating Scale (NRS); subsequent adjacent fractures and reoperation at the final follow-up; and local kyphosis preoperatively, immediately postoperatively, and at the final follow-up. These factors were compared between groups D and ND. Subsequent adjacent fractures were confirmed by a 15% loss of height on radiography and bone signal intensity changes on magnetic resonance imaging. Local kyphosis was measured as the angle between the higher endplate of the upper vertebral body and the lower endplate of the lower vertebral body of the fractured vertebra (Fig. 3), including kyphosis of the adjacent fracture [7,8]. The progression of kyphosis from the immediate postoperative period to the final follow-up was also assessed.

Radiographic imaging findings in the lateral view. (A) Preoperative image, (B) image immediately after surgery, and (C) image at the last follow-up in group ND. (D) Preoperative image, (E) image immediately after surgery, and (F) image at the last follow-up in group D (distal end of the fused segments). (G) Preoperative image, (H) image immediately after surgery, and (I) image at the last follow-up in group D (adjacent vertebra of the fused segments). Group D: patients with diffuse idiopathic skeletal hyperostosis; Group ND: patients without diffuse idiopathic skeletal hyperostosis.
2. Statistical analysis
Continuous variables were analyzed using the Mann-Whitney U test, and categorical variables were analyzed using Fisher’s exact test. For all statistical tests, statistical significance was set at p<0.05. Statistical analyses were performed using IBM SPSS Statistics ver. 23.0 (IBM Corp., Armonk, NY, USA).
Results
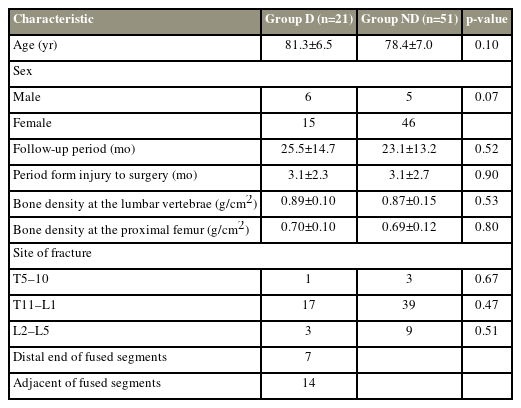
Groups D and ND included 21 and 51 patients, respectively. No significant differences were found in patient characteristics between the groups, although group D tended to be slightly older and comprised more male patients. Seven VCFs occurred at the distal end of the fused segments, and 14 occurred adjacent to the vertebra of the fused segments in group D (Table 1). No fractures occurred in the midportion of the fused segments in group D.
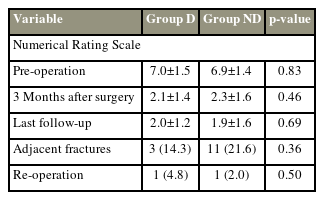
The mean preoperative NRS scores in groups D and ND were 7.0±1.5 and 6.9±1.4, respectively (p=0.83). The NRS scores 3 months postoperatively were 2.1±1.4 and 2.3±1.6 in groups D and ND, respectively (p=0.46). The NRS scores at the last follow-up were 2.0±1.2 in group D and 1.9±1.6 in group ND (p=0.69). No significant differences in the NRS scores were found between the groups at any timepoint. Subsequent adjacent fractures occurred in 3 (14.3%) of the 21 patients in group D and 11 (21.6%) of the 51 patients in group ND (p=0.36). Reoperation was performed in one patient (4.8%) in group D and one patient (2.0%) in group ND (p=0.50) (Table 2). In both groups, back pain scores were significantly better 3 months postoperatively and at the final follow-up than preoperatively (p<0.01) (Fig. 4). Reoperation was performed for anterior cement deviation in group D and back pain caused by progressive kyphosis in group ND.
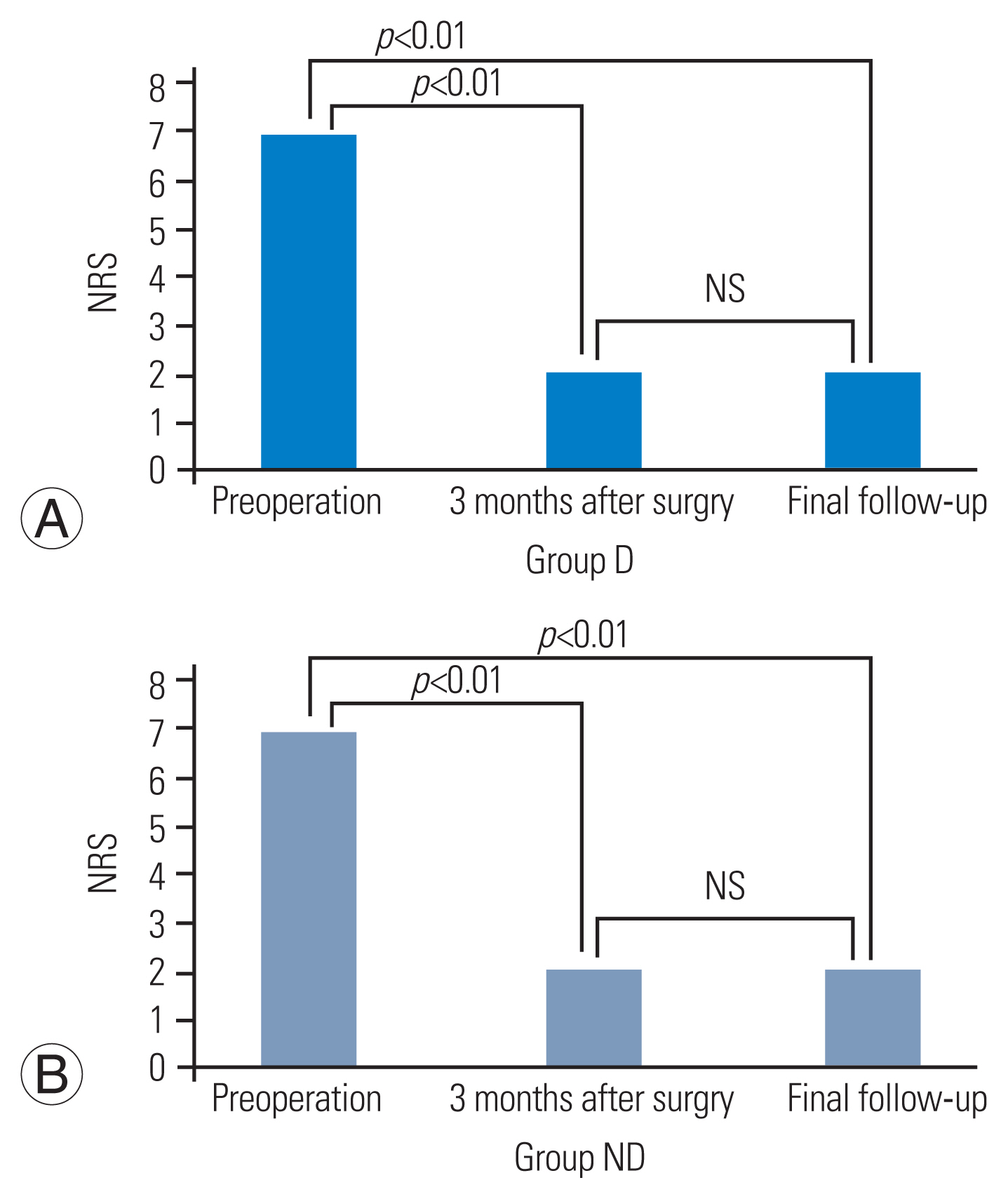
(A, B) Numeric Rating Scale (NRS) scores in groups D and ND showing that the scores improved significantly postoperatively in both the groups. Group D: patients with diffuse idiopathic skeletal hyperostosis; Group ND: patients without diffuse idiopathic skeletal hyperostosis. NS, not significance.
Local kyphosis was 19.0°±16.3° in group D and 21.9°±11.7° in group ND preoperatively (p=0.46), 12.1°±14.8° in group D and 18.2°±13.2° in group ND immediately after surgery (p=0.11), and 23.5°±16.4° in group D and 24.5°±12.9° in group ND at the final follow-up (p=0.81). The progression of kyphosis from the immediate postoperative period to the final follow-up was 11.5°±5.9° in group D and 6.3°±6.7° in group ND (p<0.01) (Table 3). The progression of kyphosis was significantly greater in group D than in group ND.
Discussion
Fractures at the midportion of the fused segments with DISH are prone to unstable fractures such as long bones during hyperextension [9]. Therefore, posterior fixation is often recommended [2,3]. However, many cases in this study sustained injury by falls from a standing position or lower, and when trauma is minor and compression forces are applied, VCFs are more likely to occur at the distal end or adjacent vertebra of the fused segments in DISH. BKP is widely recognized as the gold standard technique for pain relief in VCFs.
In this study, although the progression rate of local kyphosis was higher in group D than in group ND, no significant difference was found in back pain relief, risk of subsequent adjacent fractures, or risk of reoperation between the two groups. This finding suggests that BKP is a viable and effective option for treating VCFs at the distal end and adjacent vertebra of the fused segments in patients with DISH.
Subsequent adjacent fractures, a well-known complication of BKP, occur in 10%–52% of patients [10–12]. High cement volume and cement leakage into the disc are risk factors for subsequent adjacent fractures [12,13]; however, to the best of our knowledge, no studies have described the relationship between DISH and subsequent adjacent fractures. Initially, DISH might be a risk factor for subsequent adjacent fractures because of the increased load on the mobile segments secondary to the presence of fused vertebrae. However, no significant difference was found in the incidence of subsequent adjacent fractures between patients with and without DISH possibly because subsequent adjacent fractured were not related to spinal mobility but to the stress caused by cementation in BKP.
The patient in group D who underwent reoperation for anterior extrusion of bone cement had a large cleft in the vertebra and a deficit in the anterior wall. Cement resection and posterior fusion were subsequently performed. Studies have described the risks associated with cement extrusion. For example, Wang et al. [14] revealed that an anterior cortical defect in the vertebral body increases the risk of anterior displacement of the cement because of weight bearing. Ha et al. [15] reported that damage to the endplate might be a mechanism of the upward dislodgement of bone cement, and according to Takahashi et al. [16], a split-type fracture, angular motion of ≥14°, and large endplate deficits are risk factors for revision surgery after BKP. In patients with DISH, these risk factors increase the load at the fracture site and further increase the reoperation rate. In the patient in group D who underwent reoperation, the anterior cortices and endplates of the reoperated vertebrae were defective; therefore, the combination of posterior fixation with BKP should have been considered during the initial surgery.
In this study, the local kyphosis angle of group D increased significantly from the immediate postoperative period to the final follow-up period compared with that of group ND. Previous studies have noted an association between DISH and increased kyphosis in the sagittal global alignment [17–19]. Moreover, the actual effects are unknown because global alignment was not measured. In group D, DISH may have caused kyphosis of the global alignment, which in turn affected local kyphosis. Although no difference was noted in lumbar back pain between patients with and without DISH, kyphosis progression should be monitored in patients with DISH when BKP is performed.
Long fusion is associated with a high risk of perioperative complications such as implant failure, surgical site infections, pneumonia, urinary tract infections, hemorrhagic shock, and death [20–22]. Most patients with VCFs are older; therefore, their risks associated with posterior fusion may be higher than those in younger patients. Although DISH is a risk factor for local kyphosis, BKP for VCF is a valid option for older patients with high complication rates.
This study had several limitations. First, this was a retrospective study with a small sample. Second, kyphotic deformities in group D may only become clear during the long-term follow-up, and these issues must be monitored. Finally, we could not peform radiography of the entire spine, resulting in an evaluation of local kyphosis.
Conclusions
This study investigated the outcomes of BKP for VCFs at the distal end or adjacent vertebra of the fused segments in patients with DISH. Although local kyphosis progression was significantly greater in group D than in group ND, no significant differences in back pain, incidence of subsequent adjacent fractures, or reoperation rates were noted between the groups. BKP for VCFs in patients with DISH is effective at the distal end or adjacent vertebra of the fused segments. Thus, BKP is useful in older patients with high complication rates.
Acknowledgments
We would like to thank Editage (www.editage.jp) for English language editing.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Conception and design: Kyoichi Sanada, Jun Tanaka, Hideki Ohta, Yoshikuni Kida; data acquisition: Kyoichi Sanada, Yoshikuni Kida; analysis of data: Kyoichi Sanada; drafting of the manuscript: Kyoichi Sanada; critical revision: Jun Tanaka, Hideki Ohta, Yoshikuni Kida, Teruaki Shiokawa, Tatsuya Shibata, Shusuke Hagihara; supervision: Takuaki Yamamoto; and final approval of the manuscript: all authors.