|
 |
- Search
| Asian Spine J > Volume 11(4); 2017 > Article |
|
Abstract
Purpose
The purpose of this study was to evaluate the clinical and radiological results of the posterior-only approach with pedicle screws for the treatment of Scheuermann's kyphosis (SK).
Overview of Literature
The correction of SK with instrumentation can be performed using posterior-only or combined anterior-posterior procedures. With the use of all-pedicle screw constructs in spine surgery, the posterior-only approach has become a popular option for the definitive treatment of SK. In a nationwide study involving 2,796 patients, a trend toward posterior-only fusion with lower complication rates was reported.
Methods
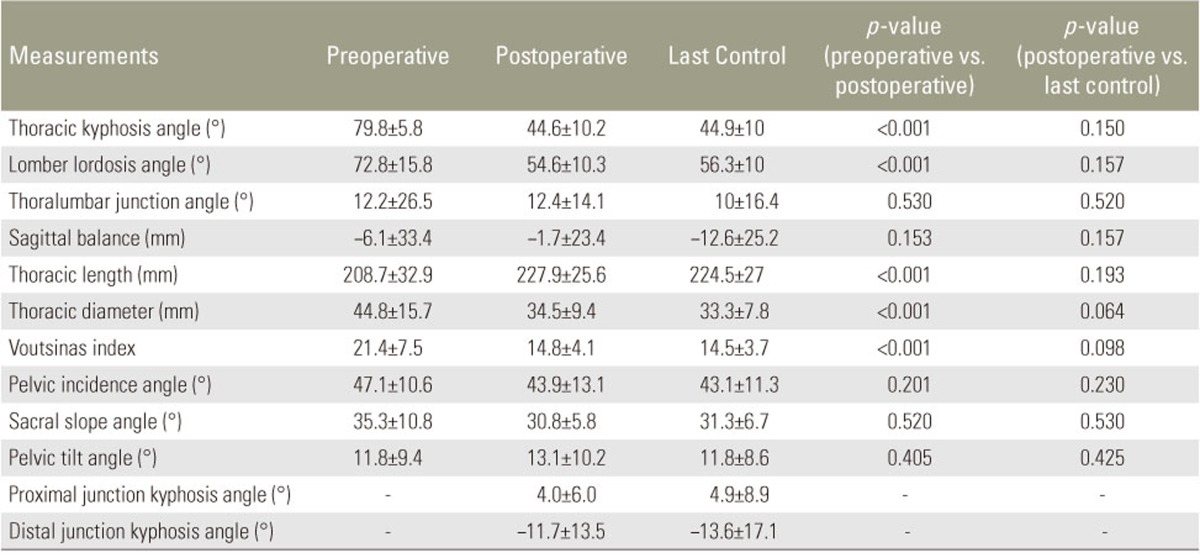
We retrospectively reviewed the data of patients who underwent posterior-only correction for SK between January 2005 and May 2013. Patients with a definite diagnosis of SK who fulfilled the minimum follow-up criterion of 24 months were included. The thoracic kyphosis (T5–T12), lumbar lordosis (L1–S1), and thoracolumbar junction (T10–L2) angles were measured from preoperative, postoperative, and last control radiographs. Sagittal balance, thoracic length, thoracic diameter, Voutsinas index and the sacral slope, pelvic tilt, proximal junction kyphosis, and distal junction kyphosis angles were also measured.
Results
Forty-five patients underwent surgery for the treatment of SK between 2005 and 2013. After applying the exclusion criteria, 20 patients (18 males and 2 females) with a mean age of 19 years were included. The mean thoracic kyphosis angle was 79.8 degrees preoperatively, 44.6 degrees postoperatively, and 44.9 degrees at the last control. There were statistically significant differences between preoperative and postoperative values in the thoracic kyphosis and lumbar lordosis angles, thoracic length, thoracic diameter, and Voutsinas index (p<0.05).
Scheuermann's kyphosis (SK) is a thoracic hyperkyphosis first described by Holger Werfel Scheuermann in 1921 [1]. Radiographically, this deformity presents as an anterior wedging of three consecutive vertebrae by more than 5 degrees, with endplate irregularities, loss of disc space, and the presence of Schmorl nodes [2].
According to the literature, operative treatment should be considered for patients with a kyphotic deformity of over 70–75 degrees, significant pain that has not responded to conservative management, and/or respiratory problems due to severe kyphosis [3]. The correction of kyphosis with instrumentation can be performed using posterior-only or combined anterior-posterior procedures [4]. With the use of all-pedicle screw constructs in spine surgery, the posterior-only approach has become a favorable option for the definitive treatment of SK [5]. In a nationwide study involving 2,796 patients, a trend toward posterior-only fusion with lower complication rates was reported [6].
The purpose of this study was to evaluate the clinical and radiological results of the posterior-only approach with pedicle screws in patients with SK.
Local ethical committee approval was obtained for this retrospective study. We retrospectively reviewed and analyzed the data of patients who underwent posterior-only correction for SK between January 2005 and May 2013. Patients with a definitive diagnosis of SK and a minimum follow-up of 24 months were included. Indications for surgery were a thoracic kyphosis angle of over 70 degrees with persistent pain despite conservative management and/or cosmetic concerns. Patients with tumors, inflammatory diseases, traumatic spine pathologies, and neurological deficits, as well as those who had spinal surgery, were excluded.
Standing anterior-posterior and lateral radiographs were taken preoperatively, shortly after surgery, and at the last control. Radiographs for all patients were evaluated by the same senior surgeon through our center's radiograph archiving system (PACS INFINITT, INFINITT Healthcare Co., Hangzhou, China). Thoracic kyphosis (T5–T12), lumbar lordosis (LL) (L1–S1), and thoracolumbar junction (T10–L2) angles were measured using the Cobb angle method preoperatively, postoperatively, and at the last control. Sagittal balance (displacement in mm, normally passing the C7 plumb line from the posterior-superior endplate of S1), thoracic length (length in mm, between the anterior-superior endplate of T1 and the anterior-inferior endplate of T12), thoracic diameter (length in mm, between the thoracic apex vertebrae and the thoracic length line), Voutsinas index (ratio of thoracic diameter to thoracic length×100, TD/TL×100), the sacral slope (SS) angle, and the pelvic tilt (PT) angle were also measured preoperatively, postoperatively, and at the last control.
Junctional kyphosis, which can occur in proximal or distal segments, is a common radiographic finding after SK surgery because of the abrupt transition between fixed and mobile spinal segments. The proximal junction kyphosis (PJK) angle (Cobb angle between the caudal endplate of the highest instrumented vertebrae and the cephalic endplate of the vertebrae two rows above) and distal junction kyphosis (DJK) angle (Cobb angle between the cephalic endplate of the lowest instrumented vertebrae and the caudal endplate of the vertebrae two rows below) were measured postoperatively and at the last control. Proximal or distal junctional kyphosis was considered to be present if the PJK or DJK angles were higher than 10 degrees. The Scoliosis Research Society 22 (SRS-22) questionnaire translated to our native language was completed by all patients.
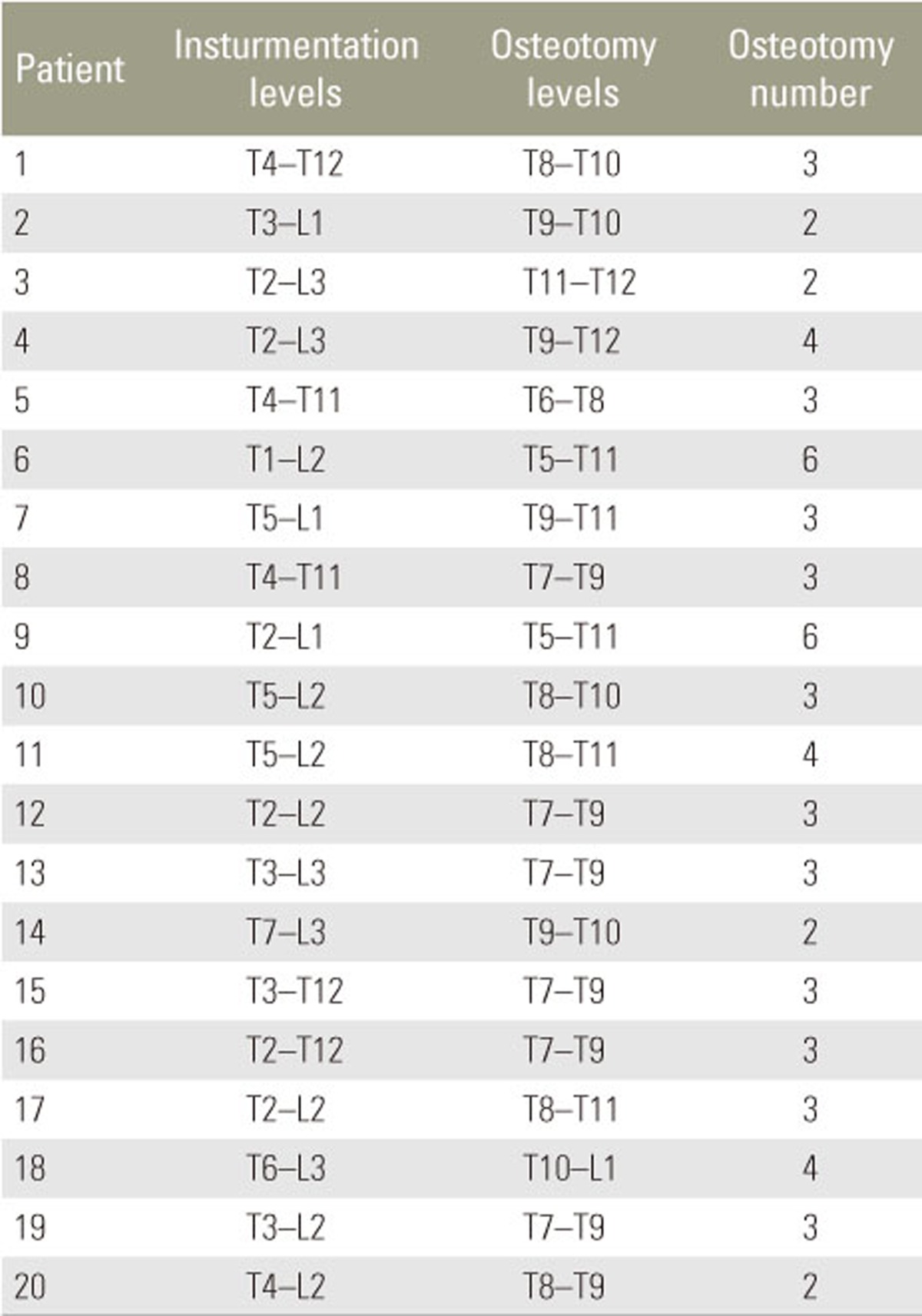
All surgeries were performed by two senior surgeons at our center's spine clinic using the same techniques. Patients were placed prone on the operating table (radiolucent table) under general anesthesia. A standard posterior midline incision was used, and paraspinal muscles were subperiosteally elevated to the tips of the transverse processes. Monoaxial titanium pedicle screws were bilaterally used for all levels and were placed using the free-hand technique. Proximal fusion was performed at the first kyphotic vertebrae to prevent PJK, and fusion was performed toward the first lordotic vertebrae distally. Apical Ponte osteotomies were routinely performed in all patients to enable deformity correction. Two 6.0 mm titanium rods were used for deformity correction after the above procedures, and the nuts were tightened. Allografts were used for nine patients, and posterior elements were decorticated and used as autologous grafts along the fusion levels for all patients.
On the first postoperative day, patients were ambulated under the guidance of an orthopedic surgeon. Patients were discharged with instructions to limit compelling activities and were contacted for follow-ups at the 2nd, 4th, 8th, 12th, and 24th weeks after surgery and annually afterwards.
SPSS ver. 17.0 for Windows (IBM, Chicago, IL, USA) was used for statistical analysis. Variance analysis (repeated analysis of variance) and post hoc Bonferroni analysis were performed to evaluate quantitative values such as preoperative, postoperative, and last control measurements. Categorical data were evaluated with Fisher's test, and p-values lower than 0.05 were considered statistically significant.
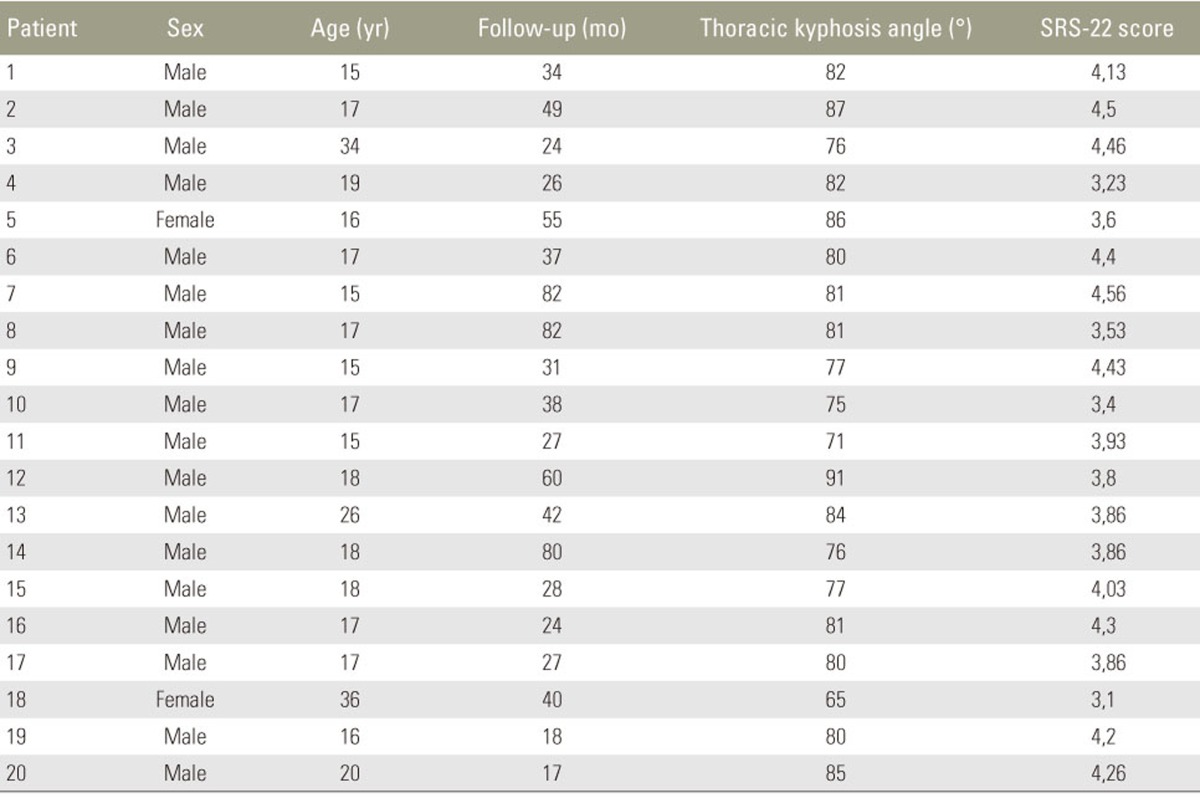
Forty-five patients underwent surgery for the treatment of SK between 2005 and 2013. After applying the exclusion criterion, 20 patients (18 males and 2 females) with a mean age of 19 years (range, 15 to 36 years) were included. Our follow-up rate was 44%, and the mean follow-up length was 41 months (range, 24 to 82 months). The demographic data of the patients are shown in Table 1, and the operative data are shown in Table 2. The mean preoperative thoracic kyphosis angle was 79.8±5.8 degrees (range, 65 to 91 degrees), and the mean postoperative thoracic kyphosis angle was 44.6±10.2 degrees (range, 20 to 58 degrees). The mean last control thoracic kyphosis angle was 44.9±10 degrees (range, 29 to 60 degrees) (Figs. 1, 2). The degree of correction was statistically significant when preoperative values were compared with early postoperative and last control values (p<0.05). There was no statistically significant difference between the early postoperative and last control values (p>0.05). Other values and the p values for preoperative, postoperative, and last control differences are shown in Table 3.
The mean SRS-22 score, which was evaluated from 1 to 5 points (1, worst; 5, best) for each component, was 3.9±0.4 points (range, 3.1 to 4.6 points) (Table 1). The best mean score was obtained from the “self-image” component and the worst was obtained from the “mental health” component. The most remarkable result from the questionnaire was that almost all patients answered “definitely yes” to the question “Would you have the same management again if you had the same condition?”
The following complications occurred: one patient had rod failure two years after surgery and revision surgery was performed, three patients had PJK (15%), and three patients had DJK (15%) (Fig. 3).
The posterior-only approach was the first operative technique introduced for the correction of kyphotic deformity in SK and was first performed by Bradford in 1975 [7]. Bradford et al. [8] reported loss of correction in 16 of 22 patients and emphasized that the correction of kyphosis at all lengths contributed to this complication. Different methods have been introduced over the years, and combined anterior-posterior fusion has been recommended for many years for rigid and large deformities. Today, debates continue regarding additional anterior release or posterior-only fusion for the surgical management of SK [4].
In this study, we achieved an average of 35 degrees of correction without loss of correction. Many studies have compared the posterior-only approach with anterior-posterior correction. In these studies, the authors reported similar results for the correction of deformity followed by loss of correction during the follow-up period, with higher complication rates reported for combined anterior-posterior groups [5910]. Consequently, the popularity of posterior-only fusion has increased in recent years. Papagelopoulos et al. [11] reported the results of posterior- only fusion using a segmental compression device in 13 patients. In the study, the thoracic kyphosis angle decreased from 68.5 to 40 degrees and the average loss of correction was 4.4 degrees after 4.5 years of follow-up. Ponte reported the results of posterior-only fusion (with Ponte osteotomies and pedicle screws) in 17 patients. In the study, the best results were achieved with the combined anterior-posterior technique [12]. Behrbalk et al. [13] also achieved satisfactory results in 21 patients in whom posterior-only fusion and Ponte osteotomies were performed. In the present study, we performed Ponte osteotomies for all patients and achieved satisfactory results for up to 91 degrees of thoracic kyphosis without additional anterior release.
In SK, thoracic hyperkyphosis is commonly associated with LL, which is reduced by the surgical correction of hyperkyphosis [14]. The preoperative and postoperative sagittal profiles and spinopelvic parameters of patients with SK have been compared in a few studies. Jansen et al. [15] reported a strong correlation between the correction of kyphosis and spontaneous decrease in the LL after fusion. Jansen also reported a correlation between LL and the SS. In the present study, we achieved a significant decrease in LL after the correction of thoracic kyphosis, and there were no significant changes in the SS, PT, and pelvic incidence (PI=SS+PT) after posterior fusion. In a recent study with 20 patients, sagittal spinopelvic parameters were evaluated after the posterior-only correction of SK and no significant changes were reported in the SS and PT, as well as in the PI as expected [16]. These results can be explained by the irreversible contracture of pelvic ligaments through the years because of kyphotic deformity.
The Voutsinas index is a measure that provides information about the morphology of kyphotic curves based on the Cobb method because the length and width of the curvature are taken into consideration [17]. In a study in which combined anterior-posterior fusion was performed in 15 patients, the authors achieved significant correction in the Voutsinas index, with no significant changes after 4 years of follow-up [18]. In our study, we also achieved significant correction and normalization in the Voutsinas index after posterior-only fusion, with no significant changes at the last control.
In a review, the overall complication rate after posterioronly fusion was reported to be 14.8% and did not significantly differ when compared with that after combined anterior-posterior fusion (16.9%) [19]. PJK and DJK are common well-known complications after SK surgery [20]. The most common risk factor for PJK is inadequate identification of the proximal end vertebrae, and overcorrection of kyphosis is another risk factor [2122]. In our study, 15% of the patients had asymptomatic PJK. The average correction of kyphosis for these patients was 33.4 degrees, and the cause of PJK was mostly likely the selection of the wrong proximal kyphotic vertebrae. Proper selection of the distal fusion level is important to prevent DJK after SK surgery [23]. Yanik et al. [24] reported their results for posterior-only fusion in 54 patients after investigating the occurrence of DJK in relation to the distal fusion level. They concluded that fusion to the first lordotic vertebrae is sufficient for distal fusion.
The main limitation of this study was the small patient population due to the low follow-up rate. The retrospective design of the study was another limitation. Prospective randomized studies with larger populations are needed in the future.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
2. Loder RT. The sagittal profile of the cervical and lumbosacral spine in Scheuermann thoracic kyphosis. J Spinal Disord 2001;14:226–231. PMID: 11389373.


3. Arlet V, Schlenzka D. Scheuermann’s kyphosis: surgical management. Eur Spine J 2005;14:817–827. PMID: 15830215.


4. Tsirikos AI, Jain AK. Scheuermann’s kyphosis; current controversies. J Bone Joint Surg Br 2011;93:857–864. PMID: 21705553.



5. Lee SS, Lenke LG, Kuklo TR, et al. Comparison of Scheuermann kyphosis correction by posterior-only thoracic pedicle screw fixation versus combined anterior/posterior fusion. Spine (Phila Pa 1976) 2006;31:2316–2321. PMID: 16985459.


6. Jain A, Sponseller PD, Kebaish KM, Mesfin A. National trends in spinal fusion surgery for Scheuermann kyphosis. Spine Deform 2015;3:52–56. PMID: 27927452.


7. Palazzo C, Sailhan F, Revel M. Scheuermann’s disease: an update. Joint Bone Spine 2014;81:209–214. PMID: 24468666.


8. Bradford DS, Moe JH, Montalvo FJ, Winter RB. Scheuermann’s kyphosis: results of surgical treatment by posterior spine arthrodesis in twenty-two patients. J Bone Joint Surg Am 1975;57:439–448. PMID: 1141252.


9. Lonner BS, Newton P, Betz R, et al. Operative management of Scheuermann’s kyphosis in 78 patients: radiographic outcomes, complications, and technique. Spine (Phila Pa 1976) 2007;32:2644–2652. PMID: 18007239.


10. Koptan WM, Elmiligui YH, Elsebaie HB. All pedicle screw instrumentation for Scheuermann’s kyphosis correction: is it worth it. Spine J 2009;9:296–302. PMID: 18640879.


11. Papagelopoulos PJ, Klassen RA, Peterson HA, Dekutoski MB. Surgical treatment of Scheuermann’s disease with segmental compression instrumentation. Clin Orthop Relat Res 2001;(386): 139–149.

12. Geck MJ, Macagno A, Ponte A, Shufflebarger HL. The Ponte procedure: posterior only treatment of Scheuermann’s kyphosis using segmental posterior shortening and pedicle screw instrumentation. J Spinal Disord Tech 2007;20:586–593. PMID: 18046172.


13. Behrbalk E, Uri O, Parks RM, Grevitt MP, Rickert M, Boszczyk BM. Posterior-only correction of Scheuermann kyphosis using pedicle screws: economical optimization through screw density reduction. Eur Spine J 2014;23:2203–2210. PMID: 25103951.


14. Jiang L, Qiu Y, Xu L, et al. Sagittal spinopelvic alignment in adolescents associated with Scheuermann’s kyphosis: a comparison with normal population. Eur Spine J 2014;23:1420–1426. PMID: 24639080.


15. Jansen RC, van Rhijn LW, van Ooij A. Predictable correction of the unfused lumbar lordosis after thoracic correction and fusion in Scheuermann kyphosis. Spine (Phila Pa 1976) 2006;31:1227–1231. PMID: 16688036.


16. Faldini C, Traina F, Perna F, Borghi R, Martikos K, Greggi T. Does surgery for Scheuermann kyphosis influence sagittal spinopelvic parameters? Eur Spine J 2015;24(Suppl 7): 893–897. PMID: 26441254.


17. Fotiadis E, Kenanidis E, Samoladas E, Christodoulou A, Akritopoulos P, Akritopoulou K. Scheuermann’s disease: focus on weight and height role. Eur Spine J 2008;17:673–678. PMID: 18301929.



18. Arun R, Mehdian SM, Freeman BJ, Sithole J, Divjina SC. Do anterior interbody cages have a potential value in comparison to autogenous rib graft in the surgical management of Scheuermann’s kyphosis? Spine J 2006;6:413–420. PMID: 16825049.


19. Coe JD, Smith JS, Berven S, et al. Complications of spinal fusion for scheuermann kyphosis: a report of the scoliosis research society morbidity and mortality committee. Spine (Phila Pa 1976) 2010;35:99–103. PMID: 20042960.


20. Denis F, Sun EC, Winter RB. Incidence and risk factors for proximal and distal junctional kyphosis following surgical treatment for Scheuermann kyphosis: minimum five-year follow-up. Spine (Phila Pa 1976) 2009;34:E729–E734. PMID: 19752692.


21. Koller H, Juliane Z, Umstaetter M, Meier O, Schmidt R, Hitzl W. Surgical treatment of Scheuermann’s kyphosis using a combined antero-posterior strategy and pedicle screw constructs: efficacy, radiographic and clinical outcomes in 111 cases. Eur Spine J 2014;23:180–191. PMID: 23893052.


22. Yanik HS, Ketenci IE, Polat A, et al. Prevention of proximal junctional kyphosis after posterior surgery of Scheuermann kyphosis: an operative technique. J Spinal Disord Tech 2015;28:E101–E105. PMID: 25075991.


23. Cho KJ, Lenke LG, Bridwell KH, Kamiya M, Sides B. Selection of the optimal distal fusion level in posterior instrumentation and fusion for thoracic hyperkyphosis: the sagittal stable vertebra concept. Spine (Phila Pa 1976) 2009;34:765–770. PMID: 19365243.


24. Yanik HS, Ketenci IE, Coskun T, Ulusoy A, Erdem S. Selection of distal fusion level in posterior instrumentation and fusion of Scheuermann kyphosis: is fusion to sagittal stable vertebra necessary? Eur Spine J 2016;25:583–589. PMID: 26195078.


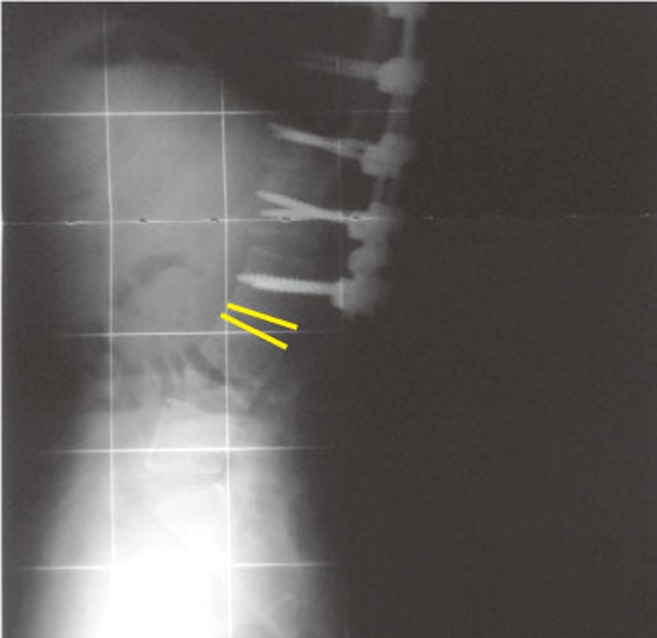
Fig. 1
A 17-year-old male with symptomatic and severe Scheuermann's kyphosis. T2–L2 levels were fused with the posterior-only approach, and Ponte osteotomies were performed. Preoperative (A), postoperative (B), and 29-month follow-up (C) standing anterior-posterior and lateral radiographs are presented.

Fig. 2
A 15-year-old male with symptomatic and severe Scheuermann's kyphosis. T5–L2 levels were fused with the posterior-onlyapproach, and Ponte osteotomies were performed. Preoperative (A), postoperative (B), and 82-month follow-up (C) standing anterior-posterior and lateral radiographs are presented.

- TOOLS
-
METRICS

- Related articles in ASJ
-
Mid-length Pedicle Screws in Posterior Instrumentation of Scoliosis2019 October;13(5)