|
 |
- Search
| Asian Spine J > Volume 12(1); 2018 > Article |
|
Abstract
Purpose
This study aimed to investigate the influence of distinct distal fusion levels on spinopelvic parameters in patients with adolescent idiopathic scoliosis (AIS) who underwent posterior instrumentation and fusion surgery.
Overview of Literature
The distal fusion level selection in treatment of AIS is the one of milestone to effect on surgical outcome. Most of the paper focused on the coronal deformity correction and balance. The literature have lack of knowledge about spinopelvic changing after surgical treatment and the relation with distal fusion level. We evaluate the spinopelvic and pelvic parameter alteration after fusion surgery in treatment of AIS.
Methods
A total of 100 patients with AIS (88 females and 12 males) were retrospectively reviewed. Patients were assigned into the following three groups according to the distal fusion level: lumbar 2 (L2), lumbar 3 (L3), and lumbar 4 (L4). Using a lateral plane radiograph of the whole spine, spinopelvic angular parameters such as thoracic kyphosis (TK), lumbar lordosis (LL), pelvic incidence (PI), sacral slope (SS), and pelvic tilt (PT) were radiologically assessed.
Results
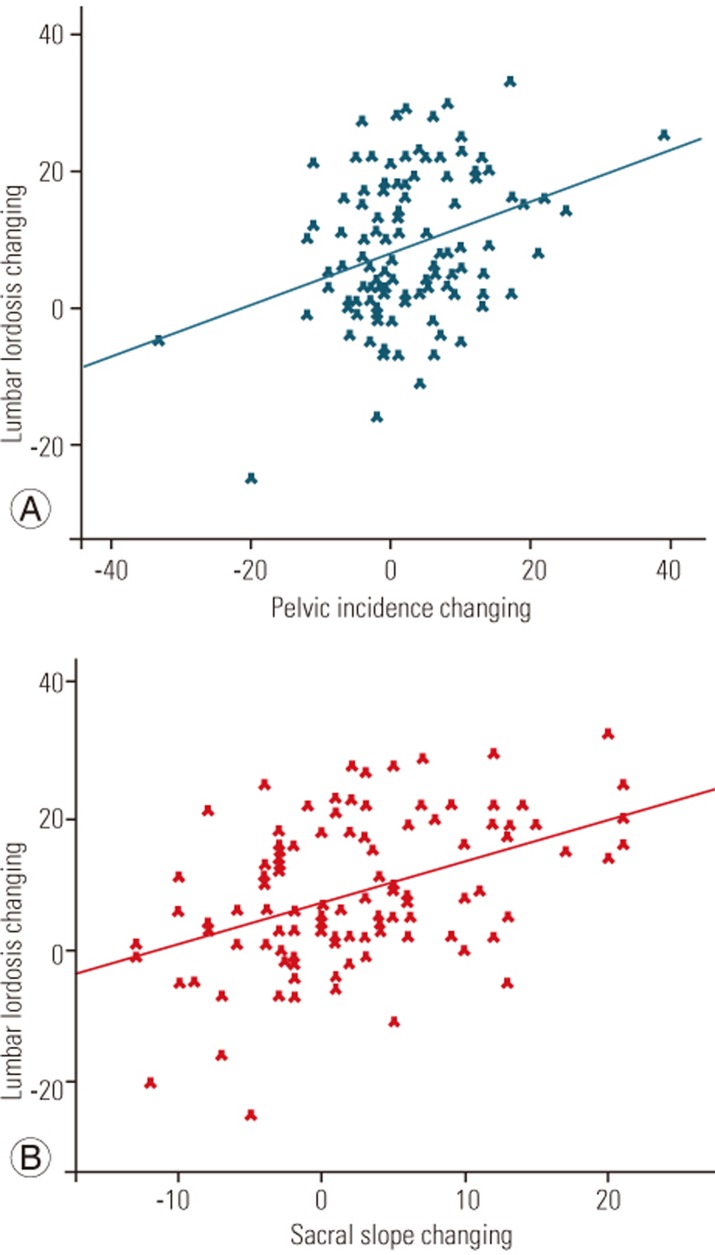
The mean age was 15±2.4 years, and the mean follow-up period was 24.27±11.69 months. Regarding the lowest instrumented vertebra, patients were categorized as follows: 30 patients in L2 (group 1), 40 patients in L3 (group 2), and 30 patients in L4 (group 3). TK decreased from 36.60±13.30 degrees preoperatively to 26.00±7.3 degrees postoperatively in each group (p=0.001). LL decreased from 52.8±9.4 degrees preoperatively to 44.30±7.50 degrees postoperatively (p=0.001). Although PI showed no difference preoperatively among the groups, it was statistically higher postoperatively in group 3 than in the other groups (p<0.05). In addition, in group 2, PI decreased from 50.60±8.74 degrees preoperatively to 48.00±6.84 degrees postoperatively (p=0.027). SS decreased from 35.20±6.40 degrees preoperatively to 33.40±5.80 degrees postoperatively (p=0.08, p>0.05). However, mean SS was significantly higher in group 3 (p=0.042, p<0.05). PT decreased from 15.50±7.90 degrees preoperatively to 15.2±7.10 degrees postoperatively. The positive relationship (28.5%) between LL and PI measurements was statistically significant (r=0.285; p=0.004, p<0.01). Furthermore, the positive relationship (36.5%) between LL and SS measurements was statistically significant (r=0.365; p=0.001, p<0.01).
With its S-shape, the sagittal spinal alignment is a distinctive feature of humankind and biomechanically assumes a key role in maintaining the upright human bipedalism with minimum energy expenditure, resulting in sagittal balance [1234567]. Sagittal radiographic parameters of the spine such as the angles of cervical lordosis, thoracic kyphosis (TK), and lumbar lordosis (LL) are used for assessing sagittal balance. Over the past several decades, numerous clinical studies have been devoted to examining these sagittal spinal parameters [891011]. However, in recent years, sagittal spinopelvic parameters have increasingly gained popularity for evaluating sagittal spinopelvic balance in children with adolescent idiopathic scoliosis (AIS) [212131415]. This has particularly been true since Duval-Beaupere et al. [16] discovered that besides examining the sagittal spinal alignment, analyzing the shape and orientation of the pelvis is a mandatory aspect for assessing.
Although sagittal spinal and spinopelvic parameters are distinct, each parameter has a high correlation with respect to the total balance of the spine. As a novel concept in the radiographical examination of patients with AIS, many researchers have recently shown an increased interest in using sagittal spinopelvic parameters such as pelvic incidence (PI), sacral slope (SS), and pelvic tilt (PT) [614171819]. However, little research has focused on the changes in spinopelvic parameters following posterior fusion surgery in the management of AIS [2021].
Although the distal fusion level plays a crucial role in reconstructing spinal deformity and trunk balance and maintaining motion segments, the effect of the lowest instrumented vertebra (LIV) on sagittal spinal and spinopelvic parameters remains to be examined in the literature. This study aimed to evaluate the effect of distinct distal fusion levels on spinopelvic parameters in patients with AIS who underwent posterior instrumentation and fusion surgery.
Between 2012 and 2014, 156 consecutive patients with a diagnosis of AIS underwent posterior instrumentation and fusion surgery that was performed by the same surgeons at the department of orthopaedics and traumatology, İstanbul Faculty of Medicine. The inclusion criteria were as follows: (1) diagnosis of AIS, (2) no history of previous spinal surgery, (3) no evidence of spondylolisthesis, and (4) a complete set of both preoperative and follow-up standing full-length anteroposterior and lateral radiographs of the spine, including the femoral head. The exclusion criteria were as follows: (1) selective thoracic fusion surgery, (2) upper level of the instrumented vertebra being lower than T3, (3) inadequate follow-up period, (4) presence of congenital deformities, and (5) anterior approach or osteotomy. Considering the above criteria, after excluding 56 patients, the remaining 100 patients who met the inclusion criteria (88 females and 12 males) were retrospectively reviewed using our institution's medical record database. The mean age of the patients was 15±2.4 years, and mean follow-up period was 24.27±11.69 months.
The distal fusion level was determined according to the stable vertebra theory, which is the first-touched vertebra by the central sacral vertical line (CSVL). The upper instrumented vertebra was the thoracal second or third vertebra. Segmental pedicle screws with a 6.0-mm titanium rod were used for all patients. All patients underwent a standard posterior surgery. After facetectomies within the fusion levels and the placement of pedicle screws, deformities were corrected via a simple rod derotation technique without direct vertebra derotation.
In terms of spinopelvic parameters, for all patients, a meticulous examination of standing full-length anteroposterior and lateral radiographs of the spine was performed by an orthopedic spine surgeon preoperatively and at the last postoperative follow-up. In the lateral view, six sagittal spinopelvic parameters, namely TK, LL, PI, SS, PT, and sagittal vertical axis (SVA), were measured. Similarly, in the anteroposterior view, two coronal spinal parameters, namely the coronal Cobb angle (CA) and CSVL, were analyzed. All radiographic parameters were measured at distinct times by two orthopedic spine surgeons. The measurements were performed both manually and digitally using the Surgimap software (Nemaris Inc., New York, NY, USA) by the author. At the final step of the study, the corresponding author (TA) provided a confirmation of the whole measurement values.
All radiographic measurements were performed using standardized techniques. LL and TK were measured using the CA technique; LL was the angle between the upper endplate of S1 and L1 and TK was the angle between the upper endplate of T1 and L1. Regarding the measurements of pelvic parameters, PI was obtained as the angle between the vertical line of the sacral plate and the line that connected the midpoint of the sacral plate to that of the bilateral femoral head center. PT was measured as the angle between the plumb line and the line that connected connecting the midpoint of the sacral plate to that of the bilateral femoral head center. SS was measured as the angle between the sacral plate and the horizontal line.
Statistical analyses were performed using the Number Cruncher Statistical System 2007 (NCSS Statistical Software, Kaysville, UT, USA) package. One-way analysis of variance was used to compare three or more normally distributed groups, and Tukey's honestly significant difference test was used to identify the group that caused the difference. Kruskal-Wallis test was used to compare three or more groups with non-normal distributions. Mann-Whitney U-test was used to identify the group that caused the difference. To interpret the comparisons of normally distributed variables within the groups, paired-sample test was performed. In addition, Wilcoxon signed rank test was used to compare variables that are not normally distributed within the groups. Finally, correlations were made using Spearman's correlation test, and p-values of <0.05 was considered to be statistically significant.
According to the Lenke classification, patients were divided into three groups: 34 patients with main thoracic curve (Lenke types I and II) were included in group 1, 32 patients consistent with Lenke type III in group 2, and 34 patients with main lumbar curve (Lenke types IV and V) in group 3. In addition, all patients were categorized according to the King-Moe classification: 34 patients were evaluated as type I, 27 as type II, 23 as type III, and 16 as type IV.
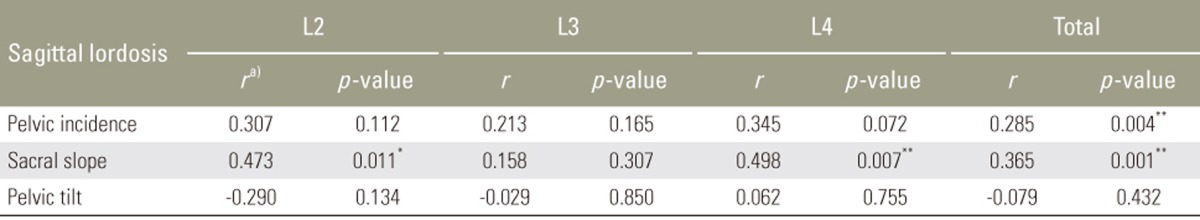
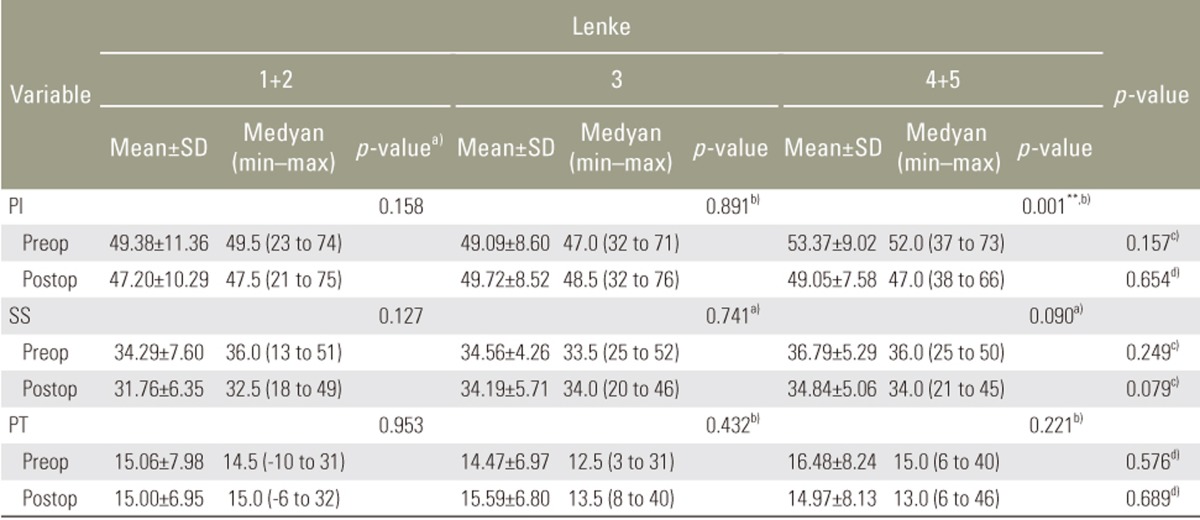
In terms of the distal fusion level, patients were categorized as follows: LIV was L2 in 30 patients (group 1, Fig. 1), L3 in 40 patients (group 2, Fig. 2), and L4 in 30 patients (group 3, Fig. 3).
TK decreased from 36.60±13.30 degrees preoperatively to 26.00±7.30 degrees postoperatively in each group, with no difference among all the groups (p=0.001, p=0.098). Similar to TK, LL demonstrated a decrease from 52.80±9.40 degrees preoperatively to 44.30±7.50 degrees postoperatively in each group, with no difference among all the groups (p=0.001, p=0.164).
Although PI showed no difference preoperatively among all the groups, it was significantly higher postoperatively in group 3 than in the other groups (p=0.006, p=0.014, p<0.05). Furthermore, PI decreased from 50.60±8.74 degrees to 48.00±6.84 degrees (p=0.027) in group 2. Although SS decreased from 35.16±6.40 degrees to 33.50±5.80 degrees, no difference was observed because of the surgery in group 3 (p=0.087, p>0.05). In group 3, mean SS decreased from 37.25±6.00 degrees preoperatively to 34.42±6.42 degrees postoperatively (p=0.050). Similarly, mean SS was significantly higher in group 3 postoperatively than group 1 (p=0.042, p<0.05). Mean PT decreased from 15.50±7.80 degrees preoperatively to 15.20±7.15 degrees postoperatively. Although there was no difference among all the groups, PT was significantly higher in group 3 than in the other groups (p=0.86, p>0.05, p=0.03) (Table 1).
For all cases, the positive relationship between LL and PI measurements was statistically significant (PI increased with LL) (r=0.285; p=0.004, p<0.01). Furthermore, the positive relationship between LL and SS measurements was statistically significant (SS increased with LL) (r=0.365; p=0.001, p<0.01) (Fig. 4, Table 2).
CSVL was 11.89±43.00 mm preoperatively and 11.40±34.00 mm postoperatively (p=0.727). CSVL did not change depending on the distal level. CA of deformity changed from 47.80±13.10 degrees preoperatively to 2.40±3.40 degrees postoperatively (p<0.05). However, SVA changed from 42.90±25.00 mm preoperatively to 30.80±12.80 mm postoperatively.
In the assessment of the variables according to Lenke groups, LL and TK significantly decreased, with no difference between the two parameters (p>0.05) among all the groups. Although there was no difference in PI among the Lenke groups, there was a statistically significant decrease in PI in group 3 (Lenke types IV and V; p>0.05, p=0.001). None of the Lenke groups showed a significant difference in terms of variance in TT measurements (p>0.05) (Table 3).
To date, the significance of restoring the spinopelvic balance following the surgical management of adult deformity has been well documented in the literature [122223]. Schwab et al. [24] proposed certain threshold angles that were relevant to spinopelvic parameters, which are essential for obtaining better functional outcomes through spinal reconstructive procedures. Moreover, Diebo et al. [22] drew attention to certain compensatory mechanisms that maintain global sagittal spinal alignment in the presence of spinopelvic mismatch. Although a great number of clinical studies that examine compensatory mechanisms following posterior instrumentation in adult scoliosis are available in the literature, little research has been devoted to examining this association in patients with AIS. To address the lack of current literature, we aimed to evaluate the effects of LIV on sagittal spinopelvic parameters in patients with AIS.
In the literature, the debate regarding the deviations in pelvic parameters in patients with AIS who underwent posterior instrumentation surgery compared with those in healthy individuals continues. Although some studies have reported no difference between the two populations [1925], others [618] revealed that PI was higher in patients with AIS than in normal individuals. However, there are explicit data in the literature regarding the variance relevant to some spinopelvic parameters in patients with AIS following surgical management [2021]. For instance, La Maida et al. [20] reported a statistically significant increase in PT. Similarly, on analyzing 60 patients with AIS following posterior spinal instrumentation and fusion surgery, Tanguay et al. [21] found a significant association between LL and pelvic parameters below and within the fusion. In the present study, in contrast to the literature, postoperative PT was not statistically significantly different from preoperative PT. However, LL was showed a statistically significant decrease, and the association between LL and pelvic parameters, according to earlier literature that found correlations among the three variables LL, SS, and PI, was positive and statistically significant (r=0.285; p=0.004, p<0.01; r=0.367; p=0.001, p<0.01).
When the distal fusion level and variance in pelvic parameters were compared, a significant decrease in PI was observed in cases with distal level at L3. distal level, whereas the highest PI values were observed in cases with L4 distal level. When the distal fusion level was determined to be L3, the changes in LL were compensated by mobile segments, and this process concluded the compensatory decrease in the PI values. However, when the distal fusion level was determined to be L4, the PI values demonstrated no statistically significant difference. As a secondary consequence, the changes in LL were compensated only by pelvic parameters. Moreover, if the distal fusion level was determined to be L4, SS decreased but PT increased; however, this was not statistically significantly different.
At the same time, the association between the change in LL and SS was more significant in cases where distal fusion levels were L2 and L4. Although changes in LL were not statistically significantly different, L3 displayed pelvic parameter changes that were independent of the changes in LL. These data show that identifying the distal fusion level as L3 plays a key role in influencing the change in pelvic parameters.
Upasani et al. [9] compared thoracic and lumbar AIS, and although there were differences between TK and LL, there was no statistically significant difference among pelvic parameters. In the current study, in terms of spinopelvic parameters, with the exception of the difference between LL and SS, none of the other parameters showed a statistically significant difference among all the groups. However, to date, little research has focused on the variance in spinopelvic parameters in AIS following surgery. La Maida et al. [20] conducted an investigation of Lenke type I patients and observed that surgical treatment decreased SS but increased PT. This phenomenon was explained as a compensatory retroversion that maintained sagittal balance [20]. However, Tanguay et al. [26] found no statistically significant difference in PT angles preoperatively or postoperatively among the Lenke groups. In groups with a major lumbar curve, surgery generates a significant decrease in PI. In contradiction to previously reported literature, PI showed a statistically significant decrease in the major lumbar curve group (Lenke types IV and V). Nevertheless, reported data that provide an explanation regarding this phenomenon are limited. We inferred that in adolescent patients, PI is not as stable a parameter as it is in adults. This can be defined that the changing at spinopelvic parameter alters with surgery through the adolescent period. The change in LL is the key aspect for explaining the difference in pelvic parameters following fusion surgery because LL is negatively influenced by fusion surgery. Accordingly, in this study, some compensatory mechanisms arose in the unfused segment and PI. Consequently, the surgery resulted in a statistically significant decrease in PI, particularly in the major lumbar curve group of AIS.
Finally, this study has some significant limitations. First, this was a retrospective cohort study that lacked a refined series. Second, we were unable to standardize the position of the radiographic images while performing the evaluations. Thus, a larger series with similar distribution is required to evaluate the variance in pelvic parameters following posterior instrumentation and fusion surgery.
LL may be a key factor for restoring pelvic parameters following posterior fusion surgery. Furthermore, this study showed that the selection of LIV (i.e., lower than the L3 level) may result in decompensation in the pelvic parameters. Consequently, spine surgeons should be stop fusion level proximaly L3 in order not to altering spinopelvic parameters.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
1. Poncet P, Dansereau J, Labelle H. Geometric torsion in idiopathic scoliosis: three-dimensional analysis and proposal for a new classification. Spine (Phila Pa 1976) 2001 26:2235–2243. PMID: 11598514.


2. Roussouly P, Labelle H, Rouissi J, Bodin A. Pre- and post-operative sagittal balance in idiopathic scoliosis: a comparison over the ages of two cohorts of 132 adolescents and 52 adults. Eur Spine J 2013 22(Suppl 2): S203–S215. PMID: 23188161.


3. Lehman RA Jr, Lenke LG, Keeler KA, et al. Operative treatment of adolescent idiopathic scoliosis with posterior pedicle screw-only constructs: minimum three-year follow-up of one hundred fourteen cases. Spine (Phila Pa 1976) 2008 33:1598–1604. PMID: 18552676.


4. Stokes IA. Three-dimensional terminology of spinal deformity: a report presented to the Scoliosis Research Society by the Scoliosis Research Society Working Group on 3-D terminology of spinal deformity. Spine (Phila Pa 1976) 1994 19:236–248. PMID: 8153835.


5. Janssen MM, Vincken KL, van Raak SM, et al. Sagittal spinal profile and spinopelvic balance in parents of scoliotic children. Spine J 2013 13:1789–1800. PMID: 23819971.


6. Mac-Thiong JM, Labelle H, Charlebois M, Huot MP, de Guise JA. Sagittal plane analysis of the spine and pelvis in adolescent idiopathic scoliosis according to the coronal curve type. Spine (Phila Pa 1976) 2003 28:1404–1409. PMID: 12838098.


7. Berthonnaud E, Dimnet J, Roussouly P, Labelle H. Analysis of the sagittal balance of the spine and pelvis using shape and orientation parameters. J Spinal Disord Tech 2005 18:40–47. PMID: 15687851.


8. Potter BK, Kuklo TR, Lenke LG. Radiographic outcomes of anterior spinal fusion versus posterior spinal fusion with thoracic pedicle screws for treatment of Lenke type I adolescent idiopathic scoliosis curves. Spine (Phila Pa 1976) 2005 30:1859–1866. PMID: 16103856.


9. Upasani VV, Tis J, Bastrom T, Pawelek J, et al. Analysis of sagittal alignment in thoracic and thoracolumbar curves in adolescent idiopathic scoliosis: how do these two curve types differ? Spine (Phila Pa 1976) 2007 32:1355–1359. PMID: 17515826.


10. Cil A, Yazici M, Uzumcugil A, et al. The evolution of sagittal segmental alignment of the spine during childhood. Spine (Phila Pa 1976) 2005 30:93–100. PMID: 15626988.


11. Diebo BG, Varghese JJ, Lafage R, Schwab FJ, Lafage V. Sagittal alignment of the spine: what do you need to know? Clin Neurol Neurosurg 2015 139:295–301. PMID: 26562194.


12. Schwab FJ, Blondel B, Bess S, et al. Radiographical spinopelvic parameters and disability in the setting of adult spinal deformity: a prospective multicenter analysis. Spine (Phila Pa 1976) 2013 38:E803–E812. PMID: 23722572.


13. Li W, Sun Z, Guo Z, et al. Analysis of spinopelvic sagittal alignment in patients with thoracic and thoracolumbar angular kyphosis. Spine (Phila Pa 1976) 2013 38:E813–E818. PMID: 23524868.


14. Lonner BS, Auerbach JD, Sponseller P, Rajadhyaksha AD, Newton PO. Variations in pelvic and other sagittal spinal parameters as a function of race in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2010 35:E374–E377. PMID: 20139806.


15. Pasha S, Aubin CE, Sangole AP, Labelle H, Parent S, Mac-Thiong JM. Three-dimensional spinopelvic relative alignment in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2014 39:564–570. PMID: 24384650.


16. Duval-Beaupere G, Schmidt C, Cosson P. A Barycentremetric study of the sagittal shape of spine and pelvis: the conditions required for an economic standing position. Ann Biomed Eng 1992 20:451–462. PMID: 1510296.


17. Legaye J, Duval-Beaupere G. Sagittal plane alignment of the spine and gravity: a radiological and clinical evaluation. Acta Orthop Belg 2005 71:213–220. PMID: 16152857.

18. Mac-Thiong JM, Labelle H, Berthonnaud E, Betz RR, Roussouly P. Sagittal spinopelvic balance in normal children and adolescents. Eur Spine J 2007 16:227–234. PMID: 16311754.


19. Yong Q, Zhen L, Zezhang Z, et al. Comparison of sagittal spinopelvic alignment in Chinese adolescents with and without idiopathic thoracic scoliosis. Spine (Phila Pa 1976) 2012 37:E714–E720. PMID: 22166928.


20. La Maida GA, Zottarelli L, Mineo GV, Misaggi B. Sagittal balance in adolescent idiopathic scoliosis: radiographic study of spino-pelvic compensation after surgery. Eur Spine J 2013 22(Suppl 6): S859–S867. PMID: 24061971.


21. Tanguay F, Mac-Thiong JM, de Guise JA, Labelle H. Relation between the sagittal pelvic and lumbar spine geometries following surgical correction of adolescent idiopathic scoliosis. Eur Spine J 2007 16:531–536. PMID: 17051398.


22. Diebo BG, Ferrero E, Lafage R, et al. Recruitment of compensatory mechanisms in sagittal spinal malalignment is age and regional deformity dependent: a full-standing axis analysis of key radiographical parameters. Spine (Phila Pa 1976) 2015 40:642–649. PMID: 25705962.


23. Barrey C, Roussouly P, Perrin G, Le Huec JC. Sagittal balance disorders in severe degenerative spine: can we identify the compensatory mechanisms? Eur Spine J 2011 20(Suppl 5): 626–633. PMID: 21796393.



24. Schwab F, Patel A, Ungar B, Farcy JP, Lafage V. Adult spinal deformity-postoperative standing imbalance: how much can you tolerate?: an overview of key parameters in assessing alignment and planning corrective surgery. Spine (Phila Pa 1976) 2010 35:2224–2231. PMID: 21102297.


25. Schlosser TP, Shah SA, Reichard SJ, Rogers K, Vincken KL, Castelein RM. Differences in early sagittal plane alignment between thoracic and lumbar adolescent idiopathic scoliosis. Spine J 2014 14:282–290. PMID: 24231781.


26. Tanguay F, Mac-Thiong JM, de Guise JA, Labelle H. Relation between the sagittal pelvic and lumbar spine geometries following surgical correction of adolescent idiopathic scoliosis: a preliminary study. Stud Health Technol Inform 2006 123:299–302. PMID: 17108442.


Fig. 1
(A) Preoperative AP spine X-ray (group 1). (B) Preoperative lateral spine X-ray with measurement (group 1). (C) Postoperative AP spine X-ray (group 1). (D) Postoperative lateral spine X-ray with measurement (group 1). AP, anteroposterior.
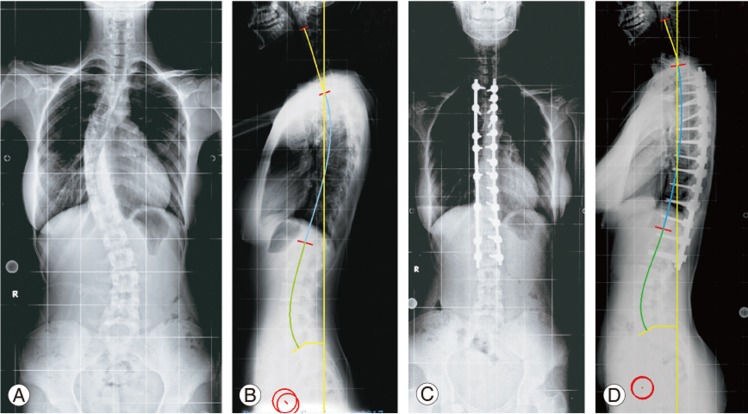
Fig. 2
(A) Preoperative AP spine X-ray (group 2). (B) Preoperative lateral spine X-ray with measurement (group 2). (C) Postoperative AP spine X-ray (group 2). (D) Postoperative lateral spine X-ray with measurement (group 2). AP, anteroposterior.
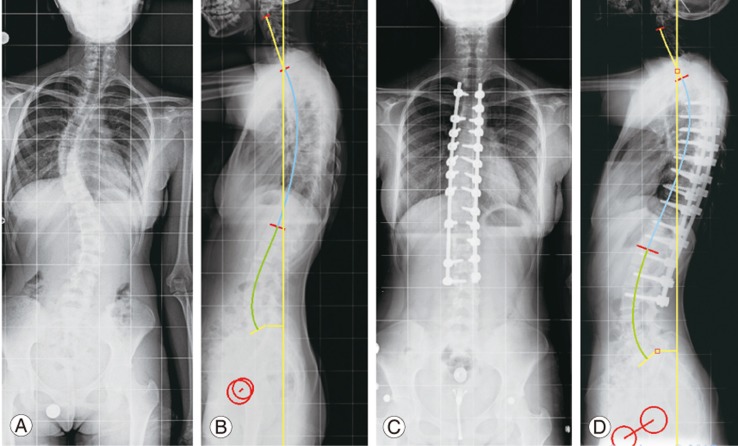
Fig. 3
(A) Preoperative AP spine X-ray (group 3). (B) Preoperative lateral spine X-ray with measurement (group 3). (C) Postoperative AP spine X-ray (group 3). (D) Postoperative lateral spine X-ray with measurement (group 3). AP, anteroposterior.
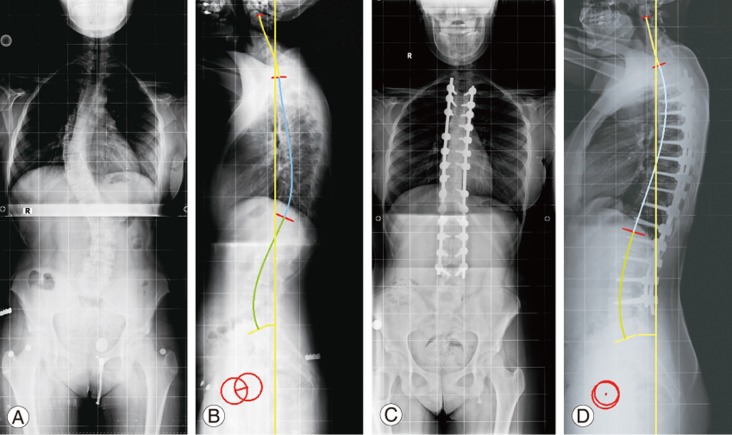
Fig. 4
(A) Correlation between lumbar lordosis and pelvic incidence (group 4). (B) Correlation between lumbar lordosis and sacral slope (group 4).
- TOOLS
-
METRICS

- Related articles in ASJ
-
The Role of Vitamin D in the Pathogenesis of Adolescent Idiopathic Scoliosis2018 December;12(6)