|
 |
- Search
| Asian Spine J > Volume 3(1); 2009 > Article |
Abstract
Purpose
To assess the radiological, clinical features and surgical outcomes of six patients of elementary school age with lumbar disc herniation (LDH).
Overview of Literature
LDH is common in people in their fourth and fifth decades. However, the condition is extremely rare in children of elementary school age. Moreover, the clinical symptoms and treatments are different from those of adults.
Methods
We reviewed a series of 6 patients under the age of 12 years, who underwent surgery for LDH at our institution between 1992-2002. Initially, all patients were treated conservatively. The indications for surgery were failure of conservative treatment for 3 months, intractable pain and/or progressive neurological impairment.
Results
The surgical findings revealed a protruding disc in five cases and a ruptured disc in one. In addition, separation of the vertebral ring apophysis was observed in 3 cases. The symptoms had disappeared completely at the last follow-up. At the last follow-up, the Japanese Orthopaedic Association score was 10 points in 5 cases and 9 points in 1, and the Kirkaldy-Willis criteria was excellent in all patients. No intervertebral disc space narrowing was observed in any patient at last follow up. In addition, there were no degenerative changes in the vertebral endplate and facet joint.
Lumbar disc herniation (LDH) is common in people in their fourth and fifth decades because the intervertebral disc undergoes degenerative changes with age. However, LDH in adolescents is uncommon and extremely rare in children of elementary school age1-6. Therefore, the incidence, disease characteristics and treatment results for LDH in elementary school-aged children are unclear. The clinical manifestations and treatment methods for LDH in children of elementary school age might be different from LDH in adults. Although previous follow-up studies on surgically-managed LDH in adolescents have reported good outcomes, there are few reports focusing on LDH in children of elementary school age. This study assessed the radiological, clinical features and surgical outcomes of six patients of elementary school age with LDH.
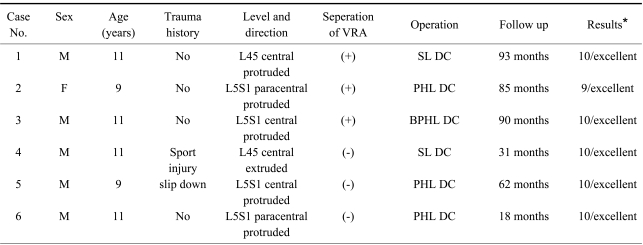
We reviewed a series of 6 patients under the age of 12 years, who underwent surgery for LDH at our institution between 1992-2002. Initially, all patients were treated conservatively. The indications for surgery were failure of conservative treatment for 3 months, intractable pain and/or progressive neurological impairment. The medical records, plain radiographs, CT scans and MRI were reviewed. The medical records were reviewed to confirm the clinical manifestation of LDH and the history of these patients. The plain radiographs, CT scans, and MRI were reviewed to determine the degree of disc herniation, extent of disc degeneration, ring apophysis fracture, and the presence of a congenital malformation. A telephone interview was conducted where needed. The average follow-up period was 63 months, ranging from 18 to 93 months. The results were analyzed using the Japanese Orthopaedic Association (JOA) score (Table 1)7 and Kirkaldy-Willis criteria (Table 2)8.
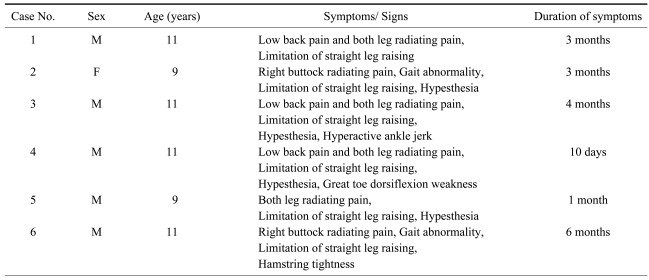
There were five boys and one girl with a mean age of 10.5 years (range, 9 years 11 months to 11 years 10 months). The symptoms developed spontaneously in 4 cases, as a result of a sport injury (Taekwondo) in one and a slip down in one. Disc herniation occurred at L4-L5 in 2 cases and L5-S1 and 4 cases. The direction of disc herniation was central in 4 cases (Fig. 1) and paracentral in 2 cases (Table 3). No patient had a congenital malformation or familial predisposition. All patients complained of radiating pain. Three, 2 and 2 patients complained of low back pain, buttock pain and an abnormal gait, respectively. The physical examination revealed a limitation of straight leg raising (SLR) in all cases, grade 4 great toe dorsiflexion in one case, hypesthesia in four, and a hyperactive ankle jerk in one. The mean symptom duration before visiting hospital was 12 weeks (Table 4).
Conservative treatments were performed initially. The patients were asked to avoid aggravating physical activity. Oral medication, such as analgesics, muscle relaxants and NSAIDs, were administered. Physical therapy was also started. Unfortunately, the treatment failed to relieve the symptoms. In 4 patients, conservative treatment for 3 months failed, and one patient had intractable pain. The remaining patient had progressive motor weakness. Therefore, surgery was performed on the six patients. The surgical findings revealed a protruding disc in five cases and a ruptured disc in one. In addition, separation of the vertebral ring apophysis was observed in 3 cases (Fig. 2). A partial hemilaminectomy and discectomy, subtotal laminectomy and discectomy, and bilateral hemilaminectomy and discectomy were performed in 3, 1 and 1 case, respectively. All fractured apophyseal fragments (3 cases) were removed concurrently when the discectomy was performed. The patients were followed-up for more than 1 year and the mean follow-up period was 63 months. The symptoms had disappeared completely at the last follow-up. The mean symptom duration after surgery was 16 weeks and the mean time until return to school was 5 weeks. There were no complications. The JOA score at the last follow-up was 10 points in 5 cases and 9 points in 1 case. All patients were excellent according to the Kirkaldy-Willis criteria (Table 3). No intervertebral disc space narrowing was observed at last follow up, and no degenerative changes in the vertebral endplate and facet joint were noted.
When the upper age limit of 12 years is used, very few cases of LDH have been reported in the literature. The first case of a herniated disc in a child of twelve years was reported by Wahren9 in 1945. Patrizio et al.4 reported that only three out of 129 cases under the age of 12 underwent surgery for lumbar disc herniation. Therefore, the six cases in this study are believed to be significant.
The causes of LDH in elementary school age are still unclear. Several primary causative factors have been suggested, such as trauma, congenital malformation, familial predisposition and vertebral slipping epiphysis. Trauma is frequently reported as the primary causative factor with variable incidence. In this study, 2 cases developed symptoms after trauma. However, 3 cases who had a separation of vertebral ring apophysis did not recall any traumatic history. Sovio et al.6 reported that a separation of vertebral ring apophysis was related to a series of minor trauma rather than an acute event. They reported that most patients did not recall any specific traumatic event. In addition to trauma, congenital malformation and familial predisposition have been suggested as etiologic factors, particularly in adolescents with lumbar disc herniation. Epstein and Lavine10 reported that 30% of juvenile lumbar herniation cases had congenital malformations, such as lumbarization, sacraization, lumbar Scheuermann's disease and spina bifida. Varlotta et al.11 calculated the relative risk of LDH before the age of 21 years, and found it to be approximately five times higher in patients with a positive family history. However, no patient in this study had a congenital malformation or a positive family history. Therefore, trauma, either an acute episode or repeated minor traumatic episodes, is believed to be the most likely factor accounting for the development of LDH in these children of elementary school age.
Epstein and Lavine10 reported that the chief complaint of juvenile HNP was low back pain and radiating pain: neurological deficit is not a common finding at that age. However, Shilito5 reported that the initial symptom of patients under the age of 15 were either back pain only or painless kyphoscoliosis in 80% of cases; only 20% of patients complained of sciatic pain. In our series, the most common symptom was radiating pain. Two patients had a gait abnormality. Hamstring tightness was observed on the physical examination in these two patients. Hamstring tightness is believed to be a characteristic symptom of juvenile LDH, particularly in children complaining of either radiating pain (sciatica) or low back pain6,12. Neurological deficits are not uncommon in this series, which is in contrast to a previous report of children and adolescent LDH patients.
Only few reports discussed the efficacy of conservative treatment. A favorable outcome was reported in 40~50% of cases managed conservatively13,14. In the absence of a neurological deficit, adolescent LDH can be safely managed non-surgically. DeOrio and Bianco15 recommended a discectomy in lumbar disc hernation in children and adolescents not responding well to conservative treatment or in patients with severe pain. The indications for surgery are a failure of conservative treatment for at least 3 months, intractable pain and/or progressive neurological impairment. The outcome of lumbar discectomy in children and adolescents is usually excellent immediately after surgery5,15. Shillito5 reported the relief of symptoms in 96% of patients. Globler et al.16 reported an 88% success rate of lumbar discectomy in children younger than 15 years of age. Smorgick et al.17 indicated that surgical discectomy provides satisfactory clinical results in adolescents with disc herniation at the mid to long term follow up period. However, Patrizio et al.4 stated that the outcomes of lumbar discectomy in children and adolescents was excellent in 93% immediately after discectomy but this decreased to 87% at the 12 year follow-up examination. In this series, the results after an average 63 months follow-up was 10 points in 5 cases and 9 points in 1 according to the JOA score, and excellent in all patients according to the Kirkaldy-Willis criteria. There was no patient whose symptoms worsened with time.
Radiating pain was the dominant and constant symptom with a limitation of SLR. Separation of the vertebral ring apophysis was the common finding. The surgical decision must depend on the clinical symptoms instead of the radiologic findings. Patients with symptoms that persist for more than 3 months or those with a progressive neurological deficit must be considered for a surgical discectomy.
References
1. Borgesen SE, Vang PS. Herniation of the lumbar intervertebral disk in children and adolescents. Acta Orthop Scand 1974;45:540ŌĆō549. PMID: 4281255.


2. Key JA. Intervertebral-disc lesions in children and adolescents. J Bone Joint Surg Am 1950;32:97ŌĆō102. PMID: 15401725.

3. Lowrey JJ. Dislocated lumbar vertebral epiphysis in adolescent children: report of three cases. J Neurosurg 1973;38:232ŌĆō234. PMID: 4694222.


4. Parisini P, Di Silvestre M, Greggi T, Miglietta A, Paderni S. Lumbar disc excision in children and adolescents. Spine (Phila Pa 1976) 2001;26:1997ŌĆō2000. PMID: 11547199.


5. Shillito J Jr. Pediatric lumbar disc surgery: 20 patients under 15 years of age. Surg Neurol 1996;46:14ŌĆō18. PMID: 8677479.


6. Sovio OM, Bell HM, Beauchamp RD, Tredwell SJ. Fracture of the lumbar vertebral apophysis. J Pediatr Orthop 1985;5:550ŌĆō552. PMID: 2931450.


7. Ishihara H, Matsui H, Hirano N, Tsuji H. Lumbar intervertebral disc herniation in children less than 16 years of age: long-term follow-up study of surgically managed cases. Spine (Phila Pa 1976) 1997;22:2044ŌĆō2049. PMID: 9306537.


8. Kirkaldy-Willis WH, Paine KW, Cauchoix J, McIvor G. Lumbar spinal stenosis. Clin Orthop Relat Res 1974;(99): 30ŌĆō50. PMID: 4274946.

9. Wahren H. Herniated nucleus pulposus in a child of twelve years. Acta Orthop Scand 1946;16:40ŌĆō42.

10. Epstein JA, Lavine LS. Herniated lmbar intervertebral discs in teen-age children. J Neurosurg 1964;21:1070ŌĆō1075. PMID: 14279827.


11. Varlotta GP, Brown MD, Kelsey JL, Golden AL. Familial predisposition for herniation of a lumbar disc in patients who are less than twenty-one years old. J Bone Joint Surg Am 1991;73:124ŌĆō128. PMID: 1824705.


12. Zhu Q, Gu R, Yang X, et al. Adolescent lumbar disc herniation and hamstring tightness: review of 16 cases. Spine (Phila Pa 1976) 2006;31:1810ŌĆō1814. PMID: 16845356.


13. Zamani MH, MacEwen GD. Herniation of the lumbar disc in children and adolescents. J Pediatr Orthop 1982;2:528ŌĆō533. PMID: 6219127.


14. Kurth AA, Rau S, Wang C, Schmitt E. Treatment of lumbar disc herniation in the second decade of life. Eur Spine J 1996;5:220ŌĆō224. PMID: 8886732.


15. DeOrio JK, Bianco AJ Jr. Lumbar disc excision in children and adolescents. J Bone Joint Surg Am 1982;64:991ŌĆō996. PMID: 6214560.


16. Grobler LJ, Simmons EH, Barrington TW. Intervertebral disc herniation in the adolescent. Spine (Phila Pa 1976) 1979;4:267ŌĆō278. PMID: 157533.


17. Smorgick Y, Floman Y, Millgram MA, et al. Mid- to long-term outcome of disc excision in adolescent disc herniation. Spine J 2006;6:380ŌĆō384. PMID: 16825042.


Fig.┬Ā1
T2 weighted MR images of an 11-year-old boy showing a central disc protrusion of the L4-5 with thecal sac compression.

Fig.┬Ā2
The fracture of vertebral ring apophysis at the upper endplate of S1. (A) CT sagittal image, (B) T2 weighted MR sagittal images, and (C) T1 weighted MR axial images.

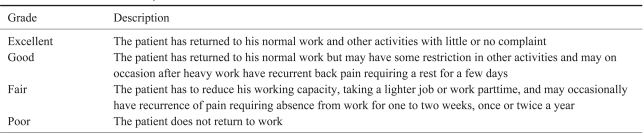
Table┬Ā1
The Japanese Orthopaedic Association's evaluation system for lower back pain syndrome (JOA Score)

- TOOLS
-
METRICS

-
- 3 Crossref
- Scopus
- 3,131 View
- 29 Download
- Related articles in ASJ
-
Impact of Acute Lumbar Disk Herniation on Sexual Function in Male Patients2022 August;16(4)
Recurrent Echinococcal Infection of the Lumbar Spine: An 11 Year Follow-up2013 March;7(1)
Interference of Detection Rate of Lumbar Disc Herniation by Socioeconomic Status2013 March;7(1)