Pyogenic Arthritis of the Facet Joint with Concurrent Epidural and Paraspinal Abscess: A Case Report
Article information
Abstract
Pyogenic arthritis of lumber spinal facet joints is an extremely rare condition. There are only 40 reported cases worldwide. Most cases were associated with history of paravertebral injection, which was not found in our patient. At the time of hospital admission, he had no abnormal magnetic resonance image findings. Two weeks later, he developed pyogenic facet joint arthritis associated with paravertebral and epidural abscess. This report is the first to describe delayed presentation of pyogenic arthritis associated with paravertebral abscess and epidural infection.
Introduction
To date, only 40 cases of pyogenic arthritis developed in the spinal facet joints have been reported worldwide. Furthermore, Magee et al. [1] reported a case of pyogenic arthritis in the spinal facet joint with simultaneous paraspinal muscle and epidural abscess. In Korea, Lee et al. [2] reported a similar case that developed following epidural steroid injection. However, there is no reported case of idiopathic pyogenic arthritis in the literature.
We herein report our experience of managing idiopathic pyogenic arthritis in the lumbar facet joint that resulted in paraspinal muscle abscess invading into the epidural space, and include a review of the literature.
Case Report
A 45-year-old male presented to our hospital with a one-week history of severe back pain, which became exacerbated 2 days prior to admission. Except for anemia, the patient did not have other past medical history. He was apyrexial on admission. The initial straight leg-raising test was negative. There were no other associated symptoms. His initial plain radiograph was unremarkable (Fig. 1). His leukocyte count (white blood cell count) was 14,800 cells per liter, erythrocyte sedimentation rate (ESR) was 120 mm/hr, and C-reactive protein (CRP) was elevated to 14.3. T2 weighted-images of magnetic resonance image (MRI) performed at another hospital showed slightly high signal density within the paraspinal muscles, for which intravenous antibiotics were administered (Fig. 2). Technetium bone scan performed on day 3 of admission was unremarkable. Two weeks after admission, the patient began to experience paraesthesia in both lower extremities. Straight leg raising test became positive, and pain in the vicinity of the spine became worsened. Plain radiograph of the spine showed slight osteolytic lesion in the facet joint that was further investigated by MRI, which demonstrated a paraspinal muscle abscess in the L2-5 vertebrae invading into the right facet joint, causing osteo-destructive changes and associated with dilatation of the epidural space in the vicinity of the fourth lumbar vertebra. An abscess-like mass showed low signal intensity on T1 weighted images, high signal intensity on T2 weighted images, and marginal enhancement on Gadolium enhanced images. It compressed on the dura in the spinal canal (Fig. 3). Surgical debridement was performed in response to the patient's neurological symptoms. Intraoperatively, the paraspinal muscle abscess was drained between the L3-5 lumbar vertebrae. In addition, L4-5 laminectomy, right medial facetectomy, and posterior decompression were performed to remove the epidural abscess (Fig. 4). Post-operatively, the patient experienced improvement in his neurological symptoms. MRI performed 2 weeks post-surgery showed resolution of the pyogenic mass, although paraspinal high signal intensity persisted, for which the patient was managed with antibiotics for 3 further weeks. The bacterial strain cultured were Staphylococcus, albeit without information on resistance (Fig. 5). Repeat blood test performed 6 weeks after surgery was unremarkable, and treatment was subsequently terminated.
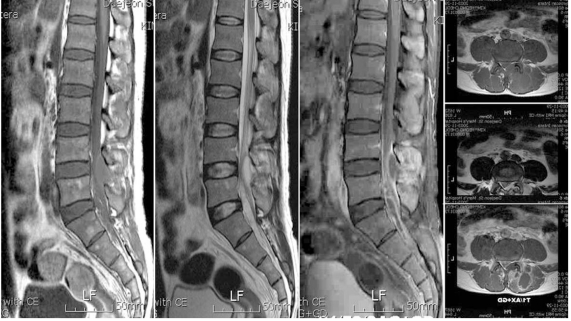
Two weeks after admission, follow up magnetic resonance image was performed. Mild signal increase in L4-5 area and no evidence of pus collection in saggital and axial images. Gadolinium enhancement was identified.

We performed surgery debrided the pyogenic collection. The patient's symptom was improved post-operatively.
Discussion
Pyogenic arthritis in the spinal facet joint is a very rare condition. Until now, approximately 40 cases have been reported in the literature. Recently, the development of pyogenic arthritis in the spinal facet joint following steroid injection to the facet joint has been reported in the literature [2]. Nonetheless, we thought it would be valuable to discuss our experience, because idiopathic pyogenic arthritis in the spinal facet joint is predominantly a secondary infection caused by pyogenic arthritis in the vertebral body. Nonetheless, recently, the concept is changing to hematogenous disseminating in more than half of the cases, and develop solely [3,4]. In addition, Muffoletto et al. [5] reported that in spinal infection, hematogenous pyogenic arthritis developed in 6 patients (4%), the predominant causative bacteria were Staphylococcus aureus and S. epidermidis, and both ESR and CRP were elevated in all cases. Our patient was apyrexial at the time of hospital admission, although elevated ESR and CRP were in evident. As such, the cause was secondary to infection.
Characteristic symptoms of pyogenic facet joint arthritis include persistent lower back pain not relieved by rest and fever. It has been reported that 90% of patients present with localized pain in the infected area, and fever was seen in 50% [3,6,7].
In this case, the initial severe localized tenderness and elevated CRP and ESR were clinically suspect. Nonetheless, infection could not be identified by initial MRI, which led to delayed diagnosis. One way to expedite diagnosis is to perform bacterial culture in conjunction with vertebral bone biopsy. It is thought that pyogenic arthritis of the posterior lumbar facet, as developed in our patient, does not invade the spine. As such, the possibility of negative findings in biopsy is high.
In regard to the dissemination of abscess from vertebral facet joints to adjacent muscles, Magee et al. [1] asserted that the cause was pyogenic arthritis in the facet joint secondary to direct dissemination of abscess within the muscles in the vicinity of the vertebrae, but such dissemination was insufficient to form an abscess in the intracanal epidura.
Baltz et al. [8] and Okada et al. [9] have reported similar experiences. They debrided abscesses disseminated to the intermuscular lesion of the psoas muscle of the anterior aspect of vertebral body, by performing anterior and posterior decompression. In our case, the abscess in the facet joint was located in the dorsal aspect of the epidural space; dissemination of intramuscular abscess was evident only within the muscles, and adequate decompression could only be achieved via the posterior route.
Regarding dissemination of abscess in the facet joint of the vertebrae to the epidural space, Lee et al. [10] reported that good outcome could be achieved using antibiotics cement beads. Our patient was treated by surgical debridement of the abscess followed by intravenous and oral antibiotics, and good outcome was obtained during the follow-up period.
Most pyogenic arthritis of the facet joint is considered to be secondary to spinal osteomyelitis of the vertebral body. Nonetheless, in some cases bacterial invasion of the facet joint by hematogenous dissemination without associated vertebral body osteomyelitis have been reported [10]. Based on these experiences, direct bacterial invasion is thought to co-exist with secondary dissemination of osteomyelitis in the vertebral body. Therefore, the diagnosis of pyogenic arthritis in the spinal facet joint is somewhat vague. Even if the initial MRI is unremarkable, imaging should be repeated if symptoms persist or deteriorate. In patients suspected of pyogenic arthritis of the facet joint following physical examination and blood tests, in addition to performing MRI, it is recommended to perform bacterial culture in conjunction with vertebral bone biopsy, supplemented by aggressive antibiotic therapy.


