|
 |
- Search
| Asian Spine J > Volume 7(4); 2013 > Article |
Abstract
Purpose
To evaluate the effect of the dynamic rotational plate to the intervertebral foraminal and discal height after anterior cervical discectomy and fusion.
Overview of Literature
There is no report regarding the changes of foraminal and discal height following cervical dynamic rotational plating.
Methods
We reviewed the outcomes of 30 patients (36 levels), who were followed-up for an average of 15 months (range, 12-57 months) after undergoing fusions with anterior cervical dynamic rotational plating for cervical radiculopathy, from March 2005 to February 2009. The changes of foraminal and intervertebral discal height of the operated levels were observed on oblique and lateral radiographs obtained at the preoperative, postoperative and follow-up examinations.
Results
The foraminal and discal height increased sufficiently, immediately following the operation. However, follow-up results showed gradual decrease in the foraminal and discal height. After 6 months of the surgery, they showed little difference compared with the preoperative heights. However, clinically, patients showed improvements in radiating pain during the follow-up period.
The static cervical plate was used to compensate the subsidence and gave sufficient biomechanical stability in surgical segments [1,2]. However, the static plate does not always provide stronger fixation than the dynamic plate [3]. The dynamic cervical plates prevent stress shielding, enable full load sharing better than static plates by maintaining axial load to the bone graft [4-6], and induce early bony union [7]. The types of dynamic plates are rotational plate, translational plate with slotted screw holes, and translational plate with plate telescope. The rotational plate has longitudinal rotation of a variable screw at the plate-screw interface.
The heights of intervertebral foramen and disc space restored by the operation were observed to decrease in the follow-up period in patients with anterior cervical discectomy and fusion [8-10]. The dynamic translational plate may cause segmental kyphosis and graft subsidence by load bearing [10], and the change in cervical intervertebral foraminal and discal height may occur. However, there is no report concerning the changes of foraminal and discal height, following cervical dynamic rotational plating. In this study, we evaluate the effect of the dynamic rotational plate to the intervertebral foramen and disc height after anterior cervical discectomy and fusion.
The retrospective study was conducted in a single institution. Thirty adult patients (thirty six segments) with degenerative cervical radiculopathy were selected, who have undergone anterior cervical fusion using allobone graft and dynamic rotational plate, from March 2005 to February 2009. All thirty six segments had disc herniations, and amongst them, 10 were combined with foraminal spurs. Those patients undergoing surgery for non-degenerative disease (trauma, infection, tumor, deformity, inflammation) were excluded. Zephir plate (Medtronic Sofamor Danek, Memphis, TN, USA), which is a dynamic rotational plate to enable the longitudinal rotation of a variable screw at the plate-screw interface was used. The average age of patients was 51.0, ratio of men to women was 19:11 and the average follow-up period was 15 months (range, 12 to 57 months). This study was approved by our university's institutional review board.
All patients underwent microscopic anterior cervical discectomy by anterolateral approach with a single surgeon. Total cervical discectomy, spur removal and removal of the posterior longitudinal ligament were done with the cervical alignment neutral. Partial uncinectomy were done in patients with foraminal spurs. Allobone graft was used as the graft substance. The proper size of the bone graft was measured with a surgical caliper, and bone graft was reformed by a rongeur. The end-plate of the recipient was partially removed before bone grafting. Then, bone graft was inserted while the interval of the intervertebral discs was slightly on traction. Bone graft size was 6 mm in all cases. The traction force was released, and the dynamic plate was inserted after the removal of a Caspar pin retractor. The size of the dynamic rotational plate used was 22.5 mm. The surgical wound was sutured with an absorbable suture. The Philadelphia brace was worn for six to eight weeks for postoperative external fixation.
Clinical symptom was observed each after 1, 3, 6, 12, and 24 months postoperatively. Visual analogue scale (VAS) score was used to assess the arm pain radiating to the upper extremities for cervical radiculopathy. Odom's criteria were assessed for patients with cervical radiculopathy.
The images were obtained with patients standing and looking straight ahead. Lateral radiographs were performed using standard radiographic techniques, wherein the tube was centered on the C3-C4 intervertebral disc. The radiographic film cassette was 72 inches from the tube and radiographs were taken without magnification. All oblique radiographs were taken on 45° oblique standing position with the fourth cervical vertebral body at the center with the beam angles of 15° cranially. Lateral and oblique views were taken after 1 day, 1, 3, 6, 12, and 15 months postoperatively. The height of the intervertebral foramen was measured at surgical segments on the oblique X-ray view. The height of the intervertebral disc was measured by averaging the length of three regions (anterior, middle, and posterior). The digital X-ray images were obtained on the PACS system (Π view, Infinitt, Seoul, Korea), which was used to obtain the measurements. Bone union was defined when there was a bony bridge across the graft site and no visible movements on the flexion and extension views.
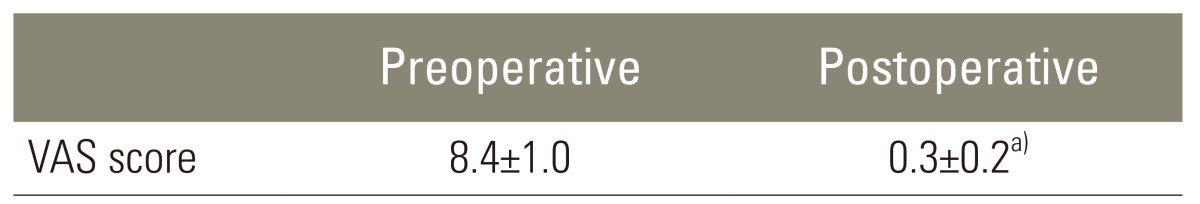
The average preoperative VAS score was 8.4±1.0 and it showed a decrement to 0.3±0.2, immediately following the operation (Table 1). Clinical outcome review of thirty patients with cervical radiculopathy confirmed that sixteen had excellent results, ten had good results and four had satisfactory results, based on the Odom's criteria. Three patients developed neck pain in the early postoperative period, and it was relieved with a pain-killer. There was no complication with surgical procedures and dynamic plates.
There was a bony bridge that crossed the graft site for all 30 patients who underwent the surgery. The bony union was achieved at 9.3 months after the operation (range, 6-12 months). Average preoperative intervertebral foraminal height was 11.6±1.7 mm on the right, and 11.4±1.7 mm on the left. Postoperative measures were increased to 13.4±1.7 mm and 12.8±1.8 mm, respectively, which showed statistically significant difference (p<0.05) (Table 2). However, follow-up results showed gradual tendency to decrease in the intervertebral foraminal height, which showed increments immediately after the operation. At 12 months after the surgery, it showed little difference compared with the preoperative data, as to be 11.7±1.7 mm for the right side and 11.4±1.7 mm for the left side (p>0.05) (Table 2). However, clinically, patients showed no increase in the radiating pain at the follow-up period. Preoperative average intervertebral disc height was 5.0±1.0 mm, and postoperatively, 7.3±1.0 mm, which indicates an increment of intervertebral disc height (p<0.05) (Table 3). Continuous decrease in the intervertebral discal height is observed during the follow-up period; however, the final height at the 15 months-follow-up showed little difference with preoperative measures (p>0.05) (Table 3). The height of the intervertebral disc was measured by averaging the length of three regions (anterior, middle, and posterior). There was no difference among the three regions at the radiographs taken after 1, 3, 6, 12, and 15 months postoperatively. It is estimated that the continuous decrement in the intervertebral disc height is attributed to reformation and resorption at the intervertebral graft.
The dynamic plate was designed in which the screws slide dynamically in the direction of the subsidence occurrence, whereas the static plate locks the screws to the plate to fuse. The slide in the dynamic plate reduced the chance of screw loosening and breakage, which may frequently occur with the static plate. Also, it reduces the axial compressive pressure to the plate biomechanically, increasing the axial compressive pressure of the grafted bone [4-6], enabling early bony fusion as a result [7]. The bone graft for anterior cervical discectomy and fusion restores the intervertebral disc height and foraminal height [8,11], and the postoperative restored height of the intervertebral foramen and disc space was observed to decrease during the follow-up [8,9]. The dynamic translational plate may cause segmental kyphosis and graft subsidence by load bearing [10], and the change in cervical intervertebral foraminal and discal height may occur. However, there is no previous report concerning the changes of foraminal and discal height, following cervical dynamic rotational plating. This study investigated the change in the radiographic measures of intervertebral foraminal and discal height after cervical fusion using dynamic rotational plate.
Postoperatively, restored intervertebral foraminal and discal height decrease gradually after the operation. They maintain increased states compared with preoperative states until 6 months postoperatively, but after 6 months, they lost significant difference compared with preoperative heights. It might be explained by the fact that early bony union between the graft and the graft bed is attributable for the decreased height. The radiating pain based on the VAS score has improved postoperatively and it was statistically significant. The clinical outcome review based on the Odom's criteria showed excellent, good and satisfactory. No complication was observed, such as new or recurrent radicular symptoms in the follow-up period. There was no association between the recurrence of postoperatively relieved radicular symptoms and the postoperatively decreased height of intervertebral foramen and disc.
The change of restored foraminal height in this study confirmed the results of previous studies [8,9]. In the radiologic study regarding graft insertion without plate during the cervical discectomy and fusion, the mean height of the foramen was 8.2±2.7 mm preoperatively, 10.8±2.6 mm on the second postoperative day, and 8.1±1.5 mm after 18 months of follow-up [9]. In the radiologic study about carbon fiber cage insertion without plate in the cervical discectomy and fusion, the mean height of the foramen was 8.1±1.5 mm preoperatively, 9.7±1.4 mm on the first postoperative day, and 9.4±1.4 mm after 12 months of follow-up [8]. The current study confirms the result of previous reports. In the current study, there is no association between the decrease in postoperatively restored intervertebral foraminal height and the clinical outcomes. The increase of postoperative foraminal area by decompressing the uncinate process did not have any positive effect on the postoperative symptom relief during the follow-up [12]. It is assumed that the neurological recovery is attributable to the removal of the herniated disc, not to increasing the foraminal area.
The change of restored discal height in the current study was observed in the other studies [9,10,13]. In the radiologic study regarding graft insertion without plate in the cervical discectomy and fusion, the mean preoperative heights of the disc was 3.1±1.7 mm, 5.8±1.6 mm on the second postoperative day, and 2.6±1.7 mm at 18 months after the operation [9]. With patients who had allograft insertion with plate in the cervical discectomy and fusion, the mean preoperative heights of the disc was 5.3±1.1 mm, 7.5±1.9 mm on the early follow-up, and 7.0±1.8 mm at average 18.1 months after the operation [13]. In patients who had autogenous bone graft insertion with translational plate in the cervical discectomy and fusion, the median graft subsidence at 6 months was 1.3 mm per level [10]. However, there is no statistically significant association between a decrease in postoperatively restored intervertebral disc height and clinical outcomes based on the VAS score, Oswestry Disability Index and neck disability index [13].
As with any study, the present investigation may have several potential problems. First, it is a retrospective study. Therefore, we did not have a protocol for standardizing all radiographs. Patients were asked to hold their neck in a neutral position. Second, we tried to standardize how to take radiographs by the protocol that the radiographic film cassette was 72 inches from the tube and radiographs were taken without magnification. However, there was a possibility of magnification in the radiographs. It is better to use the ratio of the measured length than the measured length itself. Third, we did not evaluate the cervical computed tomography, which can show the precise area of the intervertebral foramen. Fourth, the comparative study with static plates was mandatory to evaluate the effectiveness of dynamic plates for intervertebral foraminal and discal heights. Additionally, a follow-up of longer than two years are better for the surgical results following anterior cervical discectomy and fusion with dynamic plates.
The authors retrospectively evaluated the cervical foraminal and discal height changes after anterior cervical discectomy and fusion with dynamic rotational plate. To our knowledge, this study is the first in which changes of foraminal and discal height over time are shown, following anterior cervical dynamic rotational plating. The foraminal height and intervertebral discal height restored sufficiently, immediately after the operation. However, after 6 months of the surgery, they showed little difference compared with the preoperative heights. However, clinically, patients showed no aggravation in radiating pain at the follow-up period.
In conclusion, anterior cervical discectomy and fusion using the dynamic plate is an effective treatment option, in that it preserves the intervertebral foraminal and discal height. Early fusion can be achieved, yet maintaining improvement of neurological symptoms. Therefore, dynamic plating should be considered a primary treatment option for the surgery in the cervical spine.
References
1. Böhler J, Gaudernak T. Anterior plate stabilization for fracture-dislocations of the lower cervical spine. J Trauma 1980 20:203–205. PMID: 7359594.


2. Caspar W, Barbier DD, Klara PM. Anterior cervical fusion and Caspar plate stabilization for cervical trauma. Neurosurgery 1989 25:491–502. PMID: 2797387.


3. Dvorak MF, Pitzen T, Zhu Q, Gordon JD, Fisher CG, Oxland TR. Anterior cervical plate fixation: a biomechanical study to evaluate the effects of plate design, endplate preparation, and bone mineral density. Spine (Phila Pa 1976) 2005 30:294–301. PMID: 15682010.


4. Brodke DS, Gollogly S, Alexander Mohr R, Nguyen BK, Dailey AT, Bachus a K. Dynamic cervical plates: biomechanical evaluation of load sharing and stiffness. Spine (Phila Pa 1976) 2001 26:1324–1329. PMID: 11426146.


5. Brodke DS, Klimo P Jr, Bachus KN, Braun JT, Dailey AT. Anterior cervical fixation: analysis of load-sharing and stability with use of static and dynamic plates. J Bone Joint Surg Am 2006 88:1566–1573. PMID: 16818983.

6. Fogel GR, Li Z, Liu W, Liao Z, Wu J, Zhou W. In vitro evaluation of stiffness and load sharing in a two-level corpectomy: comparison of static and dynamic cervical plates. Spine J 2010 10:417–421. PMID: 20338828.


7. Goldberg G, Albert TJ, Vaccaro AR, Hilibrand AS, Anderson DG, Wharton N. Short-term comparison of cervical fusion with static and dynamic plating using computerized motion analysis. Spine (Phila Pa 1976) 2007 32:E371–E375. PMID: 17545900.


8. Bartels RH, Donk R, van Azn RD. Height of cervical foramina after anterior discectomy and implantation of a carbon fiber cage. J Neurosurg 2001 95:40–42. PMID: 11453429.


9. Celik SE, Kara A, Celik S. A comparison of changes over time in cervical foraminal height after tricortical iliac graft or polyetheretherketone cage placement following anterior discectomy. J Neurosurg Spine 2007 6:10–16. PMID: 17233285.


10. Ghahreman A, Rao PJ, Ferch RD. Dynamic plates in anterior cervical fusion surgery: graft settling and cervical alignment. Spine (Phila Pa 1976) 2009 34:1567–1571. PMID: 19564766.


11. Murphy MA, Trimble MB, Piedmonte MR, Kalfas IH. Changes in the cervical foraminal area after anterior discectomy with and without a graft. Neurosurgery 1994 34:93–96. PMID: 8121574.


12. Shen FH, Samartzis D, Khanna N, Goldberg EJ, An HS. Comparison of clinical and radiographic outcome in instrumented anterior cervical discectomy and fusion with or without direct uncovertebral joint decompression. Spine J 2004 4:629–635. PMID: 15541694.


13. Kwon B, Kim DH, Marvin A, Jenis LG. Outcomes following anterior cervical discectomy and fusion: the role of interbody disc height, angulation, and spinous process distance. J Spinal Disord Tech 2005 18:304–308. PMID: 16021009.


- TOOLS
-
METRICS

- Related articles in ASJ
-
A Review of Finite Element Modeling for Anterior Cervical Discectomy and Fusion2023 October;17(5)