|
 |
- Search
| Asian Spine J > Volume 8(3); 2014 > Article |
Abstract
Purpose
We compared the accuracy of O-arm-based navigation with computed tomography (CT)-based navigation in scoliotic surgery.
Overview of Literature
No previous reports comparing the results of O-arm-based navigation with conventional CT-based navigation in scoliotic surgery have been published.
Methods
A total of 222 pedicle screws were implanted in 29 patients using CT-based navigation (group C) and 416 screws were implanted in 32 patients using O-arm-based navigation (group O). Postoperative CT was performed to assess the screw accuracy, using the established Neo classification (grade 0: no perforation, grade 1: perforation <2 mm, grade 2: perforation ≥2 and <4, and grade 3: perforation ≥4 mm).
Results
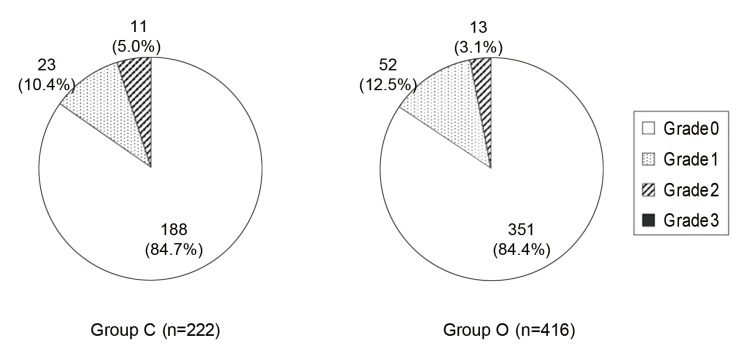
In group C, 188 (84.7%) of the 222 pedicle screw placements were categorized as grade 0, 23 (10.4%) were grade 1, 11 (5.0%) were grade 2, and 0 were grade 3. In group O, 351 (84.4%) of the 416 pedicle screw placements were categorized as grade 0, 52 (12.5%) were grade 1, 13 (3.1%) were grade 2, and 0 were grade 3. Statistical analysis showed no significant difference in the prevalence of grade 2.3 perforations between groups C and O. The time to position one screw, including registration, was 10.9±3.2 minutes in group C, but was significantly decreased to 5.4±1.1 minutes in group O.
Posterior spinal instrumented fusion is widely used in the treatment of progressive scoliosis. The correction anchor of scoliosis surgery has shifted from sublaminar wires and hooks to pedicle screw systems. The advantage of pedicle screws is that there is enough power to achieve sufficient correction [1]. The use of pedicle screw instrumentation in scoliosis surgery has increased over the last decade due to reports on the advantages of pedicle screws in enhancing the correction rate [2,3]. Several authors reported the advantages of pedicle screws over hooks in terms of the ability to achieve 3-column fixation, to de-rotate the spine, to provide improved coronal balance, and to lower pseudarthrosis and implant failure rates [2,4,5,6].
In contrast to the comparative efficacy of pedicle screws in correcting scoliosis, pedicle screw placement has increased risks of causing serious complications, such as injuries to the nerve roots or spinal cord, and major vessels [7,8,9,10]. Compared with patients with a straight spine, scoliosis patients have several different morphometric characteristics, including differences in pedicle dimensions and vertebral rotation because of the deformity [11,12,13,14,15], which increases the potential risk of screw misplacement [9,11,16,17].
Recently, clinical studies have demonstrated that computed tomography (CT) navigation can improve the accuracy of pedicle screw placement in surgery for scoliosis [18,19]. However, intervertebral anatomical relationships while the patient is prone during surgery may not match the preoperative CT data obtained while the patient is most often supine. This intervertebral motion may result in errors during surgery and a prolonged surgical time because of the need for point or surface registration for each vertebra [20]. The latest development, O-arm-assisted spinal navigation, is the only technology that includes the acquisition of high-resolution images and three-dimensional (3D) data sets on the operating table and allows fully automatic registration. To our knowledge, there are no reports in the literature comparing the results obtained using O-arm-based navigation for pedicle screw insertion with those obtained using CT-based navigation in scoliotic surgery. The purpose of the present study was to investigate the accuracy of O-arm-based pedicle screw insertion in comparison with the CT-based navigation technique in scoliotic surgery.
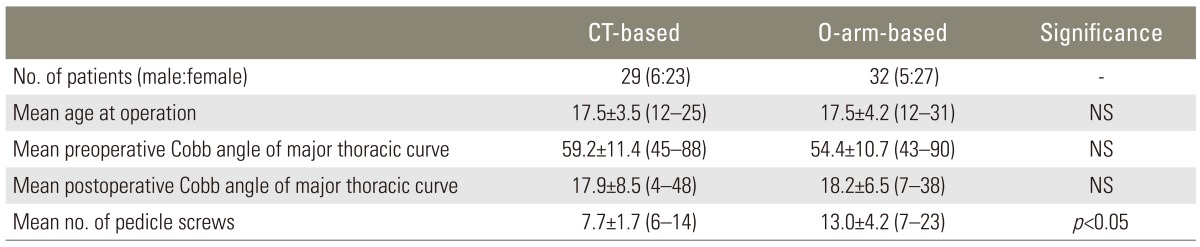
Seventy-five patients with scoliosis who underwent posterior instrumentation and fusion at Seirei Sakura Citizen Hospital, Chiba, Japan, from January 2010 to August 2011, were identified. Fourteen patients were excluded: 9 patients with congenital deformity and 5 with idiopathic scoliosis and no thoracic curve. Of the 75 patients, 61 with a thoracic curve were included in the study. All surgery was performed by two senior surgeons. Two hundred and twenty-two pedicle screws were implanted in 29 patients (6 males and 23 females) using CT-based navigation from Jan 2010 to Oct 2010 (group C) and 416 screws were implanted in 32 patients (5 males and 27 females) using O-arm navigation from Nov 2010 to Aug 2011 (group O). The etiology of scoliosis was mostly idiopathic; however, neuromuscular etiology was identified in 2 group C patients. In group O, mesenchymal and neuromuscular etiology was identified in 1 and 2 patients, respectively. The average Cobb angle of the major curve was 59.2°±11.4° (range, 45°-88°) in group C patients and 54.4°±10.7° (range, 43°-90°) in group O patients (mean±SD). The average numbers of pedicle screws were 7.7±1.7 (range, 6-14) in group C patients and 13.0±4.2 (range, 7-23) in group O patients. The average number of pedicle screws in group O patients was statistically greater than that in group C patients. There were no significant differences in the mean ages at surgery or the mean Cobb angles of the major thoracic curve between groups C and O patients (Table 1).
All patients were operated on by the same team of surgeons (T.K, T.A., and S.M.) using a 6.3 mm titanium rod and screw and hook instrumentation. Posterior correction surgery was performed using spinal cord monitoring for all the scoliosis surgeries. In group C patients, 3 to 4 pedicle screws were used at the apex on the convex side for the correction. Hooks were placed at the upper end of the fusion area, and pedicle screws were placed at the lower end of the fusion area. All screws were inserted using a navigation system. Applying a de-rotation force with convex pedicle screws, a left rod rotation maneuver was performed and 3 ultra-high molecular weight polyethylene tapes (Nespron cable system, Alfresa Pharma, Osaka, Japan) were tied to the concave rod. In group O patients, 3 or 4 pedicle screws were used at the apex on the concave side instead of the ultra-high molecular weight polyethylene tapes because we could confirm the positioning of the screw relative to the smaller concave pedicles during surgery using O-arm navigation.
A navigation system (Stealth Station, Medtronic, Sofamor Danek, Memphis, TN, USA) was used for correct screw placement and fixation of the thoracic and lumbar spine. The procedure for group C patients employed more than 6 registration points for 3 consecutive vertebrae, to shorten the surgical time (multilevel registration) [19]. Diameters and lengths of all pedicles into which the screws would be inserted were measured on preoperative 3D CT images. In group O patients, after a reference clamp was applied to the spinous process of the vertebra, CT data were obtained with automatic registration by 3D fluoroscopy (Fig. 1). After the navigation system was ready, an entry point was determined using a navigation probe, and a burr was used to make an entry hole. We reconfirmed the screw trajectory using a navigation probe, inserted a curved pedicle probe, and then inserted pedicle screws in some vertebrae above and below the vertebra on which the navigation reference frame had been placed. Reconfirmation of the accuracy of navigation was used as a reference for the vertebrae that was apart from the frame, by touching an anatomical landmark with the probe. If we suspected errors between the images on the O-arm system and the real landmarks, we obtained renewed intraoperative data for navigation [20]. The diameters of the pedicle screws were 4.5 mm, 5.5 mm, or 6.5 mm. The diameters and lengths of all pedicle screws were determined intraoperatively using the O-arm images. When pedicle perforation was detected before screw insertion, screw insertion was not performed. The total time from registration until complete insertion of all of the pedicle screws was measured in both groups. In group C patients, the measurement time started from the point merge, which was set by touching the anatomic landmarks. In group O patients, the measurement time started from the beginning of the scanning of the vertebra. Subsequently, the average time needed to insert one screw, including registration, was calculated.
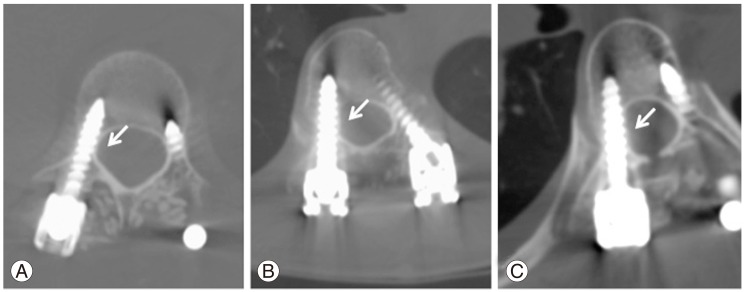
The accuracy of all pedicle screw placement was evaluated one week after surgery using reconstructed CT scan images at each screw axis. As defined by Neo et al. [21], pedicle screw positions were classified into 4 grades: grade 0, no perforation with the screw completely contained in the pedicle; grade 1, perforations <2 mm; grade 2, perforations ≥2 but <4 mm; and grade 3, perforations ≥4 mm, with grades 2 and 3 representing perforation (Fig. 2). Based on this grading system, the screw misplacement rates were determined.
Statistical analysis was performed using PASW ver. 18.0 (SPSS Inc., Chicago, IL, USA). Basic descriptive statistics (chi-squared and Fisher exact tests) were used when appropriate. Comparisons between the groups were made using a Mann-Whitney U test with a significance level set at 0.05.
After surgery, the Cobb angle of the major thoracic curve was corrected to 17.9°±8.5° in group C patients and 18.2°±6.5° in group O patients. There was no significant difference in the corrected Cobb angle between the 2 groups. Evaluation of the pedicle screw insertion position is demonstrated in Fig. 3. In group C patients, 188 (84.7%) of the 222 pedicle screw placements were categorized as grade 0, 23 (10.4%) as grade 1, 11 (5.0%) as grade 2, and 0 as grade 3. In group O patients, 351 (84.4%) of the 416 pedicle screw placements were categorized as grade 0, 52 (12.5%) as grade 1, 13 (3.1%) as grade 2, and 0 as grade 3. The perforation rates were 5.0% in group C and 3.1% in group O. There was no significant difference in the prevalence of grade 2.3 perforations between groups C and O patients. The time required for the registration procedure and insertion of one pedicle screw was 10.9±3.2 minutes in group C patients, but significantly decreased to 5.4±1.1 minutes in group O patients. No intraoperative complications, such as neurovascular injury or adverse clinical consequences, occurred as a result of pedicle perforation. No wound infection was observed.
Insertion of pedicle screws in scoliotic patients is a demanding technique because the pedicles of the thoracic spine are smaller than those in the lumbar spine, and the procedure carries the potential risk of neurological and vascular injuries. Especially in the concave side, the risk increases because the concave pedicles are thinner, more sclerotic, and dysplastic, with the spinal cord in direct contact with the medial wall of the pedicles [22]. Suk et al. [23] reported that the perforation rate of pedicle screws inserted by free hand in adolescent idiopathic scoliotic posterior fusion was 1.5%; however, only 10% of cases were evaluated by CT. Screw malpositioning was reported at a rate of 15.7% with the use of postoperative CT [22].
Several authors have reported that preoperative CT-based navigation can reduce the prevalence of pedicle screw malpositioning [18,19,24]. However, CT-based navigation has some limitations. Differences between intervertebral anatomical relationships as determined by the preoperative CT and by the intraoperative findings can cause errors. To overcome this difference, manufacturer protocols recommend registering each spinal level (single-level registration) separately. However, this registration technique can be associated with an increased operative time. To decrease the time, we performed multilevel registration [19]. Nevertheless, it still takes time to complete this registration because each anatomical landmark needs to be touched with a probe. Furthermore, selecting points on a three-dimensional model of the spine created by a computer system using the preoperative CT before surgery is burdensome for surgeons.
O-arm-based navigation has some benefits compared with CT-based navigation. O-arm-based navigation uses CT data from patients acquired in the operative position and obtains updated data as required. Selecting data from a 3D model of the spine created by a computer system using preoperative CT is not necessary. Surgeons are not dependent on preoperative CT in which the patient's position may vary from the surgical position in the operating room. The image quality of the O-arm system is almost comparable to that of the recent multidetector helical CT. These benefits can decrease potential navigation errors compared with CT-based navigation.
The perforation rates reported after operations that employed a navigation system are between 1.8% and 11.4% [18,24,25]. In the present study, the rate was as low as 5.0% in group C and 3.1% in group O. The perforation rate in both of our groups was comparable to that in previous studies. The perforation rate in group O patients was lower than that in group C patients; however, the difference was not significant. Both CT-based and O-arm-based navigation systems may reach a limit for increased placement accuracy for pedicle screws in scoliotic patients. Furthermore, surgeons tend to insert small concave pedicle screws in the apex in group O patients, while they often use ultra-high molecular weight polyethylene tapes instead of concave pedicle screws in group C patients. These concave pedicle screws are difficult to insert accurately in group O patients.
O-arm-based navigation does not require point-to-point surface matching, which increases the operative time in CT-based navigation. The O-arm navigation computer recognizes the optical tracker of both the O-arm and the reference frame that is attached to the patient's spine. Therefore, the registration time using the O-arm is decreased. In our study, the time required for the registration procedure and insertion of one pedicle screw was 10.9±3.2 minutes in group C patients, but this was significantly decreased to 5.4±1.1 minutes in group O patients. Because it is not necessary to preoperatively select reference points from 3D models when using O-arm navigation, the burden for surgeons is decreased. The O-arm technique is also less invasive for patients.
However, the O-arm technique has some drawbacks. The large size of the O-arm occupies much more space compared with conventional CT-based navigation. Furthermore, the O-arm needs additional special staff to operate it. Second, increased radiation exposure is a problem for patients. Lange et al estimated that spinal procedures that require up to 6 lumbar cone-beam CT scans on small patients impart a radiation dose that is within the range of the dose imparted by a single abdominal CT scan of the abdomen [26]. The increase in radiation dose using O-arm navigation should be studied further. Comparing the merits of O-arm navigation for avoiding perforation by pedicle screws and the disadvantages of increased radiation exposure is difficult. For the operative staff, the exposure is nearly zero because the whole surgical team leaves the operation room during the CT scan. Regarding the cost, Sanborn et al. [27] reported that using the O-arm for confirming pedicle screw placement was the most cost-effective strategy compared to neurophysiological monitoring and isocentric fluoroscopy.
To our knowledge, this is the first report to compare the accuracy of screw placement by CT-based navigation and O-arm-based navigation for scoliotic patients. O-arm- and CT-based navigation techniques have comparatively high accuracy for pedicle screw placement. However, it is known that CT navigation-based techniques prolong the operative time [19,20]. The screw placement time using the O-arm-based technique can be reduced significantly compared with CT-based navigation. There may be some bias in our study because it could not be controlled in a randomized manner. Additionally, there is a learning curve for the navigation system assistance that may have influenced our results. A comparative study of CT- and O-arm-based navigation for more cases should be conducted. O-arm navigation can decrease the time for inserting pedicle screws without compromising the accuracy of pedicle screw placement in scoliotic patients.
O-arm-based navigation facilitates pedicle screw insertion as accurately as conventional CT-based navigation. The use of O-arm-based navigation successfully reduced the time needed for computer-assisted surgery, demonstrating advantages in safety and accurate pedicle screw placement for scoliotic surgery.
References
1. Lenke LG, Kuklo TR, Ondra S, Polly DW Jr. Rationale behind the current state-of-the-art treatment of scoliosis (in the pedicle screw era). Spine (Phila Pa 1976) 2008 33:1051–1054. PMID: 18449036.


2. Halm H, Niemeyer T, Link T, Liljenqvist U. Segmental pedicle screw instrumentation in idiopathic thoracolumbar and lumbar scoliosis. Eur Spine J 2000 9:191–197. PMID: 10905435.



3. Hamill CL, Lenke LG, Bridwell KH, Chapman MP, Blanke K, Baldus C. The use of pedicle screw fixation to improve correction in the lumbar spine of patients with idiopathic scoliosis. Is it warranted? Spine (Phila Pa 1976) 1996 21:1241–1249. PMID: 8727200.


4. Gaines RW Jr. The use of pedicle-screw internal fixation for the operative treatment of spinal disorders. J Bone Joint Surg Am 2000 82:1458–1476. PMID: 11057475.


5. Kuklo TR, Lenke LG, O'Brien MF, Lehman RA Jr, Polly DW Jr, Schroeder TM. Accuracy and efficacy of thoracic pedicle screws in curves more than 90 degrees. Spine (Phila Pa 1976) 2005 30:222–226. PMID: 15644761.


6. Lee SM, Suk SI, Chung ER. Direct vertebral rotation: a new technique of three-dimensional deformity correction with segmental pedicle screw fixation in adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2004 29:343–349. PMID: 14752361.


7. Lonstein JE, Denis F, Perra JH, Pinto MR, Smith MD, Winter RB. Complications associated with pedicle screws. J Bone Joint Surg Am 1999 81:1519–1528. PMID: 10565643.


8. Minor ME, Morrissey NJ, Peress R, et al. Endovascular treatment of an iatrogenic thoracic aortic injury after spinal instrumentation: case report. J Vasc Surg 2004 39:893–896. PMID: 15071460.


9. Papin P, Arlet V, Marchesi D, Rosenblatt B, Aebi M. Unusual presentation of spinal cord compression related to misplaced pedicle screws in thoracic scoliosis. Eur Spine J 1999 8:156–159. PMID: 10333156.



10. West JL 3rd, Ogilvie JW, Bradford DS. Complications of the variable screw plate pedicle screw fixation. Spine (Phila Pa 1976) 1991 16:576–579. PMID: 2053001.


11. Liljenqvist UR, Halm HF, Link TM. Pedicle screw instrumentation of the thoracic spine in idiopathic scoliosis. Spine (Phila Pa 1976) 1997 22:2239–2245. PMID: 9346144.


12. O'Brien MF, Lenke LG, Mardjetko S, et al. Pedicle morphology in thoracic adolescent idiopathic scoliosis: is pedicle fixation an anatomically viable technique? Spine (Phila Pa 1976) 2000 25:2285–2293. PMID: 10984779.


13. Smith RM, Pool RD, Butt WP, Dickson RA. The transverse plane deformity of structural scoliosis. Spine (Phila Pa 1976) 1991 16:1126–1129. PMID: 1948404.


14. Xiong B, Sevastik B, Sevastik J, Hedlund R, Suliman I, Kristjansson S. Horizontal plane morphometry of normal and scoliotic vertebrae. A methodological study. Eur Spine J 1995 4:6–10. PMID: 7749910.


15. Xiong B, Sevastik B, Willers U, Sevastik J, Hedlund R. Structural vertebral changes in the horizontal plane in idiopathic scoliosis and the long-term corrective effect of spine instrumentation. Eur Spine J 1995 4:11–14. PMID: 7749899.


16. Heini P, Scholl E, Wyler D, Eggli S. Fatal cardiac tamponade associated with posterior spinal instrumentation A case report. Spine (Phila Pa 1976) 1998 23:2226–2230. PMID: 9802166.


17. Suk SI, Lee CK, Kim WJ, Chung YJ, Park YB. Segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis. Spine (Phila Pa 1976) 1995 20:1399–1405. PMID: 7676339.


18. Kotani Y, Abumi K, Ito M, et al. Accuracy analysis of pedicle screw placement in posterior scoliosis surgery: comparison between conventional fluoroscopic and computer-assisted technique. Spine (Phila Pa 1976) 2007 32:1543–1550. PMID: 17572625.


19. Takahashi J, Hirabayashi H, Hashidate H, Ogihara N, Kato H. Accuracy of multilevel registration in image-guided pedicle screw insertion for adolescent idiopathic scoliosis. Spine (Phila Pa 1976) 2010 35:347–352. PMID: 20075780.


20. Ishikawa Y, Kanemura T, Yoshida G, et al. Intraoperative, full-rotation, three-dimensional image (O-arm)-based navigation system for cervical pedicle screw insertion. J Neurosurg Spine 2011 15:472–478. PMID: 21761967.


21. Neo M, Sakamoto T, Fujibayashi S, Nakamura T. The clinical risk of vertebral artery injury from cervical pedicle screws inserted in degenerative vertebrae. Spine (Phila Pa 1976) 2005 30:2800–2805. PMID: 16371908.


22. Hicks JM, Singla A, Shen FH, Arlet V. Complications of pedicle screw fixation in scoliosis surgery: a systematic review. Spine (Phila Pa 1976) 2010 35:E465–E470. PMID: 20473117.


23. Suk SI, Lee SM, Chung ER, Kim JH, Kim SS. Selective thoracic fusion with segmental pedicle screw fixation in the treatment of thoracic idiopathic scoliosis: more than 5-year follow-up. Spine (Phila Pa 1976) 2005 30:1602–1609. PMID: 16025028.


24. Sakai Y, Matsuyama Y, Nakamura H, et al. Segmental pedicle screwing for idiopathic scoliosis using computer-assisted surgery. J Spinal Disord Tech 2008 21:181–186. PMID: 18458587.


25. Rajasekaran S, Vidyadhara S, Ramesh P, Shetty AP. Randomized clinical study to compare the accuracy of navigated and non-navigated thoracic pedicle screws in deformity correction surgeries. Spine (Phila Pa 1976) 2007 32:E56–E64. PMID: 17224800.


26. Lange J, Karellas A, Street J, et al. Estimating the effective radiation dose imparted to patients by intraoperative cone-beam computed tomography in thoracolumbar spinal surgery. Spine (Phila Pa 1976) 2013 38:E306–E312. PMID: 23238490.


27. Sanborn MR, Thawani JP, Whitmore RG, et al. Cost-effectiveness of confirmatory techniques for the placement of lumbar pedicle screws. Neurosurg Focus 2012 33:E12PMID: 22746229.

Fig. 1
Navigation images using O-arm providing horizontal and sagittal views during surgery. The blue guide shows the trajectory of the pedicle screw. The quality of the O-arm image is almost comparable to the recent multidetector helical computed tomography scans.
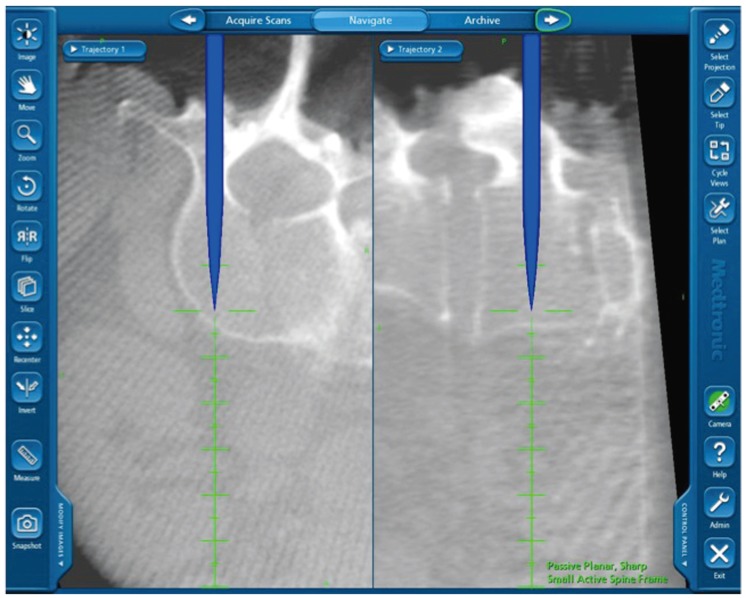
Fig. 2
Postoperative computed tomography assessment of the pedicle screw position: grade 0, no perforation and the screw was completely contained in the pedicle (A); grade 1, perforations<2 mm (B); grade 2, perforations≥2 but <4 mm (C); and grade 3, perforations≥4 mm, with grades 2 and 3 representing perforation. In both groups C and D, no screw was categorized as grade 3 (A arrow, no perforation; B, C arrows, perforations).
- TOOLS