|
 |
- Search
| Asian Spine J > Volume 8(3); 2014 > Article |
Abstract
Purpose
To explore the impact of chronic low back pain (CLBP) on individuals' quality of life; to understand current treatment practices and level of satisfaction with treatment in patients with CLBP.
Overview of Literature
Assessing subjective, patient-reported outcomes such as quality of life is essential to health care research.
Methods
Influences of the CLBP were analyzed via a questionnaire, which contained the character of CLBP, effect of pain management, Korean version Oswestry Disability Index (K-ODI) and Korean version of 12-item Short Form Health Survey (SF-12v2).
Results
Of 3,121 subjects who responded, 67.3% had moderate to severe pain; 43.5% presented prolonged CLBP of more than two years; and 32.4% had suffered from sleep disturbance due to pain. 22.8% of the patients were not satisfied with current pain management. The mean K-ODI score was 37.63; and it was positively correlated with the mean pain intensity (r=0.6, p<0.001). The SF-12v2 result was negatively correlated with mean pain intensity (PCS: r=-0.5, p<0.001; MCS: r=-0.4, p<0.001) and also negatively correlated with the K-ODI score (PCS: r=-0.75, p<0.001; MCS: r=-0.5, p<0.001). The conformity between patients and doctors in pain assessment was fair (╬║=0.2463).
Low back pain (LBP) and associated disabilities constitute a growing public health concern, particularly in industrialized countries [1]. It is one of the three most common reasons for healthcare visits, with an episode in presumably up to 75% of the population at some point [2]. Most cases of LBP are not severe and resolves within a few days or within few weeks; but for about 6% to 10% of patients, the disease may become recurrent or chronic [3,4]. Chronic low back pain (CLBP) is an entity developing in patients with LBP which persists for more than 12 weeks, such that recovery is slow and uncertain [4]. Chronic low back pain is often poorly understood and difficult to treat and can have a significant influence on the patient's quality of life in various areas of everyday functioning. Chronic pain is a common condition, for which patients seek care from various health care providers. It causes much suffering and disability and is frequently mistreated or undertreated [5]. As the importance of pain control is emphasized, the Agency for Health Care Policy and Research, a US agency, has issued recommendations for the treatment of pain. Health care providers should view good pain control as a source of pride and a major responsibility in quality care [6].
In 2007, characteristics and management patterns of CLBP were investigated nationally by the Korean Society of Spinal Surgery. The society reported that 65% of patients were satisfied with current pain management. Unlike in the past, recent pain management has replaced nonsteroidal anti-inflammatory drugs (NSAIDs) by more powerful analgesics. With this change of treatment pattern, the purpose of this study is to evaluate the status of CLBP management by investigating the satisfaction with current pain management in patients with CLBP. Secondary purpose of this study is to document pain intensity evaluated by patients and doctors and to assess the disability and limitation of quality of life due to CLBP.
Patient recruitment and data collection were performed by 76 physicians at 62 outpatient clinical centers, of which 53 were general hospitals and 9 were specialized spine hospitals in the Republic of Korea. The study was conducted from October 2011 to January 2012; and 3,345 patients who had visited orthopedic outpatient centers for low back pain treatment were recruited. The inclusion criteria were adult male or female patients of twenty-years or older, with CLBP symptom duration of at least three months and whose pain was controlled with analgesics at the time of the survey. Here we defined chronic pain patient as: a patient whose pain has lasted for three months or longer; who experienced continuous pain within the last one week; and/or currently taking analgesics for pain treatment. Also the patients who were capable of understanding the questionnaire and who provided written informed consent were recruited. The exclusion criteria were patients who had spinal fracture within six months and spinal tumor or other malignancy, who had undergone spinal surgery within three months, who were taking medicine for psychiatric disorder and who had possibility of exaggerated complaints due to automobile or accident insurance.
After obtaining patient consent, patients responded to questionnaires on characteristics of CLBP, Korean version of Oswestry Disability Index (K-ODI) (Suppl. 1) and quality of life by Korean version of Short Form 12 Health Survey V2 (SF-12v2) (Suppl. 2).
The ODI was originally developed as a self-assessment score for low back pain patients, and is based on patient's subjective impression of his or her own state of disability. Though the questionnaire is rather dated, it has been validated, and its reliability and sensitivity to changes in functional status have been documented [7,8]. It is comprised of ten items, each of which is followed by six alternatives [7]. Each question is scored from 0 to 5, and the sum of the scores is then presented as percentage. Higher score of K-ODI means that the function has decreased.
The SF-12v2 is a multipurpose short-form survey with twelve questions, all selected from the SF-36 Health Survey (Ware, Kosinski, and Keller, 1996). It is consisted of eight domains, and the values in each domain contribute to physical and mental values (physical component score [PCS] and mental component score [MCS]), which provide glimpses into mental and physical functioning and overall health-related quality of life. PCS and MCS are computed using the score of twelve questions and range from 0 to 100, where 0 indicates the lowest level of health and 100 indicates the highest level of health [9].
Mean pain intensity was estimated by numeric rating scale (NRS), categorized into four groups: 0, pain free; 1-3, mild; 4-6, moderate; and 7-10, severe. The patient's satisfaction with current pain management was measured using a four-point Likert scale (very satisfied, satisfied, unsatisfied, very unsatisfied), and it was categorized into two groups (satisfaction group,very satisfied and satisfied; dissatisfaction group, unsatisfied and very unsatisfied).
Also main causative diagnosis of CLBP and current pain management, the degree of pain improvement, pain intensity, nature of pain and next treatment management plan were taken from doctors who managed patients with CLBP.
Demographic data is described with means┬▒standard deviations, median, minimum, maximum and ranges by descriptive statistics. The relationship between mean pain intensity and satisfaction with current pain management was evaluated by chi-square test. The relationship between mean pain intensity and K-ODI score was evaluated by analysis of variance (ANOVA) test. Pearson correlation coefficients were used for correlation analysis between mean pain intensity and other variables (SF-12v2, K-ODI). Kappa statistics were used to analyze conformity of mean pain intensity evaluation between patient and doctor. Wilcoxon sum test was used for analysis of difference between pain improvement evaluation between doctors and patients.
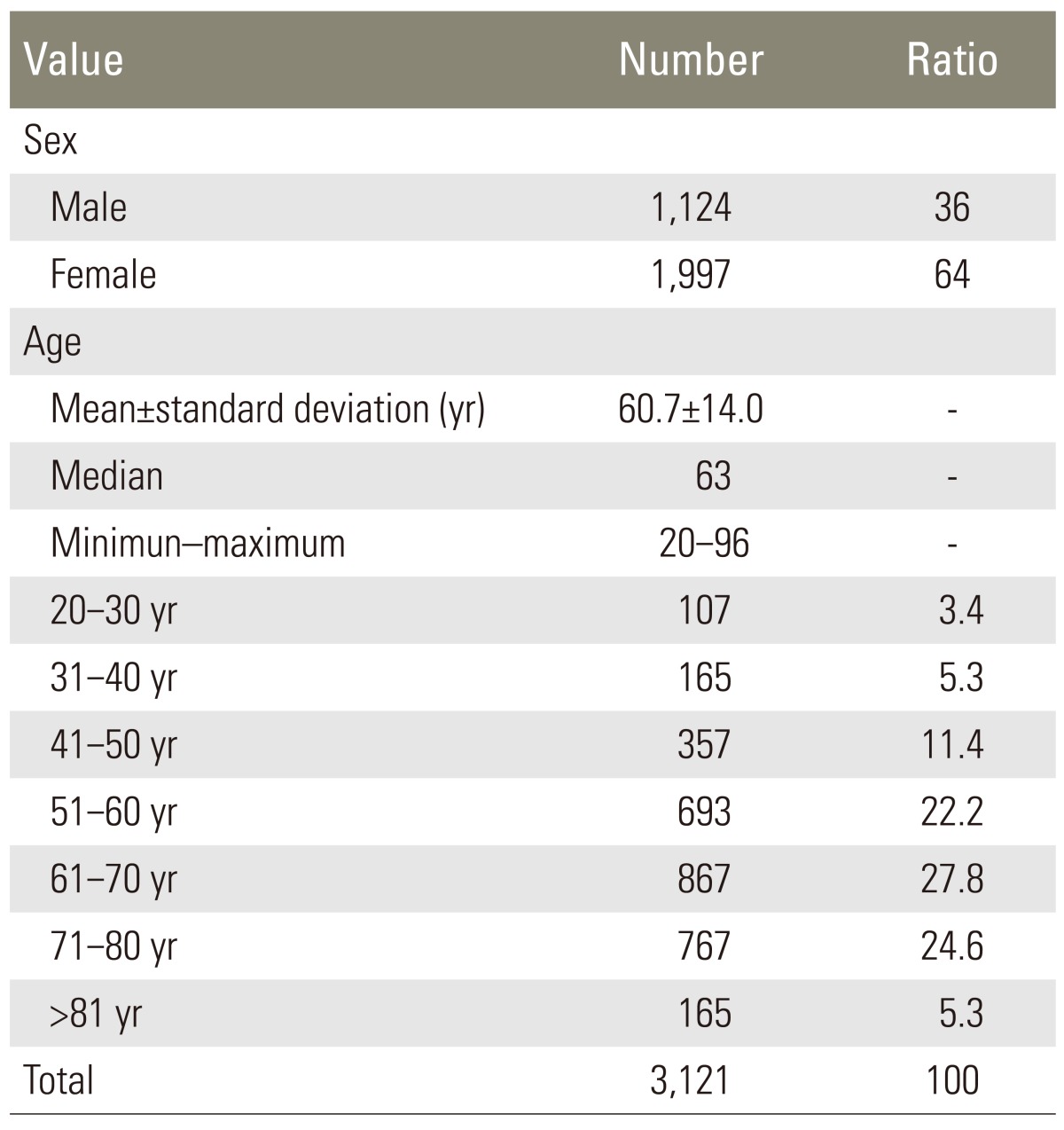
Two hundred and twenty-four patients were excluded (62 patients were under 19 years; 38 patients had LBP less than three months; and 169 patients did not complete the questionnaire). Overall data of 3,121 patients could be evaluated; and 1,997 (64.0%) were female. Mean age was 60.7┬▒14.0. The vast majority was between 50 years and 70 years, over 50 years (2,492/3,121, 79.8%), and 60s (867, 27.8%) (Table 1). The main diagnoses of patients with CLBP were spinal stenosis (47.31%) and herniated nucleus pulposus (23.52%) (Fig. 1).
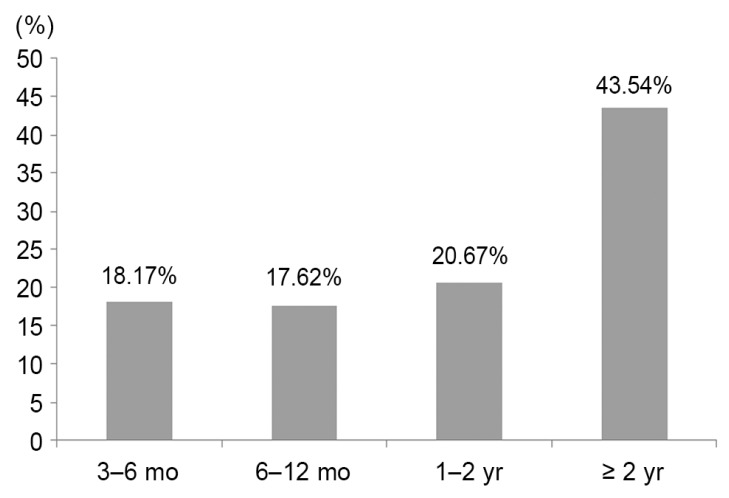
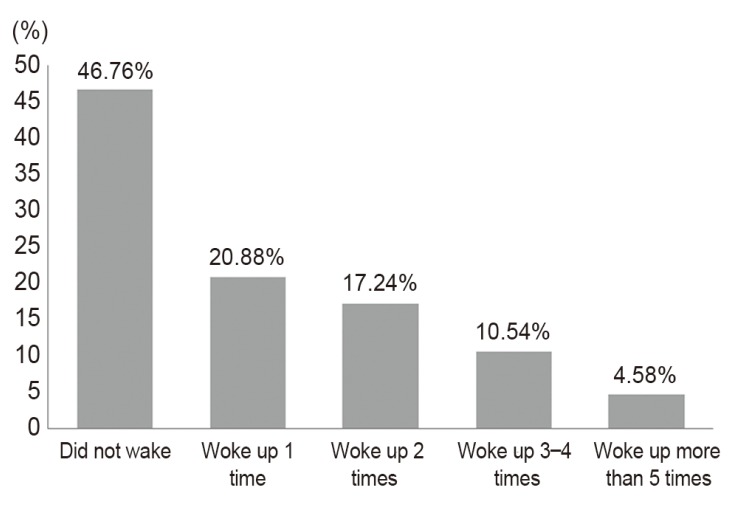
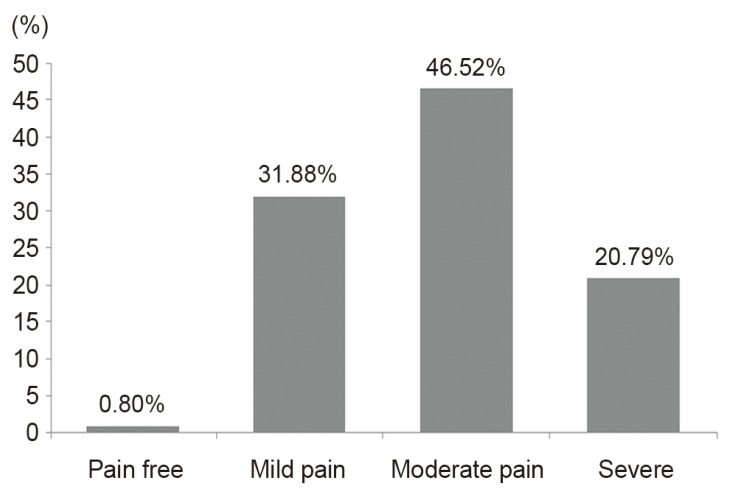
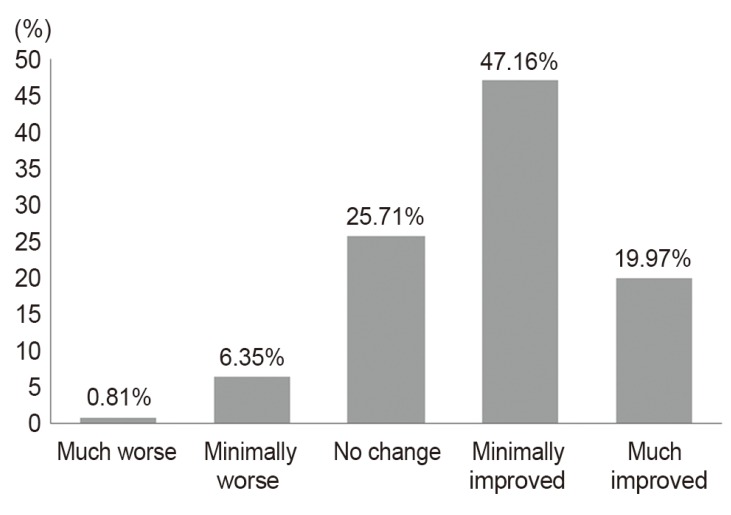
Nearly half of the patients (1,359, 43.5%) had prolonged LBP for at least two years (Fig. 2). The time during the day that the patients most frequently suffered LBP was from 7 PM to midnight (1,027, 35.1%) (Fig. 3). 32.4% of patients woke up from sleep at least two times due to LBP (Fig.4). The sleep disturbance was proportional to pain intensity (Fig. 5). And 67.3% of patients presented moderate to severe pain of the mean pain intensity during the last week (Fig. 6). For LBP, 56.5% of patients had moderate to severe pain; and for radiating pain, 49.8% of patients had moderate to severe pain. 67.1% of patients considered that their CLBP was improved after medication; and 32.9% of patients replied that their pain was not improved (Fig. 7). The ratio of patients who received treatment other than medication (injection therapy, physical therapy, therapeutic exercise) was 43.4%. Most patients (77.2%) were satisfied with their current pain management, but 22.8% of patients were not satisfied. The dissatisfaction percentage was higher as the pain severity grew (Fig. 8). The correlation between mean pain intensity and satisfaction with current pain management was statistically significant. This indicated that as pain intensity increased, satisfaction level significantly decreased (Table 2).
The mean K-ODI score of all patients was 37.63. A comparison of K-ODI scores of the four-group levels (divided by mean pain intensity) suggested that difference was statistically significant among each group (ANOVA test, p9<0.001) (Table 3). Also the correlation coefficient between the mean pain intensity and the mean K-ODI score showed highly positive correlation (Pearson correlation=0.61) (Table 4). Hence, the more severe the pain, the higher was the disability in the low back.
The mean PCS was 36.25, and the mean MCS was 41.77. The results of SF-12v2 were negatively correlated with mean pain intensity and K-ODI score. In addition, there was a positive correlation between SF-12v2 and patient's satisfaction on current pain management. However, SF-12v2 did not show a significant correlation with K-ODI (Table 2).
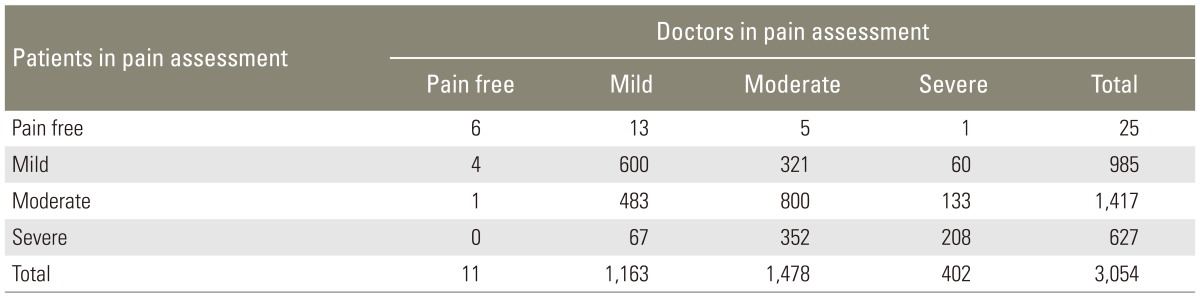
Most doctors reported that current medications were NSAIDs (1,724, 55.24%) and tramadol/acetaminophen extended release (713 cases, 22.85%). And 61.6% of doctors replied that they will maintain the current medication in response to a question of 'what analgesic will you prescribe next.' 17.5% of doctors had administrated a procedure in the past two weeks for CLBP management. In CLBP character assessed by doctors, 61.67% of patients had LBP with radiating pain and 38.33% had LBP without radiating pain. In pain intensity assessed by doctors, 61.6% of patients had moderate to severe LBP. The conformity between patients and doctors in pain assessment revealed that doctors were likely to underestimate a patient's pain intensity (╬║=0.2463) (Table 5). 68.1% of doctors considered that the pain was improved after medication. The assessment of pain improvement between doctors and patients was similar.
In our study, 43.5% of patients had suffered low back pain for more than two years. In a study that investigated treatment duration for work-related LBP in Korea [10], 70.7% of subjects were treated for LBP for more than three months, and 20.5% of subjects were treated for more than two years. In a survey of chronic pain in Europe [11], almost 60% of subjects had pain for more than two years. There is wide variance among these studies, but CLBP is often prolonged for more than two years. Alsaadi et al. [12] presented that prevalence of sleep disturbance in patients with LBP was 58.7%, and that the intensity of back pain was weakly associated with sleep disturbance. These results were different from our results (32.4%). The difference may be because our results did not include acute LBP.
67.3% of patients presented more than moderate pain in our study. Some studies of chronic pain, not CLBP only, reported that 80% to 100% of patients with chronic pain presented moderate to severe pain [11,13]. It is important that most CLBP patients complain of moderate or severe pain.
The body of evidence for chronic LBP has advanced with the development of reliable and valid patient self-reported outcome measures. However, it is often difficult to make comparisons between published studies, because different outcome measures have been utilized to assess pain, function and quality of life [14]. We sought to answer the clinical questions of how pain characteristics affected the assessment of pain intensity, patient's satisfaction and quality of life. In regard to pain management, most patients (77.2%) were satisfied with current pain management; and the relationship between pain intensity and patient satisfaction was inversely related. Regarding the impact of CLBP on quality of life, some health status surveys showed that the mean PCS was 47.1, in people whose age was between 55 and 64 years; and the mean PCS was not below 40, in people over 65 years of age. Similarly, the mean MCS was 53.9, for those whose age was between 55 and 64 years; and the mean MCS was not below 50, in people whose age was over 65 years [9]. On the other hand, mean PCS and MCS in our study were 36 and 41.5, respectively. As compared with health status for CLBP generally, our results revealed lower health status than these PCS and MCS. The disability and quality of life decreased when pain was increased; and relationship between disability and quality of life was inverse. These results were similar to other studies [11,15].
The doctors' assessment of pain intensity was lower than those of the patients' assessment. But there was no significant difference between doctors and patients evaluations of the mean pain intensity. Also there was no difference in assessment of pain improvement after medication between doctors and patients.
This study was limited to patients in outpatient clinics; and the results are not necessarily generalized to other settings. In addition, results may not be representative at a national level because of the limited number of participating centers.
The present survey has suggested that CLBP increases negative aspect of quality of life. Of total 22.8% of the patients were not satisfied with current pain management. Such needs to be taken more seriously by doctors for improvement in satisfaction and quality of life in patients with CLBP.
Supplementary Materials
Suppl. 1. Korean version of Oswestry Disability Index (K-ODI)
Supplementary material can be found via http://www.asianspinejournal.org/src/sm/asj-8-346-s001.pdf.
Suppl. 2. Korean version of Short Form 12 Health Survey V2 (SF-12v2)
Supplementary material can be found via http://www.asianspinejournal.org/src/sm/asj-8-346-s002.pdf.
References
1. Ruoff GE, Rosenthal N, Jordan D, Karim R, Kamin M. Protocol CAPSS-112 Study Group. Tramadol/acetaminophen combination tablets for the treatment of chronic lower back pain: a multicenter, randomized, double-blind, placebo-controlled outpatient study. Clin Ther 2003 25:1123ŌĆō1141. PMID: 12809961.


3. Von Korff M, Saunders K. The course of back pain in primary care. Spine (Phila Pa 1976) 1996 21:2833ŌĆō2837. PMID: 9112707.


4. Andersson GB. Epidemiological features of chronic low-back pain. Lancet 1999 354:581ŌĆō585. PMID: 10470716.


6. Carr DB, Jacox AK, Chapman CR. Acute pain management: operative or medical procedures and trauma. Clinical Practice Guideline. Rockville, MD: Agency for Health Care Policy and Research, Public Health Service, U.S. Department of Health and Human Services; 1992.AHCPR Pub. No. 92-0032.
7. Fairbank JC, Couper J, Davies JB, O'Brien JP. The Oswestry low back pain disability questionnaire. Physiotherapy 1980 66:271ŌĆō273. PMID: 6450426.

8. Fisher K, Johnston M. Validation of the Oswestry low back pain disability questionnaire, its sensitivity as a measure of change following treatment and its relationship with other aspects of the chronic pain experience. Physiother Theory Pract 1997 13:67ŌĆō80.

9. Office of Public Health Assessment Center for Health Data Utah Department of Health. 2001 Utah Health Status Survey report Health Status in Utah: The Medical Outcomes Study SF-12 [Internet]. Salt Lake City, UT: Office of Public Health Assessment Center for Health Data Utah Department of Health; 2004.cited 2014 Apr 20. Available from: http://health.utah.gov/opha/publications/2001hss/sf12/2001HSS_sf12.htm
10. Kim HS, Choi JW, Chang SH, Lee KS, Oh JY. Treatment duration and cost of work-related low back pain in Korea. J Korean Med Sci 2005 20:127ŌĆō131. PMID: 15716617.



11. Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain 2006 10:287ŌĆō333. PMID: 16095934.


12. Alsaadi SM, McAuley JH, Hush JM, Maher CG. Prevalence of sleep disturbance in patients with low back pain. Eur Spine J 2011 20:737ŌĆō743. PMID: 21190045.


13. Moulin DE, Clark AJ, Speechley M, Morley-Forster PK. Chronic pain in Canada: prevalence, treatment, impact and the role of opioid analgesia. Pain Res Manag 2002 7:179ŌĆō184. PMID: 12518174.


14. Chapman JR, Norvell DC, Hermsmeyer JT, et al. Evaluating common outcomes for measuring treatment success for chronic low back pain. Spine (Phila Pa 1976) 2011 36(21 Suppl): S54ŌĆōS68. PMID: 21952190.


15. Harker J, Reid KJ, Bekkering GE, et al. Epidemiology of chronic pain in denmark and sweden. Pain Res Treat 2012 2012:371248PMID: 22693667.



Table┬Ā2
The correlation among Pain intensity Korean version Oswestry Disability Index (K-ODI), Satisfaction Short Form 12 Health Survey V2

- TOOLS