|
 |
- Search
| Asian Spine J > Volume 8(5); 2014 > Article |
Abstract
Purpose
To evaluate characteristics of back muscle strength in patients scheduled for lumbar fusion surgery.
Overview of Literature
Little is known regarding muscle strength in patients with symptomatic lumbar degenerative diseases who require fusion surgery.
Methods
Consecutive 354 patients scheduled for posterior lumbar interbody fusion due to symptomatic degenerative diseases were approached for participation. 316 patients were enrolled. Before surgery, muscle strength was assessed by measuring maximal isometric extension strength at seven angular positions (0┬░, 12┬░, 24┬░, 36┬░, 48┬░, 60┬░, and 72┬░) and mean isometric strength was calculated. The Oswestry Disability Index (0-100) and visual analogue scale (0-100) for back pain were recorded. Muscle strength was compared according to gender, age (<60, 60-70, and Ōēź70 years) and scheduled fusion level (short, <3; long, Ōēź3).
Results
Isometric strength was significantly decreased compared with previously reported results of healthy individuals, particularly at extension positions (0┬░-48┬░, p<0.05). Mean isometric strength was significantly lower in females (p<0.001) and older patients (p<0.05). Differences of isometric strength between short and long level fusion were not significantly different (p>0.05). Isometric strengths showed significant, but weak, inverse correlations with age and Oswestry Disability Index (r<0.4, p<0.05).
Conventional open surgery is still a widely accepted method for the management of a variety of spinal disorders requiring spinal stabilization. However, the long incisions, extensive detachment of muscle from the spinal processes and subsequently prolonged wide retraction can result in back muscle injury and atrophy [1].
Patients with low back pain have decreased cross sectional area and reduced muscle strength of back muscle compared with healthy individuals [2]. Patients with scheduled for lumbar fusion surgery also have reduced muscle strength and muscle atrophy in the back region due to symptomatic chronic low back pain.
Back muscle strength has been considered as one of the most important parameters in patients with chronic low back pain and functional disability [3]. Numerous studies have demonstrated the relationships between a significant decrease of back muscle strength and chronic low back pain or limitation of daily activities [4,5].
To properly quantify back muscle strength before and after surgery, a variety of lumbar strength testing devices have been developed and used. Although controversies remain with regard to the type of devices or the patient's position during measurements [6,7], the isometric back muscle strength test is one of the most objective measurements of back muscle function [8,9] and an isometric lumbar extension machine was considered to have excellent reliability in the measurement of back muscle strength [4,7].
Many studies involving trunk muscle strength testing have used these isometric strength testing machines [8,9,10,11]. However, little is known concerning muscle strength of patients with symptomatic lumbar degenerative diseases scheduled for lumbar fusion surgery.
The objectives of this investigation were to evaluate characteristics of back muscle strength in patients scheduled for lumbar fusion surgery due to symptomatic lumbar degenerative diseases and to provide baseline data to physicians and for exercise specialists to aid in the planning of a rehabilitation program after lumbar fusion surgery.
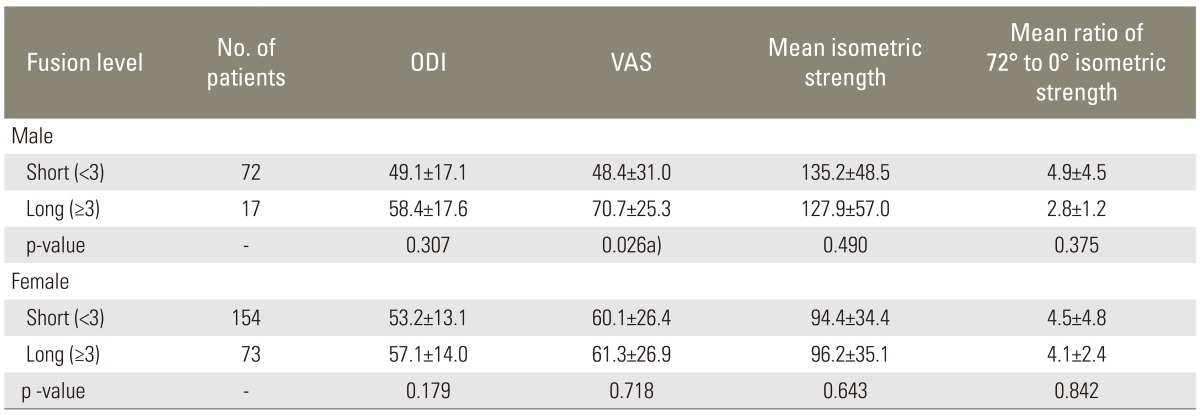
Between 2007 and 2010, consecutive 354 patients who failed adequate conservative management for more than 6 months and who were scheduled for elective posterior lumbar interbody fusion according to our indication for fusion surgery including lumbar spinal instability, neurogenic claudication, severe radicular pain, and progressive objective neurological deficit were approached to participate in the study. Inclusion criteria were no previous lumbar spinal surgery or fusion surgery, full range of motion in lumbar movement, no severe back pain, and consent for testing. Exclusion criteria were failure to properly follow the strength measurement protocol due to severe back pain and restriction of lumbar range of motion, prior simple decompression without instrumentation, and previous lumbar spinal surgery or fusion surgery. Thirty-eight patients were excluded. 316 patients (227 females; mean age, 64 years; age range, 40-79 years) were enrolled in this study (Fig. 1).
All data were prospectively collected before surgery. The Oswestry disability index (ODI) (range, 0-100) and back pain visual analogue scale (VAS) (range, 0-100) were used for evaluations. Body weight (kg) and body mass index (BMI; kg/m2) were also obtained. The 316 patients consisted of combined degenerative disc disease and spinal stenosis (n=179), degenerative spondylolisthesis (n=90), spondylolytic spondylolisthesis (n=34), and segmental instability with degenerative disc disease (n=13). Fusion surgery at the intervertebral disc level from T10-11 to L5-S1involved one segment (n=128), two segments (n=98), three segments (n=41), four segments (n=24), or five or more segments (n=25). This study protocol was approved by the institutional review board at our institution.
Prior to surgery, back muscle strength was evaluated by measurement of isometric strength using a lumbar extension machine (MedX, Ocala, FL, USA). Each test included measurement of the maximal voluntary isometric strength of the lumbar extensor muscles at seven angular positions (0┬░, 12┬░, 24┬░, 36┬░, 48┬░, 60┬░, and 72┬░) of lumbar flexion. Mean isometric strength and 72┬░/0┬░ ratio of isometric strength were calculated.
All subjects were instructed thoroughly on the method for accurate testing and performed warm-up exercises for 15 minutes before testing. Subjects were positioned according to the established protocol and were then asked to increase the lumbar extension torque over a period of 2 to 3 seconds. Once maximal tension had been achieved, subjects were instructed to maintain the contraction for an additional 1 to 2 seconds. After reaching maximum torque, they were asked to slowly decrease the torque. During contractions, concurrent visual feedback was provided on a video display screen interfaced with the machine and patients were verbally encouraged to give their maximum effort. All subjects practiced three times prior to accurate testing at 0┬░, 18┬░, and 54┬░. A 10-second rest period was provided between angle measurements and the maximal isometric voluntary extension of the back muscles was measured (foot-pounds). All subjects were assessed by the same specialist in our sports medicine center, who was blinded to other results. The reliability test was not performed.
A professional medical statistical consultant performed the statistical analyses using SAS version 9.1 (SAS Institute, Cary, NC, USA). Values were recorded as mean┬▒standard deviation. Lumbar extension strength was compared according to gender, age (<60, 60-70, and Ōēź70 years) and scheduled fusion level (short, <3; long, Ōēź3) and correlation analysis between variables was performed. The t-test, Mann-Whitney U-test, 1-way analysis of variance test, Kruskal-Wallis test, and Spearman rank correlation were used for statistical analyses. Significance was accepted for a p-value <0.05.
Characteristics of the patients and comparisons between male and female patients are displayed in Table 1. There were no significant differences between male and female patients in ODI, VAS, and ratio of 72┬░/0┬░ strength (p>0.05). However, the mean isometric strength was significantly lower in female patients than in male patients (p<0.001).
Isometric lumbar extension strength increased according to higher lumbar flexion angle and isometric strengths at all seven angular positions were significantly weaker in female patients than in male patients (p<0.05). In addition, compared to previously reported results of healthy individuals at our institution [12], isometric strengths of the patients showed significant decreases, particularly in lumbar extension positions (0┬░-48┬░, p<0.05) (Fig. 2).
When the patients were divided into three groups according to their age (<60, 60-70, and Ōēź70 years), no significant differences in ODI and VAS were observed between the three groups (p>0.05). However, significant differences were observed in mean isometric strength and 72┬░/0┬░ ratio of isometric strength (p<0.05) (Table 2). In both male and female patients, isometric strength was significantly weaker in older patients (p<0.05), except for the 72┬░ measurement in females (p=0.059) (Fig. 3).
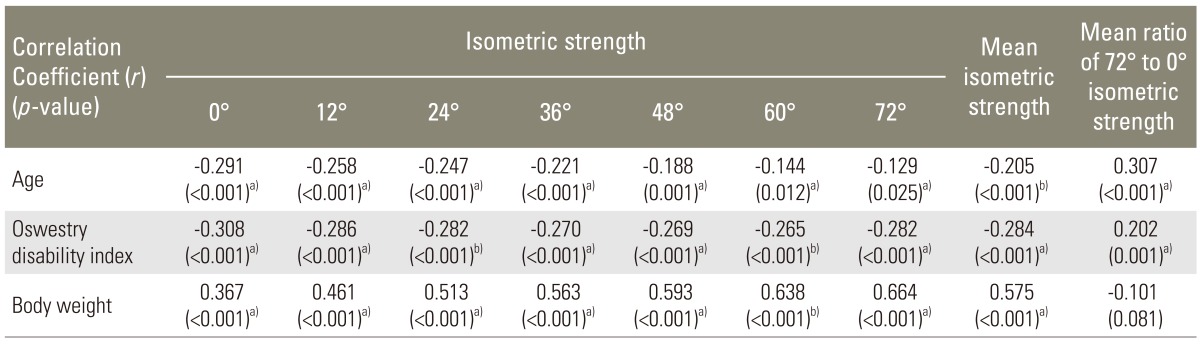
Differences between short and long level fusion patients were not significant (p<0.05), except in VAS of male patients (p=0.026) (Table 3).
Correlation analyses revealed significant negative associations of isometric lumbar extension strength with patient age and ODI, and a significant positive association with body weight at all seven angular positions (p<0.05) (Table 4).
This is the first study evaluating back muscle strength of patients with symptomatic lumbar degenerative diseases who required lumbar fusion surgery. In these patients, back muscle strength significantly decreased compared with healthy individuals, particularly at lumbar extension positions. Female and older patients also showed significantly lower isometric strengths, but differences of isometric strengths between short and long level fusion patients were not significant.
The variety of lumbar strength testing devices that have been developed constitute two major types: isokinetic and isometric. These measurements have been performed in patients with low back pain [10,13,14]. However, Gruther et al. [15] reported that isokinetic test devices are limited to muscle function assessment purposes in patient with low back pain because of learning effects. Assessment of lumbar muscle strength using isometric test device in patients with low back pain is reliable [7].
Like previous studies concerning back muscle strength in patients with chronic low back pain [16,17], presently significant decreases of isometric strength were evident in patients with symptomatic lumbar degenerative diseases. However, the decrease of muscle strength was much bigger at lumbar extension positions than at flexion positions. The muscle strength of patients with severe functional disability and low back pain were even lower at extension angular positions (0┬░-48┬░). The results suggest that isometric strength at extension positions could be more associated with lumbar dysfunctions and back pain of patients with symptomatic degenerative diseases than those at flexion positions.
In this study, the 72┬░/0┬░ ratio of isometric strength was also analyzed. The ratio of isometric strength indicates the balance of muscular strength throughout the range of motion (ROM). In general, a ratio >1.40:1 represents functional weakness in the extended portion of the ROM, and a ratio <1.40:1 represents functional weakness in the flexed portion of the ROM [18]. This ratio is reportedly higher in patients with back pain than in healthy individuals [19,20]. Presently, the mean 72┬░/0┬░ ratio was 4.5, which was even higher than that previously reported (2.3-2.9) in patients with chronic low back pain [12]. Because isometric strength of the patients with symptomatic degenerative diseases was weaker at lumbar extension positions than at flexion positions, the 72┬░/0┬░ strength ratio was very high. This indicated a severe muscle imbalance in trunk muscle strength. Muscle imbalance is a risk factor for patients with low back pain [21], and patients with scheduled lumbar fusion surgery require rehabilitation before and after surgery. In addition, the mean 72┬░/0┬░ strength ratio showed a significant positive association with patient age and ODI score. Thus, in patients with symptomatic lumbar degenerative diseases, the ratio of isometric strength is important in evaluating the clinical outcome after surgery or rehabilitation. Mean isometric strength of the patients with symptomatic lumbar degenerative diseases were compared with previously reported results of our institution [12]. A total of 845 persons (216 males) were included as healthy controls; their mean age (65 years; range, 60-78 years) was not significantly different with the patients in this study (p=0.242). Isometric strength of each gender were separately compared.
Although there were no significant differences in ODI and VAS according to gender and age, isometric strength was significantly lower in females and older patients with symptomatic degenerative diseases. These differences should be considered in pre- and postoperative rehabilitation programs. However, comparison of isometric strength according to the fusion length did not reveal significant differences in patients' isometric extension strength between short (<3) and long (Ōēź3) level fusion. In addition to this comparison, the authors also compared the isometric strength of between 1 vs. Ōēź2, <4 vs. Ōēź4, and <5 vs. Ōēź5 level fusion patients; there were also no significant differences. In general, back muscle strength of patients with multiple lumbar degenerative diseases is considered to be weaker than those of patients with short level diseases [22,23]. However, in this study, the comparative isometric strengths were not different. Symptomatic lumbar lesions, even in short level disease, might seriously affect back muscle strength. A separate analysis of patients with lumbar degenerative kyphosis could not be performed, due to its rarity.
Our results showed a significant inverse correlation of isometric lumbar extension strength with ODI score. Although the correlation was weak (r<-0.4), this result could be clinically important because there are few studies showing a direct association between back muscle strength and patients' functional disability [4,15].
The present study has several limitations. First, a direct comparison with a healthy control group was not performed. Although previous results of subjects with a mean age similar to that of the patients were used, interpretation of the results could be limited. Second, the reliability test for isometric strength measurements was not performed; however, many published studies have demonstrated excellent reliability of the isometric lumbar extension strength test, even in elderly persons or patients with chronic low back pain. Lastly, it was not easy to perform a precise evaluation of muscle strength of patients with symptomatic degenerative diseases. To minimize this limitation, one specialist in our sports medicine center evaluated the muscle strength of all patients and continuously encouraged patients to give their maximal effort using visual feedback on a video display of the machine, and patients who could not properly perform the protocol of strength measurement were excluded.
In patients with symptomatic degenerative disease in the lumbar spine, back muscle strength significantly decreased, particularly at lumbar extension positions and in females and older patients. However, differences of isometric strength according to fusion level were not significant. These results could aid in understanding of the characteristics of back muscle strength and in design of a rehabilitation plan in patients with lumbar degenerative diseases.
Acknowledgments
This study was supported by the Division of Sports Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
References
1. Kim DY, Lee SH, Chung SK, Lee HY. Comparison of multifidus muscle atrophy and trunk extension muscle strength: percutaneous versus open pedicle screw fixation. Spine (Phila Pa 1976) 2005;30:123ŌĆō129. PMID: 15626992.


2. Demoulin C, Crielaard JM, Vanderthommen M. Spinal muscle evaluation in healthy individuals and low-back-pain patients: a literature review. Joint Bone Spine 2007;74:9ŌĆō13. PMID: 17174584.


3. Hirsch G, Beach G, Cooke C, Menard M, Locke S. Relationship between performance on lumbar dynamometry and Waddell score in a population with low-back pain. Spine (Phila Pa 1976) 1991;16:1039ŌĆō1043. PMID: 1835159.


4. Imagama S, Matsuyama Y, Hasegawa Y, et al. Back muscle strength and spinal mobility are predictors of quality of life in middle-aged and elderly males. Eur Spine J 2011;20:954ŌĆō961. PMID: 21072545.


5. Sertpoyraz F, Eyigor S, Karapolat H, Capaci K, Kirazli Y. Comparison of isokinetic exercise versus standard exercise training in patients with chronic low back pain: a randomized controlled study. Clin Rehabil 2009;23:238ŌĆō247. PMID: 19218298.


6. Udermann BE, Mayer JM, Graves JE, Murray SR. Quantitative Assessment of Lumbar Paraspinal Muscle Endurance. J Athl Train 2003;38:259ŌĆō262. PMID: 14608437.


7. Roussel NA, Truijen S, De Kerf I, Lambeets D, Nijs J, Stassijns G. Reliability of the assessment of lumbar range of motion and maximal isometric strength in patients with chronic low back pain. Arch Phys Med Rehabil 2008;89:788ŌĆō791. PMID: 18374015.


8. Azghani MR, Farahmand F, Meghdari A, Vossoughi G, Parnianpour M. Design and evaluation of a novel triaxial isometric trunk muscle strength measurement system. Proc Inst Mech Eng H 2009;223:755ŌĆō766. PMID: 19743641.


9. Keller TS, Szpalski M, Gunzburg R, Spratt KF. Assessment of trunk function in single and multi-level spinal stenosis: a prospective clinical trial. Clin Biomech (Bristol, Avon) 2003;18:173ŌĆō181.


10. Kim YS, Park J, Hsu J, Cho KK, Kim YH, Shim JK. Effects of training frequency on lumbar extension strength in patients recovering from lumbar dyscectomy. J Rehabil Med 2010;42:839ŌĆō845. PMID: 20878044.


11. Ostelo RW, Costa LO, Maher CG, de Vet HC, van Tulder MW. Rehabilitation after lumbar disc surgery: an update Cochrane review. Spine (Phila Pa 1976) 2009;34:1839ŌĆō1848. PMID: 19602996.


12. Park WH, Lee BS. Isometric evaluation of the lumbar extensors in the normal Korean adult. Korean J Sports Med 2000;18:181ŌĆō192.
13. Urzica I, Tiffreau V, Popielarz S, Duquesnoy B, Thevenon A. Isokinetic trunk strength testing in chronic low back pain. The role of habituation and training to improve measures. Ann Readapt Med Phys 2007;50:271ŌĆō274. PMID: 17350132.


14. Keller A, Brox JI, Reikeras O. Predictors of change in trunk muscle strength for patients with chronic low back pain randomized to lumbar fusion or cognitive intervention and exercises. Pain Med 2008;9:680ŌĆō687. PMID: 18828199.


15. Gruther W, Wick F, Paul B, et al. Diagnostic accuracy and reliability of muscle strength and endurance measurements in patients with chronic low back pain. J Rehabil Med 2009;41:613ŌĆō619. PMID: 19565154.


16. Scheuer R, Friedrich M. Reliability of isometric strength measurements in trunk and neck region: patients with chronic neck pain compared with pain-free persons. Arch Phys Med Rehabil 2010;91:1878ŌĆō1883. PMID: 21112429.


17. Lee KW, Hwang JH, Bang HJ. Isometric evaluation of the lumbar extensors in chronic low back pain. J Korean Acad Rehabil Med 1997;21:1ŌĆō7.
18. Jones A, Pollick M, Graves J, et al. The lumbar spine. Santa Barbara, Calif: Sequoia communication; 1998.
19. Carpenter DM, Graves JE, Pollock ML, et al. Effect of 12 and 20 weeks of resistance training on lumbar extension torque production. Phys Ther 1991;71:580ŌĆō588. PMID: 1852797.


20. Tucci JT, Carpenter DM, Pollock ML, Graves JE, Leggett SH. Effect of reduced frequency of training and detraining on lumbar extension strength. Spine (Phila Pa 1976) 1992;17:1497ŌĆō1501. PMID: 1471008.


21. Lee JH, Hoshino Y, Nakamura K, Kariya Y, Saita K, Ito K. Trunk muscle weakness as a risk factor for low back pain. A 5-year prospective study. Spine (Phila Pa 1976) 1999;24:54ŌĆō57. PMID: 9921591.


22. Kang CH, Shin MJ, Kim SM, Lee SH, Lee CS. MRI of paraspinal muscles in lumbar degenerative kyphosis patients and control patients with chronic low back pain. Clin Radiol 2007;62:479ŌĆō486. PMID: 17398274.


23. Lee JC, Cha JG, Kim Y, Kim YI, Shin BJ. Quantitative analysis of back muscle degeneration in the patients with the degenerative lumbar flat back using a digital image analysis: comparison with the normal controls. Spine (Phila Pa 1976) 2008;33:318ŌĆō325. PMID: 18303466.


Fig.┬Ā1
Flow chart of the enrolled patients. PLIF, posterior lumbar interbody fusion; ROM, range of motion.
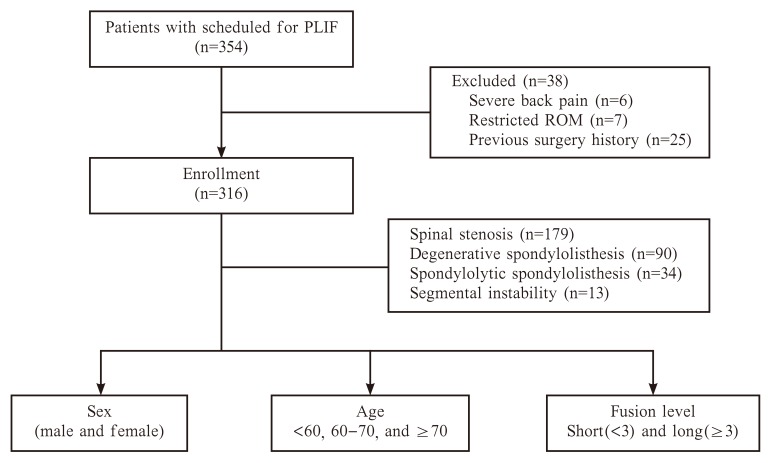
Fig.┬Ā2
In both genders, isometric strength of patients with symptomatic lumbar degenerative diseases were compared to those of healthy controls with a similar mean age. Isometric strengths of the patients significantly decreased, particularly in lumbar extension positions (0┬░-48┬░).
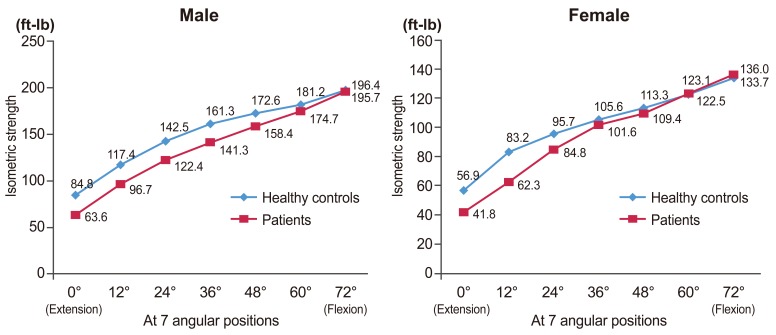
Fig.┬Ā3
Comparison of isometric strength according to age in male and female patients. At all seven angular positions, isometric strength was significantly weaker in older patients' groups (p<0.05), except in females at 72┬░ (p=0.059).