|
 |
- Search
| Asian Spine J > Volume 9(1); 2015 > Article |
Abstract
Study Design
Lumber disc arthroplasty is a technological advancement that has occurred in the last decade to treat lumbar degenerative disk diseases.
Purpose
The aim of this retrospective study was to establish the impact and outcomes of managing patients with lumbar degenerative disk disease who have been treated with lumbar total disc arthroplasty (TDA).
Methods
We reviewed the files of 104 patients at the Department of Neurosurgery in Colmar (France) who had been operated on by lumbar spine arthroplasty (Prodisc) between April 2002 and October 2008.
Results
Among the 104 patients, 67 were female and 37 were male with an average age of 33.1 years. We followed the cases for a mean of 20 months. The most frequent level of discopathy was L4-L5 with 62 patients (59.6%) followed by L5-S1 level with 52 patients (50%). Eighty-three patients suffered from low back pain, 21 of which were associated with radiculopathy. The status of 82 patients improved after surgery according to the Oswestry Disability Index score, and 92 patients returned to work.
The appropriate surgical technique to treat lumbar degenerative diseases has been controversial, particularly that for chronic lumbago. Advances in the field of lumbar spine surgery have transformed the management of lumbar degenerative disk diseases. Among these techniques, total arthroplasty through an anterior or anterolateral approach has been widely used by spinal surgeons [1,2,3,4,5,6,7,8,9,10,11,12,13,14,15,16,17,18,19,20,21,22]. The anterior approach allows complete access to the lumbar discs without incising paravertebral muscles and removing posterior structures. Therefore, this approach does not compromise biomechanical stability or functionality of posterior lumbar facets.
We present our experience with total disc arthroplasty for treating lumbar degenerative diseases and evaluate outcomes following this technique.
A total of 104 patients underwent total disc arthroplasty (Prodisc, Synthes Inc., West Chester, PA, USA) at the Department of Neurosurgery of Colmar in France from April 2002 to October 2008. All patients were included in the study. We studied the files of these patients retrospectively, and the clinical history, examinations, and radiological findings were reviewed for each patient (Fig. 1). Surgery was performed in the following circumstances: lumbalgia caused by chronic and invalidating discopathy, and resistance to 6 months of medical treatment in an adult <60 years suffering symptomatic discopathy lumbar or lumbosacral discopathy without associated sciatica [1,2,3,8,9,11,12,13,14,16,19]. Patients were evaluated during the preoperative period. The patients were examined clinically at 6 and 12 weeks postoperatively and evaluated with a visual analogue scale (VAS) ranging from 0 (no pain) to 10 (worst pain imaginable) and with the Oswestry disability index (ODI), which ranges from 0-100. All patients underwent X-ray imaging of the lumbar spine on week 6 postoperatively. Among the patients, 21 had undergone previous lumbar spine surgery using a posterior approach.
A transperitoneal approach was performed in 91 patients and an anterior paramedian retroperitoneal approach was used in 13 cases. Patients undergoing the transperitoneal approach were placed in the Trendelenburg position, and a transverse incision was made in the skin and peritoneum after muscle-splitting. The intraperitoneal organs were retracted, the prevertebral neurovascular structures (hypogastric nerve plexus, vena cava, and aorta) were identified, and the posterior layer of the peritoneum was opened. After meticulous dissection, the anterior longitudinal ligament and disk were incised, and a diskectomy was performed. The posterior longitudinal ligament was preserved if possible, and an artificial disc was placed in the intervertebral disc space. The incision for patients undergoing the anterior paramedian retroperitoneal approach was left paramedian oblique. The external oblique fascia and muscles were identified and opened, and the rectus muscle was retracted. The peritoneum was dissected and retracted medially. Then psoas muscle, left ureter, left iliac artery, and vein were identified and retracted, respectively. The remainder of the procedure was similar to that of the transperitoneal approach.
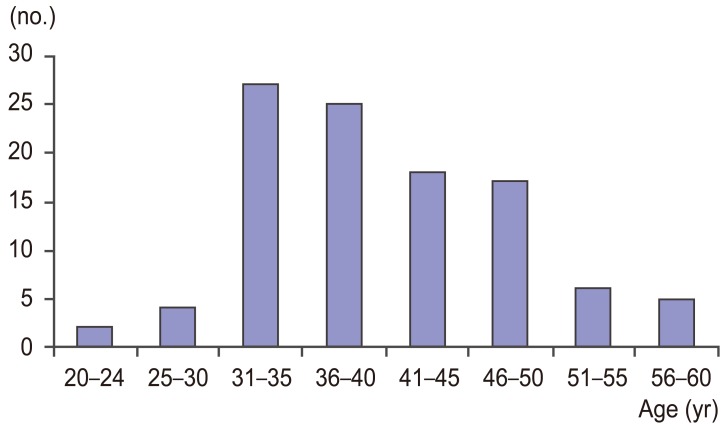
A total of 104 patients (67 females and 37 males; median age, 35.1 years; range, 20-58 years) were included (Fig. 2). Mean follow-up was 20 months (range, 3-38 months).
Twenty-one patients had been operated on previously using a posterior approach for different reasons, including disk herniation, lumbar canal stenosis, and other causes. We did not intervene surgically if the level had been instrumented previously. Eighty-three patients (79.81%) suffered from pure lumbago without radiculopathy, and 21 patients (20.19%) had associated radiculopathy.
All patients benefited from a magnetic resonance imaging (MRI) scan of the lumbar spine conducted at the time of diagnosis. We were compelled to carry out a discography in 22 patients because there were doubts about the symptomatic degenerated disc level.
More than one symptomatic degenerated disk level was detected in 17 cases; 13 patients with two levels and four patients with three levels.
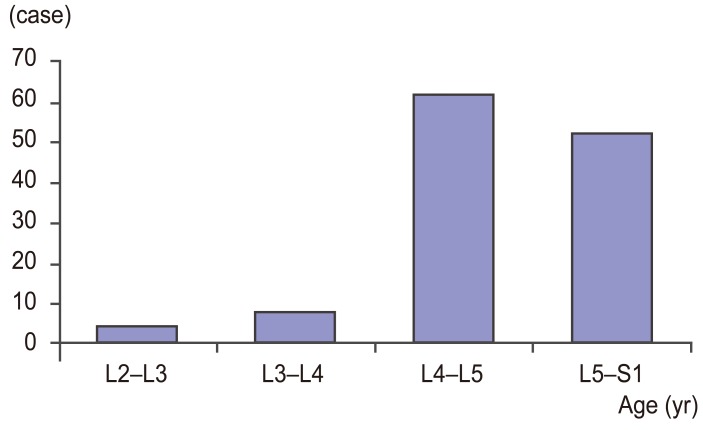
Clinical radiculopathy was discordant with symptomatic degenerated disk level in radiological findings of nine patients. The most frequent symptomatic degenerated disk level was L4-L5 (62 cases; 59.62%), followed by the L5-S1 level (52 cases; 50 %). Higher levels were less frequent with seven cases (6.73%) at the L3-L4 level and four cases (3.85%) at the L2-L3 level (Figs. 3, 4).
Eighty-seven patients (83.65%) underwent surgery for one level, 13 (12.50%) for two levels, and four patients (3.85%) underwent operations for three levels.
MRI showed the following results: 43 patients had Modic sign 0, 43 patients had Modic sign I, 15 patients had Modic sign II, and three patients had Modic sign III.
All patients had preoperative computed tomography angiography to assess the vascular system of the region as well as anteroposterior (AP) and lateral lumbar spine radiographs and dynamic X-rays.
The average length of stay in the hospital was 3.5 days (range, 2-15 days). Patients were encouraged to ambulate on day 1 and were authorized to restart their activities at the first consultation.
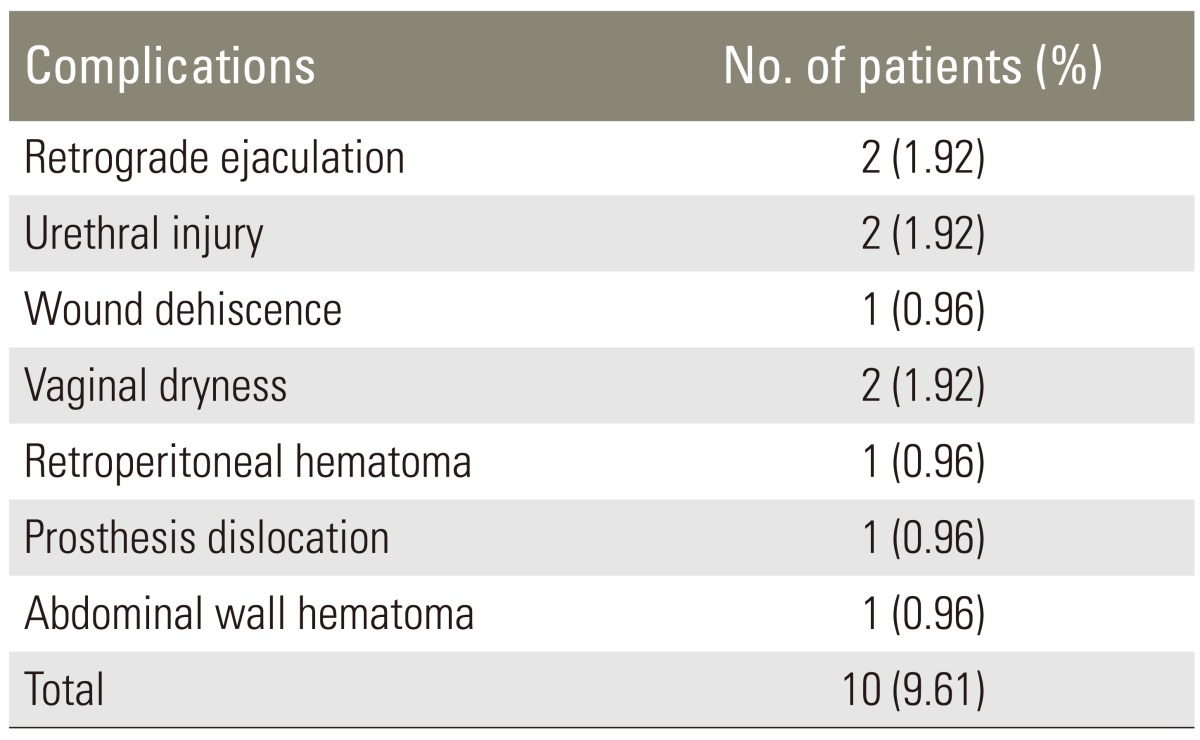
The postoperative complications are summarized in Table 1.
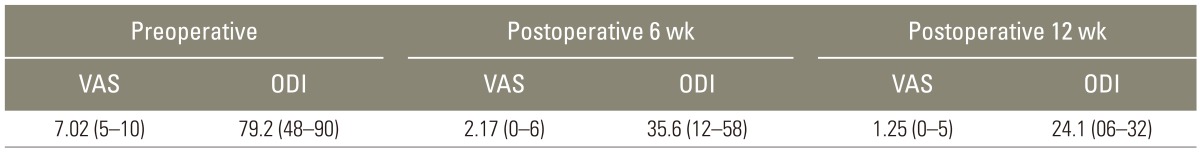
All patients responded to the VAS and the ODI before, during the immediate preoperative period, and 6 and 12 weeks after surgery. Table 2 summarizes the results of this evaluation. All patients improved after 6 weeks except one who lost 1 point on the VAS at 6 weeks but returned to the preoperative level at 12 weeks, and three patients did not improve on the VAS. All patients improved on the ODI at 6 and 12 weeks. Patients were followed up for a mean of 20 months clinically and radiologically every 3 months
Treatment for lumbalgia has been problematic for spine specialists, as the surgical treatment is controversial. According to Burke et al. [5], lumbar degenerative disc diseases lead to mechanical instability that stimulates nociceptive intradiscal fibers. This source of pain is removed by replacing the symptomatic degenerated disk with an artificial disc. In addition, mobility, disc height, and segmental stability are restored. The ProDisc was designed by Marnay in 1987 [3]. Thereafter, this technique spread rapidly, and several clinical trials were conducted in the USA. Numerous studies with positive results support this technique. Our results demonstrated satisfactory outcomes with significant improvement on the VAS and ODI. All patients were consulted 6 and 12 weeks postoperatively, and AP and lateral lumbar spine radiographs were obtained. Among the 104 patients, 51 (49.03%) returned to work within 6 weeks and 92 (88.46%) returned within 12 weeks. Forty-five patients had dynamic X-rays that confirmed persistence of the mobile section. Twenty-three patients participated in strenuous and regular sports activity before surgery. Among them, 19 (82.6%) started complete sports and physical activities after 12 weeks. Four patients were hospitalized in medical physical and rehabilitation centers. The minimum VAS pain score preoperatively was 5. Thirty-six (34.62%) patients had zero pain (VAS=0) 6 weeks postoperatively, and 68 (66.35%) had VAS scores ≤6. Among the patients with radiculopathy, 17 became asymptomatic (Table 3). The clinical radiculopathy was discordant with the symptomatic degenerated disk level in the radiological findings of nine patients. One study [9] suggested that patients with radiculopathy without herniation may be suboptimal candidates for the procedure.
Studies have reported complication rates of 1%-40% for this procedure [1,2,3,8,9,11,12,13,14,15,16,17,18,19,22], whereas we had a relatively lower 9.61% of complications. This large difference can be explained by the use of various techniques and approaches and the level of experience of the surgeon. In our study, 91 patients (87.5%) were operated on using a transperitoneal approach and 13 cases (12.5%) by an anterior paramedian retroperitoneal approach. We have more experience with the transperitoneal approach than the retroperitoneal approach. We believe that the retroperitoneal approach does not provide the opportunity for symmetry, as there is no straight axis of vision, and the iliac artery and iliac vein (at left because this approach is usually performed by the left side) must be retracted medially. We operated on four patients (3.86%) due to complications (Tables 1, 4). These complications included wound dehiscence, retroperitoneal hematoma, abdominal wall hematoma, and a prosthesis dislocation.
One of the most important complications in the literature is major vessel injury with an incidence of 1.9%-2.9% [5,6]. We had one retroperitoneal hematoma (0.96%). The incidence of retrograde ejaculation is 0%-4.1% in the literature. We had two cases (1.92%).
Our results following artificial total disc replacement were promising, particularly in comparison with posterior fusion results. In the latter cases, patients suffered postoperative back pain for various reasons. A meta-analysis of artificial total disc replacement vs. fusion for lumbar degenerative disc diseases performed by Yajun et al. [20] showed that total disc arthroplasty provides for slightly better functioning and back pain status and significantly greater patient satisfaction. The follow-up was 2 years in that meta-analysis. Another study performed in South Korea [8] with a 5-year follow up showed 88% satisfied or somewhat satisfied patients. Our study produced similar results with 86.54% satisfied and somewhat satisfied patients at 6 weeks and 87.5% satisfied at 12 weeks. Our average follow-up was 20 months (range, 3-38 months), which was relatively short but we noticed that the most important improvement occurs in the first 6 weeks and the evolution becomes slower and more discrete as time passes. According to the meta-analysis by Yajun et al. [20], ODI and VAS scores are typically lower than our results (on average 2 and 10, respectively).
References
1. Aoki Y, Ohtori S, Ino H, et al. Disc inflammation potentially promotes axonal regeneration of dorsal root ganglion neurons innervating lumbar intervertebral disc in rats. Spine (Phila Pa 1976) 2004;29:2621–2626. PMID: 15564910.


2. Awe OO, Maltenfort MG, Prasad S, Harrop JS, Ratliff JK. Impact of total disc arthroplasty on the surgical management of lumbar degenerative disc disease: Analysis of the Nationwide Inpatient Sample from 2000 to 2008. Surg Neurol Int 2011;2:139PMID: 22059134.



3. Bertagnoli R, Kumar S. Indications for full prosthetic disc arthroplasty: a correlation of clinical outcome against a variety of indications. Eur Spine J 2002;11(Suppl 2): S131–S136. PMID: 12384734.



4. Bertagnoli R, Yue JJ, Shah RV, et al. The treatment of disabling single-level lumbar discogenic low back pain with total disc arthroplasty utilizing the Prodisc prosthesis: a prospective study with 2-year minimum follow-up. Spine (Phila Pa 1976) 2005;30:2230–2236. PMID: 16205353.


5. Burke JG, Watson RW, McCormack D, Dowling FE, Walsh MG, Fitzpatrick JM. Intervertebral discs which cause low back pain secrete high levels of proinflammatory mediators. J Bone Joint Surg Br 2002;84:196–201. PMID: 11924650.


6. Cunningham BW, Gordon JD, Dmitriev AE, Hu N, McAfee PC. Biomechanical evaluation of total disc replacement arthroplasty: an in vitro human cadaveric model. Spine (Phila Pa 1976) 2003;28:S110–S117. PMID: 14560182.


7. Edgard-Rosa G, Geneste G, Negre G, Marnay T. Midline anterior approach from the right side to the lumbar spine for interbody fusion and total disc replacement: a new mobilization technique of the vena cava. Spine (Phila Pa 1976) 2012;37:E562–E569. PMID: 22517482.


8. Fantini GA, Pappou IP, Girardi FP, Sandhu HS, Cammisa FP Jr. Major vascular injury during anterior lumbar spinal surgery: incidence, risk factors, and management. Spine (Phila Pa 1976) 2007;32:2751–2758. PMID: 18007256.


9. Griffith SL, Shelokov AP, Buttner-Janz K, LeMaire JP, Zeegers WS. A multicenter retrospective study of the clinical results of the LINK SB Charite intervertebral prosthesis. The initial European experience. Spine (Phila Pa 1976) 1994;19:1842–1849. PMID: 7973983.


10. Hamdan AD, Malek JY, Schermerhorn ML, Aulivola B, Blattman SB, Pomposelli FB Jr. Vascular injury during anterior exposure of the spine. J Vasc Surg 2008;48:650–654. PMID: 18585888.


11. Hochschuler SH, Ohnmeiss DD, Guyer RD, Blumenthal SL. Artificial disc: preliminary results of a prospective study in the United States. Eur Spine J 2002;11(Suppl 2): S106–S110. PMID: 12384730.



12. Katsimihas M, Bailey CS, Issa K, et al. Prospective clinical and radiographic results of CHARITE III artificial total disc arthroplasty at 2- to 7-year follow-up: a Canadian experience. Can J Surg 2010;53:408–4145. PMID: 21092434.


13. Markwalder TM, Wenger M, Marbacher S. A 6.5-year follow-up of 14 patients who underwent ProDisc total disc arthroplasty for combined long-standing degenerative lumbar disc disease and recent disc herniation. J Clin Neurosci 2011;18:1677–1681. PMID: 22099076.


14. Park CK, Ryu KS, Lee KY, Lee HJ. Clinical outcome of lumbar total disc replacement using ProDisc-L in degenerative disc disease: minimum 5-year followup results at a single institute. Spine (Phila Pa 1976) 2012;37:672–677. PMID: 21857395.


15. Rundell SA, Day JS, Isaza J, Guillory S, Kurtz SM. Lumbar total disc replacement impingement sensitivity to disc height distraction, spinal sagittal orientation, implant position, and implant lordosis. Spine (Phila Pa 1976) 2012;37:E590–E598. PMID: 22146286.


16. Sasani M, Oktenoglu T, Tuncay K, Canbulat N, Carilli S, Ozer FA. Total disc replacement in the treatment of lumbar discogenic pain with disc herniation: a prospective clinical study. Turk Neurosurg 2009;19:127–134. PMID: 19431121.

17. Scott-Young MN, Lee MJ, Nielsen DE, Magno CL, Kimlin KR, Mitchell EO. Clinical and radiological Mid-Term outcomes of lumbar single-level total disc replacement. Spine (Phila Pa 1976) 2011 9 08 [Epub]. http://dx/doi/org/10.1097/BRS.0b013e3182345aa2

18. Siepe CJ, Mayer HM, Heinz-Leisenheimer M, Korge A. Total lumbar disc replacement: different results for different levels. Spine (Phila Pa 1976) 2007;32:782–790. PMID: 17414914.


19. Vicars R, Prokopovich P, Brown TD, et al. The effect of anterior-posterior shear on the wear of CHARITE total disc replacement. Spine (Phila Pa 1976) 2012;37:E528–E534. PMID: 22037530.



20. Yajun W, Yue Z, Xiuxin H, Cui C. A meta-analysis of artificial total disc replacement versus fusion for lumbar degenerative disc disease. Eur Spine J 2010;19:1250–1261. PMID: 20364392.



21. Zigler JE. Lumbar spine arthroplasty using the Pro-Disc II. Spine J 2004;4:260S–267S. PMID: 15541675.


22. Zweig T, Hemmeler C, Aghayev E, Melloh M, Etter C, Roder C. Influence of preoperative nucleus pulposus status and radiculopathy on outcomes in mono-segmental lumbar total disc replacement: results from a nationwide registry. BMC Musculoskelet Disord 2011;12:275PMID: 22136141.