 |
 |
- Search
| Asian Spine J > Volume 9(5); 2015 > Article |
Abstract
Overview of Literature
Surgical outcome of lower cervical lesions in patients undergoing hemodialysis has been reported. However, surgical outcome for upper cervical lesions in hemodialysis patients is unclear.
Methods
Upper cervical lesions in nine patients undergoing hemodialysis were surgically treated. Mean age at surgery was 61.6 years (range, 52-68 years), and the mean follow-up period was 45.4 months (range, 2-98 months). Patients had undergone hemodialysis for an average of 25.3 years (range, 16-40 years) at surgery. Seven patients with destructive spondyloarthropathy (DSA) of the upper cervical spine were treated with atlantoaxial or occipitocervical fixation. Two patients with retro-odontoid pseudotumors were treated with C1 posterior arch resection alone. Japanese Orthopedic Association (JOA) scores for cervical myelopathy, postoperative complications, postoperative radiography, and preoperative and postoperative occipital pain were evaluated.
Dialysis-related amyloidosis is a complication of endstage renal disease that results from the accumulation of β2-microglobulin and its deposition as amyloid fibrils in tissue. Periarticular tissue and bone are the most common sites of β2-microglobulin amyloid deposition. Dialysis-related amyloidosis is associated with carpal tunnel syndrome, pathological fractures, diffuse arthritis, and spondyloarthropathy. Since the first report of destructive spondyloarthropathy (DSA) [1], spine lesions have been well recognized in hemodialysis patients. The cervical spine is the most common site for hemodialysis-related lesions, and cervical DSA severely restricts the activities of daily living for hemodialysis patients. Several reports have described the surgical outcome and long-term follow-up results for hemodialysis patients with lower cervical lesions [23456]. Other reports have described upper cervical lesions in patients receiving long-term hemodialysis [78910111213141516]. Upper cervical lesions include periodontoid pseudotumor and atlantoaxial or occipitoatlantal DSA. Periodontoid pseudotumor causes myelopathy or radiculopathy, and DSA causes myelopathy or occipital pain [912141516]. Fracture of the odontoid process and associated severe instability has been reported in patients having atlantoaxial DSA [914]. As upper cervical lesions sometimes result in fatal spinal cord injury, these lesions demand special attention [8]. Only a few reports have addressed the surgical treatment of hemodialysis-related upper cervical lesions [11141516]. For pseudotumor cases, laminectomy and tumor resection have been reported [1617]. For DSA cases, Brooks posterior fusion and a combined Magerl and Brooks procedure have been reported [1516]. However, the details of postoperative outcome remain unclear.
Here, we report the surgical outcome for nine cases of hemodialysis-related upper cervical lesions.
This study was conducted in nine hemodialysis patients (five men and four women) who underwent surgery for upper cervical lesion at our hospital between 1996 and 2013. Odontoid fractures with a clear history of trauma or rheumatoid arthritis (i.e., atlantoaxial subluxation and vertical subluxation) were excluded. The mean age at surgery was 61.6 years (range, 52-68 years). The mean follow-up period was 45.4 months (range, 2-98 months). One patient was lost to follow-up two months after surgery. The patients had undergone hemodialysis for an average of 25.3 years (range, 16-40 years) at surgery. Two patients had periodontoid pseudotumor with severe myelopathy. Their radiography showed no DSA changes in the upper cervical spine. Four patients had severe myelopathy and occipital pain due to atlantoaxial DSA. One of these patients had an odontoid fracture due to erosion of the odontoid process. Three patients had severe myelopathy and occipital pain due to DSA of both occipitoatlantal and atlantoaxial joints. We performed C1 posterior arch resection for the two pseudotumor cases. A combined Magerl and Brooks procedure was performed for the atlantoaxial DSA cases. Occiput (Oc)-C5 fixation was performed for the C1-C5 DSA case. Oc-C fixation was performed for the Oc-C DSA cases. C3-C7 laminoplasty was performed if simultaneous spinal canal stenosis was seen in the lower cervical spine (Table 1).
Preoperative and postoperative neurological status was evaluated with the Japanese Orthopedics Association (JOA) score for cervical myelopathy [17]. Although the maximum score was 17 points, three points were deducted because of the difficulty in evaluating bladder function for patients undergoing hemodialysis, resulting in a maximum score of 14 points. Lateral extension-flexion radiographs were obtained to determine fusion status and the presence of adjacent segment degeneration. Perioperative complications were also investigated. All patients were fully informed that their data would be submitted for publication.
The mean preoperative and postoperative JOA score were 3.7 points (range, 0-14 points) and 8.1 points (range, 3-14 points), respectively, indicating an improvement of 4.4 points. The mean JOA score at the final follow-up was 6.3 points (range, 3-11 points). Since case 4 was operated on for odontoid fracture due to DSA without myelopathy, preoperative and postoperative JOA scores were both 14 points. No patient showed lower cranial nerve impairment. Seven patients with DSA had severe preoperative occipital pain that disappeared postoperatively. Postoperative radiography showed solid bone union in five patients who had fusion surgery. In two patients, bone union was not confirmed because one patient died two months after surgery. The other patient was lost to follow-up. The two periodontoid pseudotumor patients who had C1 posterior arch resection did not show any instability on radiography at 89 months and 67 months after surgery. One patient (case 4) had reoperation due to the progression of C5-C6 DSA, so C5-T1 anterior spinal fusion was performed. Other patients did not show adjacent segment disease. One patient (case 8) died from panperitonitis two months after surgery. No postoperative surgical site infections were noted.
The patient was a 63-year-old woman who had undergone hemodialysis for 35 years. She visited our hospital due to gait disturbance and left occipital neck pain. JOA score was 1 point on the first visit. Lateral extension-flexion radiographs showed severe instability at atlantoaxial joints (Fig. 1). Computed tomography (CT) showed mild destruction of right occipitoatlantal joint (Fig. 2A), mild destruction of left occipitoatlantal joint, and severe destruction of left atlantoaxial joint (Fig. 2B). CT also showed severe erosive change of the odontoid process (Fig. 2C). Magnetic resonance imaging (MRI) showed a high T2 signal in the spinal cord at the C1 level without severe spinal canal stenosis, indicating spinal cord injury due to instability of atlantoaxial joints (Fig. 3A). Spinal canal stenosis was also observed in lower cervical spine (Fig. 3B). We performed Oc-C3 fixation, C1 posterior arch resection, and C3-C7 laminoplasty (Fig. 4). The left occipital pain disappeared after surgery. The postoperative JOA score was 7 points one year after surgery.
Surgical outcome for upper cervical lesions in hemodialysis patients was investigated. We treated the periodontoid pseudotumor cases without DSA changes in radiography with C1 posterior arch resection. Several types of surgical treatment for periodontoid pseudotumor in hemodialysis patients have previously been reported [71516]. C1 posterior arch resection and tumor resection are possible for pseudotumors located on the posterolateral side of the odontoid process [1516]. Moonis et al. [18] treated a pseudotumor case located on the odontoid process with transoral resection and posterior fusion. However, this procedure is too invasive to perform in long-term hemodialysis patients. We therefore performed a previously described C1 posterior arch resection alone [7]. Although this approach might have caused instability due to DSA, our long-term follow-up data showed satisfactory results without instability on radiography. Our results showed that myelopathy caused by periodontoid pseudotumor might be treated with C1 posterior arch resection alone.
We experienced seven cases of upper cervical DSA. A combined Magerl and Brooks procedure was performed for three patients with atlantoaxial DSA. If the patient had spinal canal stenosis due to simultaneous periodontoid pseudotumor, C1 laminoplasty was performed with atlantoaxial fixation [11]. Several reports concerning atlantoaxial DSA have been published [111214]. Gerster et al. [9] reported that 38 percent of patients undergoing long-term hemodialysis showed upper cervical lesions, including cystic radiolucency in the C1 lateral mass, dens, and body of C2 on radiography. They also reported that radiography showed occipitoatlantal joint change in two of 23 patients undergoing long-term hemodialysis [9]. It was also reported that slight instability at the occipitoatlantal joint was observed in two of five patients who had atlantoaxial DSA [12]. We experienced occipitoatlantal DSA in four cases. In our cases, all patients with occipitoatlantal DSA had atlantoaxial DSA. In these cases, Oc-C fixation was required. Since patients with myelopathy due to upper cervical DSA sometimes suffer fatal spinal cord injury with minor trauma, surgery is required for these patients [8]. Odontoid fracture due to DSA causes especially severe instability and has a higher risk of spinal cord injury; thus fixation surgery is mandatory. There have been several reports describing surgical treatments for the upper cervical DSA [91214]. However, no reports of the precise surgical procedures and long-term follow-up data have been published. In this study, three cases were treated with the Magerl and Brooks procedures, and four cases were treated with Oc-C fixation. Although reoperation was done due to progression of lower cervical DSA in one patient (case 4), all patients who were able to follow-up had solid bone union and did not show any problems in the upper cervical spine during follow-up.
The average neurological recovery in our series, as measured by the JOA score, was 4.4 points. This result is similar to the findings of reports on lower cervical lesions in patients undergoing hemodialysis [25], indicating that neurological recovery after surgical treatment in hemodialysis-related upper cervical lesions can be satisfactory [25]. We also showed the long-term follow-up data of five patients. Although the JOA score gradually decreased because of factors unrelated to the cervical spine, we did not experience a case of reoperation for the upper cervical spine.
Conflict of Interest
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
1. Kuntz D, Naveau B, Bardin T, Drueke T, Treves R, Dryll A. Destructive spondylarthropathy in hemodialyzed patients: a new syndrome. Arthritis Rheum 1984;27:369–375. PMID: 6712753.


2. Abumi K, Ito M, Kaneda K. Surgical treatment of cervical destructive spondyloarthropathy (DSA). Spine (Phila Pa 1976) 2000;25:2899–2905. PMID: 11074677.


3. Han IH, Kim KS, Park HC, et al. Spinal surgery in patients with end-stage renal disease undergoing hemodialysis therapy. Spine (Phila Pa 1976) 2009;34:1990–1994. PMID: 19680107.


4. Spinos P, Matzaroglou C, Partheni M, Deli A, Karanikolas M, Konstantinou D. Surgical management of cervical spondyloarthropathy in hemodialysis patients. Open Orthop J 2010;4:39–43. PMID: 20148095.



5. Sudo H, Ito M, Abumi K, et al. Long-term follow up of surgical outcomes in patients with cervical disorders undergoing hemodialysis. J Neurosurg Spine 2006;5:313–319. PMID: 17048767.


6. Yuzawa Y, Kamimura M, Nakagawa H, et al. Surgical treatment with instrumentation for severely destructive spondyloarthropathy of cervical spine. J Spinal Disord Tech 2005;18:23–28. PMID: 15687848.


7. Amoroso E, Vitale C, Silvestro A. Spinal-cord compression due to extradural amyloidosis of the cervico-occipital hinge, in a hemodialysed patient: a case report. J Neurosurg Sci 2001;45:120–124. PMID: 11533538.

8. Danesh FR, Klinkmann J, Yokoo H, Ivanovich P. Fatal cervical spondyloarthropathy in a hemodialysis patient with systemic deposition of beta2-microglobulin amyloid. Am J Kidney Dis 1999;33:563–566. PMID: 10070922.


9. Gerster JC, Carruzzo PA, Ginalski JM, Wauters JP. Cervicooccipital hinge changes during longterm hemodialysis. J Rheumatol 1989;16:1469–1473. PMID: 2689648.

10. Hsu CW, Wu MS, Leu ML. Dialysis-related cervical amyloidoma presenting with quadriplegia. Ren Fail 2001;23:135–138. PMID: 11256523.


11. Kato Y, Kanaya K, Itoh T. Destructive spondyloarthropathy of the atlantoaxial joint with severe spinal cord compression in long-term hemodialysis patients. J Orthop Sci 2006;11:644–650. PMID: 17139476.


12. Kroner G, Stabler A, Seiderer M, Moran JE, Gurland HJ. Beta 2 microglobulin-related amyloidosis causing atlantoaxial spondylarthropathy with spinal-cord compression in haemodialysis patients: detection by MRI. Nephrol Dial Transplant 1991;6(Suppl 2): 91–95. PMID: 1866078.

13. Mandrioli J, Zini A, Cavalleri F, Vandelli L, Nichelli P, Colombo A. Isolated Hypoglossal nerve palsy due to amyloid cervical arthropathy in long term hemodialysis. J Neurol 2006;253:1229–1231. PMID: 16609805.


14. Mikawa Y, Yamaoka T, Watanabe R. Compression of the spinal cord due to destructive spondyloarthropathy of the atlanto-axial joints. J Bone Joint Surg Am 1996;78:1911–1914. PMID: 8986670.


15. Takeshima Y, Kotsugi M, Park YS, Nakase H. Hemodialysis-related upper cervical extradural amyloidoma presenting with intractable radiculopathy. Eur Spine J 2012;21(Suppl 4): S463–S466. PMID: 22116311.


16. Vignes JR, Eimer S, Dupuy R, Donois E, Liguoro D. beta(2)-Microglobulin amyloidosis caused spinal cord compression in a long-term haemodialysis patient. Spinal Cord 2007;45:322–326. PMID: 16926830.


17. Ogawa Y, Chiba K, Matsumoto M, et al. Long-term results after expansive open-door laminoplasty for the segmental-type of ossification of the posterior longitudinal ligament of the cervical spine: a comparison with nonsegmental-type lesions. J Neurosurg Spine 2005;3:198–204. PMID: 16235702.


18. Moonis G, Savolaine ER, Anvar SA, Khan A. MRI findings of isolated beta-2 microglobulin amyloidosis presenting as a cervical spine mass: case report and review of literature. Clin Imaging 1999;23:11–14. PMID: 10332591.


Fig. 1
Preoperative extension (A) and flexion (B) lateral radiographs showing severe instability of atlantoaxial joints.
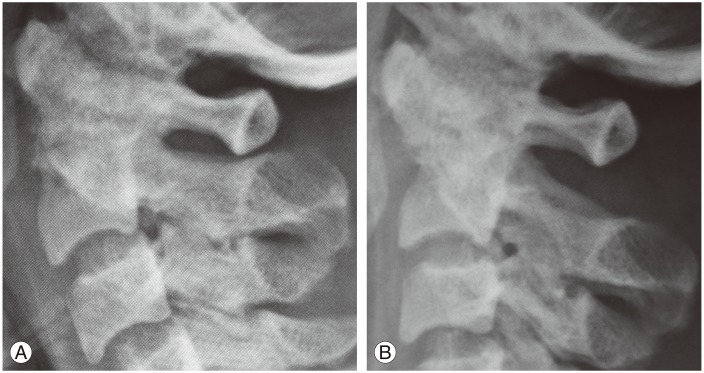
Fig. 2
Sagittal computed tomography (CT) showing mild destruction of right Oc-C1 joint (A) and mild destruction of left Oc-C1 joint and severe destruction of left atlantoaxial joint (B). (C) Sagittal CT showing erosive change of the odontoid process. Oc, occiput.
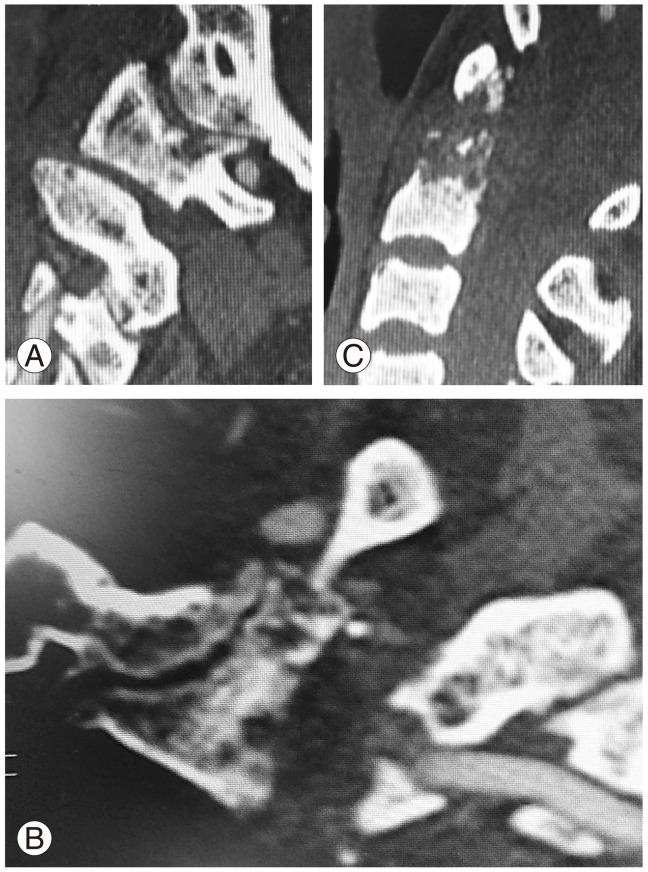
Fig. 3
Magnetic resonance imaging showing T2 high signal in spinal cord at C1 level without sever spinal canal stenosis, indicating spinal cord injury due to instability of atlantoaxial joints (arrow) (A). Spinal canal stenosis observed in lower cervical spine (B).
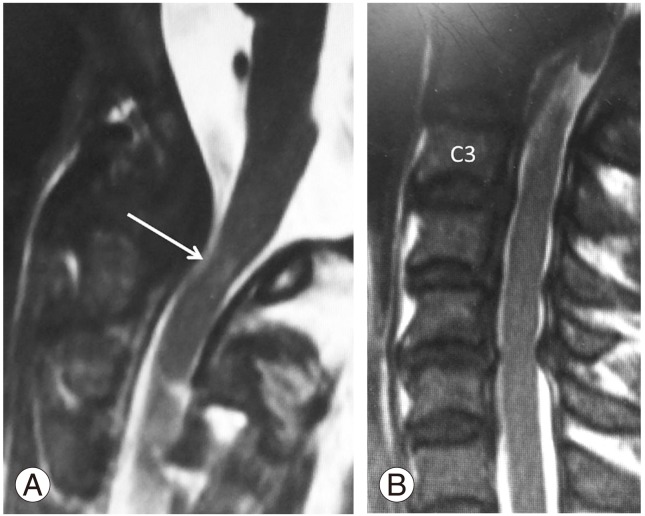
Fig. 4
Postoperative lateral radiography after surgery. Oc-C3 fixation, C1 posterior arch resection, and C3-C7 laminoplasty was performed. Oc, occiput.
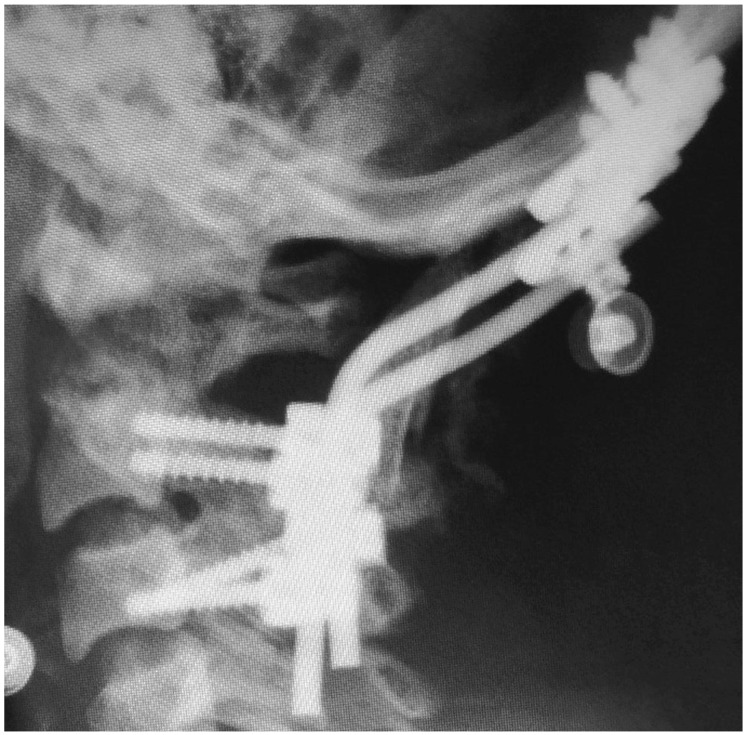
Table 1
Summary of patients data
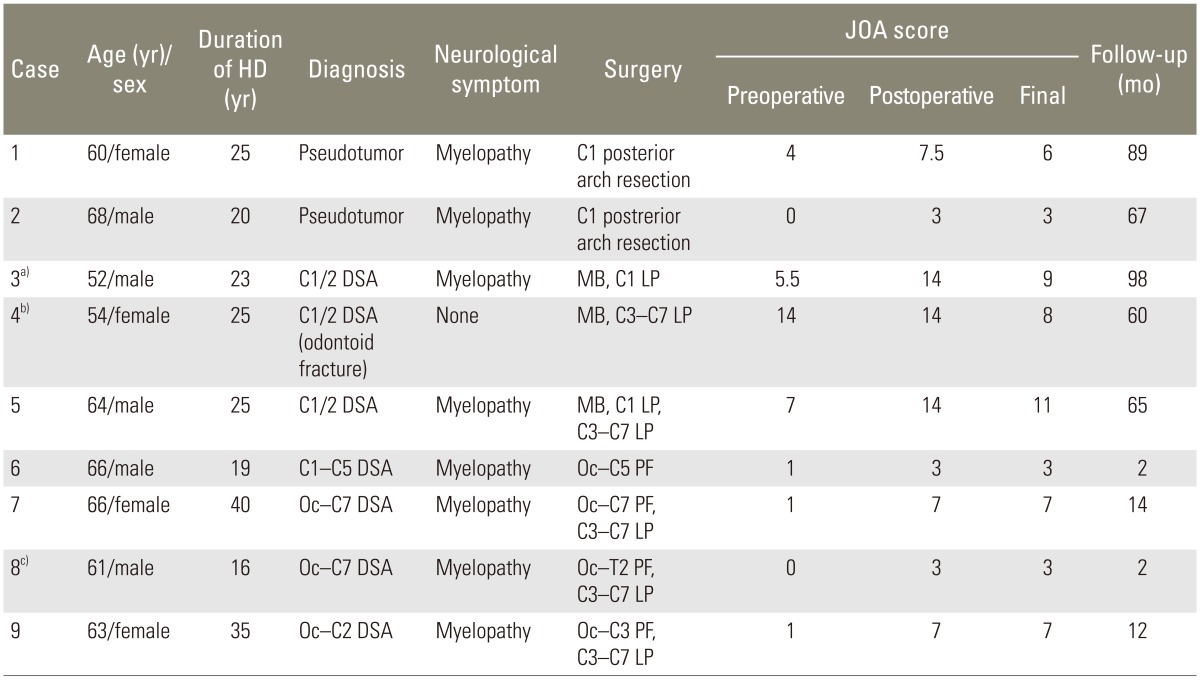
HD, hemodialysis; JOA, Japanese Orthopedic Association; DSA, destructive spondyloarthropathy; MB, Magerl and Brooks procedure; LP, laminoplasty; Oc, occiput; PF, posterior fusion.
a)C3-C7 LP was performed 9 years after primary surgery; b)C5/6 DSA was treated with anterior spinal fusion; c)Athetoid cerebral palsy died from panperitonitis.
- TOOLS
-
METRICS

- Related articles in ASJ
-
Are We Missing Osteoporosis-Related Vertebral Fractures in Men?2011 June;5(2)





