Effect of Different Types of Upper Instrumented Vertebrae Instruments on Proximal Junctional Kyphosis Following Adult Spinal Deformity Surgery: Pedicle Screw versus Transverse Process Hook
Article information
Abstract
Study Design
Retrospective comparative study.
Purpose
To compare the incidence of proximal junctional kyphosis (PJK) between transverse process hooks (TPHs) and pedicle screws (PSs) at the upper instrumented vertebrae (UIV) following adult spinal deformity (ASD) surgery.
Overview of Literature
The choice of UIV implant type may be important for avoiding PJK; however, few comparative clinical studies have evaluated the incidence of PJK according to the type of UIV implant used in ASD surgery.
Methods
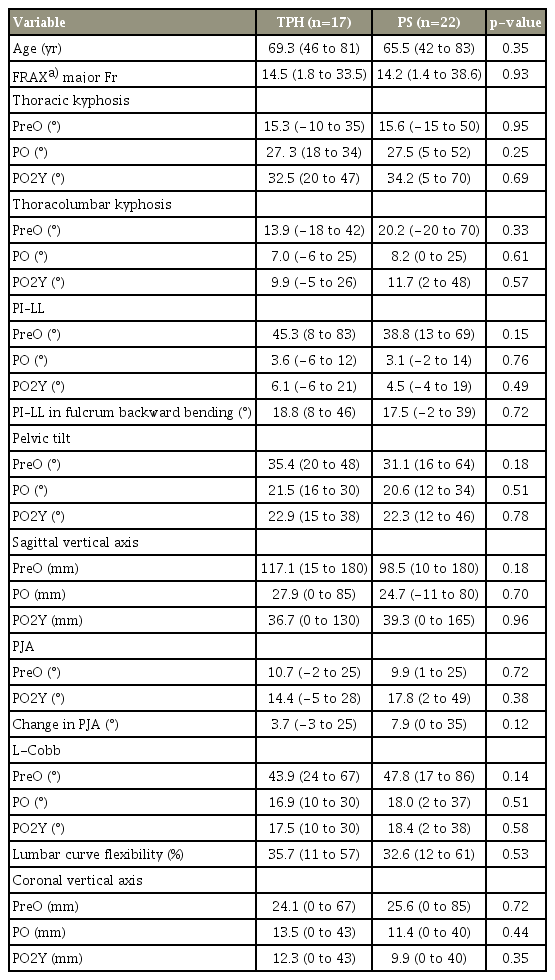
We retrospectively reviewed 39 consecutive patients with ASD (mean age, 67 years; mean follow-up period, 41 months) who underwent corrective surgery between 2009 and 2013. TPH was used in 17 patients and PS in 22 patients. PJK was defined as the presence of a UIV or UIV±1 fracture, or a change in the proximal junctional angle (PJA) of >20°. Data of patients with TPH and PS were compared.
Results
The TPH group had a PJK incidence of 17.6% compared with 27.3% in the PS group (p =0.47). In the TPH group, PJK was a result of UIV fracture in one patient, UIV−1 fracture in one patient, and ligamentous failure in one patient. In the PS group, six patients developed PJK because of UIV fracture. No differences in radiographic parameters were found between the two groups. After analyzing the PJA data in the patients with PJK, the changes in PJA were significantly higher in the PS group than in the TPH group (19.0°/5.0°, p =0.04).
Conclusions
Our results show that using TPH as a UIV implant may not prevent PJK; however, using TPH as the UIV anchor may prevent vertebral collapse if cases of UIV fracture. The increased risk of UIV fracture collapse in the PS group may be a result of a higher mechanical load on UIV when using PS.
Introduction
Surgical intervention for an adult spinal deformity (ASD) is mainly aimed at correcting the spinopelvic malalignment and subsequently restoring the global sagittal balance [1]. To achieve spinal balance, surgical long-segment fixation to the pelvis is often necessary [2,3]. However, long-segment spinal fixation, particularly to the pelvis, is associated with the potential risks of postoperative complications including pseudoarthrosis [4], implant failure [5,6], and adjacent problems [7,8]. Proximal junctional kyphosis (PJK) is an important concern with ASD surgery [7,8]. PJK following ASD surgery is reported in approximately 30% of cases [8] and may result in poor clinical outcomes [9] or neurological problems [10,11]. Several reports found that possible risk factors were long and rigid fusion constructs and pedicle screw (PS) instrumentation techniques [11,12], upper instrumented vertebrae (UIV) [13,14], integrity of the posterior soft-tissue tension band [15,16], magnitude of the correction in the sagittal plane [17,18], combined anteroposterior (AP) spinal surgery [19], and osteoporosis [20].
Some previous reports that targeted adolescent idiopathic scoliosis described the possibility of the implant type at UIV in spinal deformity surgery as a factor in the development of PJK [21,22]. To avoid PJK, it is thought that the type of UIV implant may be important; however, few comparative clinical studies have evaluated the incidence of PJK according to the type of UIV implant in ASD surgery. The aim of this study is to compare the incidence of PJK and changes in the proximal junctional angle (PJA) following ASD surgery using two types of UIV implants: transverse process hooks (TPHs) and PSs.
Materials and Methods
The medical records of 39 consecutive patients (two men and 37 women) with ASD who underwent corrective surgery by a single surgeon at a single institution and were followed up for at least 2 years were retrospectively reviewed. The mean age at the time of surgery was 67.4 years (range, 42–83 years), and the average follow-up period was 42.9 months (range, 24–91 months). All patients complained of multiple years of lower back pain that was not alleviated with conservative treatment. T9 UIV was selected in 13 patients and T10 UIV in 26 patients. Spinopelvic fusion was performed in all patients using iliac or sacral-alar-iliac screws. PSs as UIV implants were used in the first 22 patients until 2013, and TPHs were used in the next 17 patients from 2013 onward. Sublaminar taping with two polyethylene tapes at UIV was also used in all patients. Augmentation by sublaminar taping at UIV was an effective method of preventing the pull-out of spinal instruments, including TPH and PS. It also added semirigid stabilization by holding the entire lamina. Among the 39 patients, 10 patients underwent three-column osteotomy (pedicle subtraction osteotomy or vertebral column resection).
The following radiographic parameters were assessed with standing AP and lateral plain radiography immediately prior to surgery (PreO), 2 weeks after surgery (PO), and 2 years after surgery (PO2Y): degree of thoracic kyphosis (TK, T5–T12), degree of thoracolumbar kyphosis (TLK, T10–L2), degree of lumbar lordosis (LL, T12– S1), pelvic tilt (PT), pelvic incidence (PI), sagittal vertical axis (SVA), Cobb angle of the lumbar curve (L-curve), and coronal vertical axis. Each patient’s curve flexibility was also evaluated with side bending (L-curve flexibility) films in the coronal plane and with fulcrum backward bending (FBB) films in the sagittal plane [23]. PJA was measured between the caudal endplate of UIV to the cephalad endplate located two vertebrae proximal, as previously described by Glattes et al. [24].
PJK was defined by two criteria: (1) UIV, UIV+1, and UIV−1 vertebral fracture, and (2) change in PJA (dPJA) of at least 20° compared with the preoperative measurement. Using all data, two comparative analyses were performed: (1) between PJK and non-PJK groups and (2) between TPH and PS groups.
Clinical outcomes were evaluated using the Japanese editions of the Scoliosis Research Society-22 Outcomes Questionnaire (SRS-22) and the Medical Outcomes Study Questionnaire Short-Form 36 (SF-36) administered at PreO and PO2Y. All data were statistically analyzed using analysis of variance, Mann–Whitney U-test, or paired or unpaired t-test as appropriate (JMP ver. 11.0; SAS, Cary, NC, USA). For all tests, p<0.05 was considered statistically significant.
This study was approved by the ethics committee of Osaka City General Hospital (approval no., 1305011).
Results
1. Clinical outcomes
The mean total SRS-22 scores were 2.5±0.7 at PreO, which significantly improved to 3.8±0.5 at PO2Y (p<0.0001). The mean overall patient satisfaction scores were 4.1 (range, 2.5–5.0), indicating a good surgical outcome. All domains of SRS-22 significantly improved at PO2Y (Table 1). Table 2 shows health-related quality of life data measured by SF-36. All domains of SF-36 significantly improved at PO2Y (p<0.05).
2. Radiographic evaluation
The mean values of the preoperative radiographic parameters in the sagittal plane were as follows: TK, 15.4°; TLK, 17.5°; LL, 11.5°; PT, 32.9°; PI, 52.3°; and SVA, 104.6 mm. The preoperative mean PI–LL was 40.4°. PI–LL in FBB films was 18.2°. PI–LL was reduced to 3.3° at PO and increased to 5.2° at PO2Y. PT improved was to 20.9° at PO and remained stable at PO2Y. SVA also improved to 26.1 mm at PO, but increased to 39.0 mm at PO2Y, although the change was not significant (Table 3).
PJK occurred in nine patients, three in the TPH group and six in the PS group. The incidence of PJK in the two groups was not significantly different (p=0.47). In the TPH group, PJK was caused by UIV fracture in one patient, UIV−1 fracture in one patient, and ligamentous failure resulting in dPJA >20° in one patient. In six patients in the PS group (66.7%), PJK was caused by UIV fracture that occurred within 4 weeks after surgery.
1) PJK group versus non-PJK group
The mean age at surgery in the PJK group was significantly more than that in the non-PJK group (73.5 versus 65.5 years.). Additionally, the risk of a major fracture, according to the fracture risk assessment tool (FRAX), was significantly higher in the PJK group than in the non-PJK group (22.4 versus 11.6). Comparative analysis of radiographic parameters indicated that there was a greater tendency for PO SVA, PO2Y TK, and PO2Y TLK in the PJK group than in the non-PJK group. PJA at PO2Y in the PJK group was significantly larger than that in the non-PJK group (p=0.01). Table 4 summarizes these analyses. All domains of the SRS-22 scores in both the groups are shown in Table 5, and all domains of SF-36 are shown in Table 6. No significant differences were noted between the two groups.
2) TPH versus PS group
The incidence of PJK in the TPH group was statistically comparable with that in the PS group, as already described. No significant differences were noted in any of the data including age at surgery, FRAX, and radiographic parameters (Table 7). However, the dPJA of patients with PJK was significantly larger in the PS group than in the TPH group (Table 8).
Discussion
PJK is a recognized complication following ASD surgery and has recently attracted increased attention [7-11,16-18]. PJK had been defined as a change in PJA of >10° [24]. However, some studies have indicated that these changes do not affect clinical outcomes. Bridwell et al. [25] evaluated PJK following ASD surgery using PJA >20° and found that the clinical outcomes were worse in patients with PJK. Yagi et al. [10,18] classified PJK into three types: ligamentous failure, bone failure, and implant/bone interface failure. Therefore, in the present study, changes in PJA of >20° and the presence of UIV or UIV±1 fracture were used to define PJK. The incidence of PJK in the current study was 24% (9/37), and eight of the nine PJK patients showed bone failure, including UIV fracture and UIV−1 fracture. Six UIV fractures occurred within 4 weeks after surgery. Several previous reports have cited PJK incidence ranging from 20% to 40% [8]. Yagi et al. [10] reported that 76% of PJK occurred within 3 months after surgery [10], and Maruo et al. [17] reported that 62% of PJK occurred within 8 weeks after surgery [17]. They also stated that UIV fracture was the most common mechanism of PJK. Our results approximately matched their results. Therefore, we believe that UIV fracture is the most common etiology of PJK and that it occurs relatively early after ASD surgery.
Several risk factors of PJK, including older age [11,17,18], spinopelvic fusion [6,18,26], magnitude of sagittal imbalance [10], magnitude of TK [17], and a greater PI–LL change [17] have been previously reported. Recently, Scheer et al. [26] of the Invasive Species Specialist Group reported a computer-based preoperative predictive model for proximal junctional failure (PJF). The seven strongest predictors of PJF are age, lowest instrumented vertebra, preoperative SVA, UIV implant type, UIV, preoperative PT, and preoperative PI–LL. Our comparative analysis indicates that older age (p=0.01) and fracture risk defined by FRAX (p=0.04) are possible risk factors of PJK. Preoperative SVA (p=0.11) shows some tendency in that regard.
According to previous reports, the impact of PJK on quality of life is variable [9,18]. However, the severity of PJK may vary, and PJF may result in compromised structural integrity and neurological deficit, with severe cases potentially needing revision surgery [10,11]. Unlike PJK, patients with PJF have a worse clinical course. The current comparative analysis of health-related quality of life between PJK and non-PJK shows that PJK has no significant impact on surgical outcomes. It may be because none of the patients had a neurological deficit and radiographic measurements improved in all patients with PJK.
Preventing PJK in patients who undergo ASD surgery is one of the most important issues for successful correction surgery and improvement in the postoperative quality of life [26]. As described, PJK is a multifactorial phenomenon that may occur after long-segment fixation surgery. Therefore, there is no definitive solution for preventing PJK, although there are some prophylactic procedures. Some reported strategies are the treatment of osteoporosis with teriparatide [20]; surgical intervention including cement augmentation [13], UIV anchors [21,22], and percutaneous screws [27]; transitional rods [28]; UIV selection [13-15]; and preservation of the posterior ligamentous complex [16].
Among these strategies, we were particularly interested in the types of UIV anchors. The comparative analysis of TPH and PS as UIV anchors indicates no significant difference in the incidence of PJK. However, changes in PJA in patients with PJK were significantly more common in the PS group (Fig. 1) than in the TPH group (Fig. 2). The magnitude of vertebral body collapse following vertebral fracture was more severe in the PS group. Watanabe at al. [11] reported proximal junctional vertebral fracture following ASD surgery that used PS constructs. Additionally, a comparative study of adolescent idiopathic scoliosis surgery indicated significant advantages for TPH over PS fixation to prevent PJK [21,22]. In a biomechanical study, TPH fixation produced a significant reduction of flexion movement compared to PS fixation [15]. Our results were consistent with these reports. We speculate that the mechanism of PJK using PS as the UIV anchor may be as follows. In the patient with osteoporosis, PS as the UIV anchor may directly damage the vertebral body, allowing subsequent vertebral fracture. If a fracture occurs, PS may break the upper endplate and penetrate the disc space, leading to severe collapse of UIV. Conversely, TPH as the UIV anchor may be a better choice because it provides a soft landing at the transitional segment of the long-segment fixation construct [29]. There are some limitations to our study. Our study included a small number of cases and had a short-term follow-up period, and this was not a biomechanical study. Future work should involve a longer follow-up period and a larger sample size.
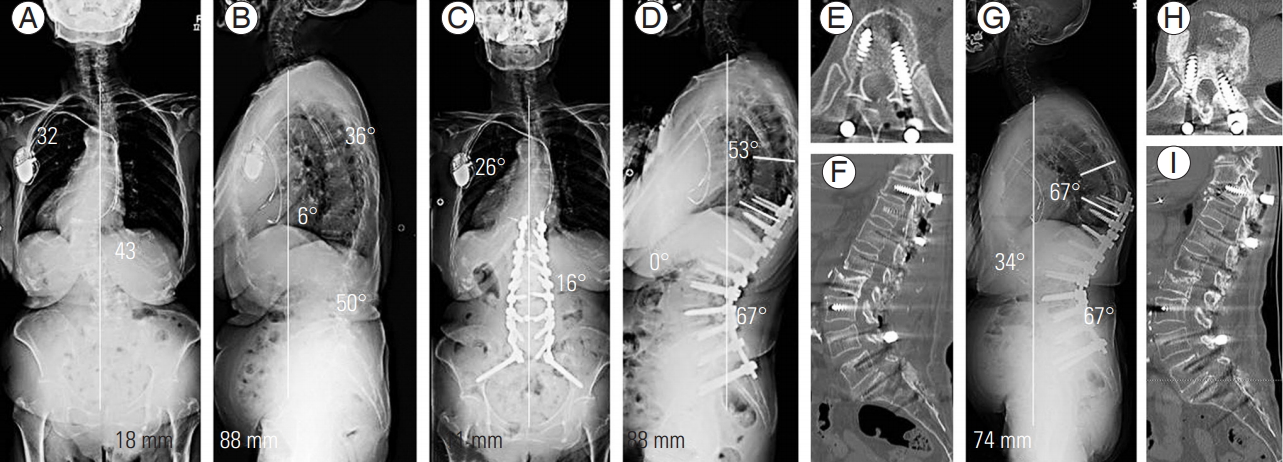
Case presentation: an 83-year-old woman who underwent T10 pelvic posterior corrective surgery using PS as UIV anchor. (A, B) Preoperative radiographs. AP radiograph shows that the Cobb angle of the lumbar curve and the compensatory thoracic curve were 26° and 43°, respectively. Lateral radiograph shows TK of 36°, TLK of 6°, LL of 50°, PT of 23°, and PI of 63°. PI–LL was 13°. SVA shifted 88 mm anteriorly. (C, D) Radiographs 2 weeks after surgery. AP radiograph shows a Cobb angle of the compensatory thoracic and lumbar spine reduced to 26° and 16°, respectively. Lateral radiograph shows TK of 53°, TLK of 0°, LL of 67°, and PT of 22°. PI–LL was reduced to −4°, and SVA was improved to −11 mm. (E, F) CT images 1 week after surgery showing no apparent fracture at UIV. However, UIV fracture occurred 1 month after surgery with progression of segmental kyphosis. (G) Radiograph 3 years after surgery. Lateral radiograph shows TK of 67°, TLK of 34°, LL of 67°, PT of 22°, and SVA deteriorated to 74 mm. Proximal junctional angle changed from 12° before surgery to 34° at 3 years after surgery. (H, I) CT images show vertebral collapse of UIV and PS penetration of the disc space. PS, pedicle screw; UIV, upper instrumented vertebrae; AP, anteroposterior; TK, thoracic kyphosis; TLK, thoracolumbar kyphosis; LL, lumbar lordosis; PT, pelvic tilt; PI, pelvic incidence; SVA, sagittal vertical axis; CT, computed tomography.
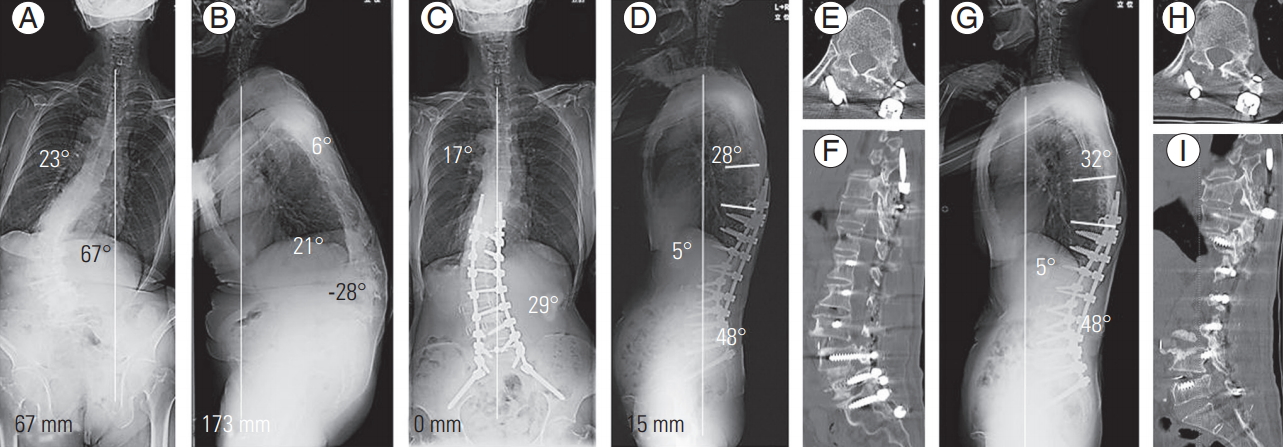
Case presentation: A 75-year-old woman who underwent T10 pelvic lateral interbody fusion and posterior corrective surgery using transverse process hook as UIV anchor. (A, B) Preoperative radiographs. AP radiograph shows that the Cobb angle of the lumbar curve and the compensatory thoracic curve were 23° and 67°, respectively. Lateral radiograph shows TK of 6°, TLK of 21°, LL of -28°, PT of 45°, and PI of 55°. PI–LL was 83°. SVA shifted 173 mm anteriorly. (C, D) Radiographs 2 weeks after surgery. AP radiograph shows that Cobb angle of the compensatory thoracic and lumbar spine reduced to 17° and 16°, respectively. Lateral radiograph shows TK of 28°, TLK of 6°, LL of 48°, and PT of 26°. PI–LL was reduced to 7°, and SVA improved to 15 mm. (E, F) CT images 1 week after surgery show no apparent fracture at UIV. However, UIV fracture occurred 3 weeks after surgery but without progression of segmental kyphosis. (G) Radiographs 3 years after surgery. Lateral radiograph shows TK of 32°, TLK of 6°, LL of 48°, PT of 26°, and no deterioration of SVA. Proximal junctional angle changed from 11° before surgery to 13° at 3 years after surgery. (H, I) CT images show that the vertebral collapse of UIV is acceptable and that the endplate of UIV is intact. CT, computed tomography. UIV, upper instrumented vertebrae; AP, anteroposterior; TK, thoracic kyphosis; TLK, thoracolumbar kyphosis; LL, lumbar lordosis; PT, pelvic tilt; PI, pelvic incidence; SVA, sagittal vertical axis; CT, computed tomography.
Conclusions
Our results show that using TPH as a UIV implant may not prevent PJK; however, using TPH as the UIV anchor may prevent vertebral collapse if cases of UIV fracture. In this study, the increased risk of collapse with UIV fracture in the PS group may have been the result of a higher mechanical load on UIV when using PS fixation. Further biomechanical studies should be performed to clarify our results.
Notes
No potential conflict of interest relevant to this article was reported.
Author Contributions
Matsumura A: corresponding author, conception, design, and analysis; Matsumura A, Namikawa T, Kato M, Oyama S, Ozaki T, Hori Y, Yabu A: acquisition of data; and Hidaka N, Nakamura H: critically revising the article.