Introduction
Aspergillus infections are opportunistic infections that are encountered most commonly in immunocompromised patients. They usually involve the lungs, skin, central nervous system, paranasal sinus, orbit, or bone, but may disseminate1. Aspergillus osteomyelitis is an uncommon manifestation that most frequently involves the lumbar spine2 and usually arises as a result of hematogenous transmission from another focus. Other mechanisms include direct transmission from the lung, or contamination during surgery2. The increased number of organ transplants in recent years has resulted in a remarkable increase in the incidence of immunocompromised individuals. Early diagnosis and appropriate antifungal therapy are critical because aspergillus spondylitis (AS) has a high risk of developing complications during conservative and surgical treatment. We report a case of multiple AS in a liver transplant recipient also involving the right hip joint.
Case Report
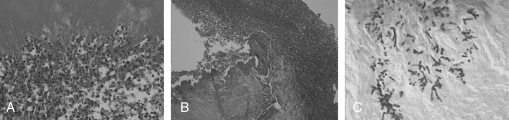
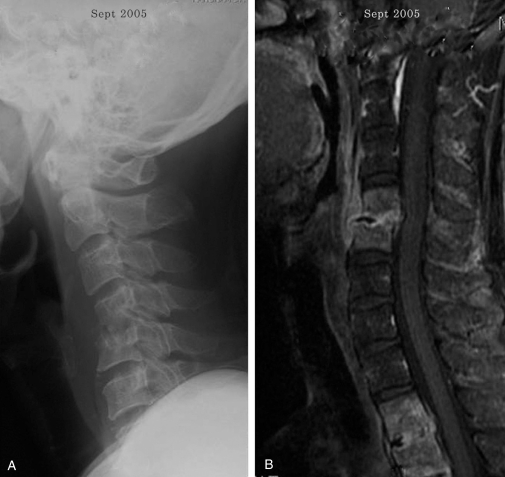
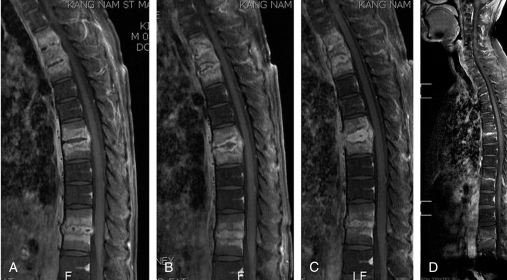
A 46-year-old man presented with unremitting low back pain and right leg weakness that had persisted for 1 month. He had previously received partial liver transplant under a diagnosis of liver cirrhosis in March 2005 but fever with an unknown origin persisted after the transplant. Suspecting sepsis, the patient was treated with multiple antibiotics, but a fungal colony was found in the left lower lung field during the antibiotics treatment. Aspergillus was confirmed in the sputum culture test. Accordingly, 60 mg of Amphotericin B was injected intravenously for two weeks but with no significant improvement. Consequently, 50 mg of a different antifungal agent, candidas (caspofungin acetate), was injected over a 2-week period, and a lobectomy was performed on the left lower lung. The patient was under immunosuppression (cyclosporine 250 mg orally), which was continued under antifungal treatment after the lobectomy. After the lobectomy, he complained of mild low back pain and consulted our department. Mild tenderness was found over the low back but there was no abnormality on the plain radiograms except for the degenerative changes in the lumbar spine. Low back pain was not significant enough to recommend a MRI, so we just recommended limited activity, non-steroidal anti-inflammatory drugs and close observation. However, the low back pain did not subside, and he again consulted our department. A physical examination revealed severe tenderness and rigidity over the lower lumbar area. Straight leg raising on the right lower extremity was restricted to 50°, and extension of the right great toe and dorsiflexion of right ankle were poor. The sensory performance of his right leg had decreased, a limited range of motion of the right hip was noted, and the Patrick test was positive. A laboratory examination showed an erythrocyte sedimentation rate (ESR) of 100 mm/hour (reference range, 0 to 15 mm/ hour), C-reactive protein (CRP) of 2.14 mg/dL (reference range, 0 to 0.3 mg/dL), white blood cell count of 5.4/mm3, and lymphocytes percent of 17.2%. The plain roentgenograms of the lumbar spine revealed rapid progressive destructive changes, narrowing of the intervertebral disc space of L3-4 and L4-5 with an erosion of the end plates of L3, L4, and L5 (Fig. 1A). MR imaging of the lumbar spine showed narrowing of the disc space at L3-4 and L4-5, and an irregular contour of the endplate at L3-4, as well as an epidural abscess from L2-3 to L4-5 (Fig. 1B). The pelvic roentgenogram showed a loss of contour at the right acetabulum and joint space narrowing of the right hip (Fig. 1C). The patient underwent anterior decompression and anterior interbody fusion with autogenous strut iliac bone for L-3-4-5, but surgical intervention was not performed for L2-3. The surgical findings did not show any pus at the anterior aspect of L3, L4, and L5, but an epidural abscess and infective granuloma were observed at the L3-4 and L4-5 intervertebral space. Gram staining and cultures of the tissue specimens were negative. A pathological examination of the biopsy specimen showed acute inflammation and necrosis with fungal hyphae (Fig. 2). The following day, there was dramatic improvement on his leg weakness, but there was still pain during hip motion. An infection specialist recommended continuing the antifungal chemotherapy with Amphotericin B. A 50 mg of Amphotericin B was injected intravenously daily over a 40 day period (accumulatively total 2 g). The laboratory examination showed an ESR of 108 mm/hour and CRP of 1.89 mg/dL after administering Amphotericin B. Two months later, the patient was readmitted because of severe neck pain and right arm weakness that had persisted for 3 weeks. After a physical observation, general tenderness was observed in the cervical spine. The axial compression test and Spurling test was positive, and decreased motor function with no sensory abnormality was observed in the right upper limb. The laboratory examination showed an ESR of 110 mm/hour and CRP of 0.83 mg/dL. Plain roentgenograms of the cervical spine revealed intervertebral disc space narrowing of C4-5 with erosion of the end plates and subluxation (Fig. 3A). MR imaging of the cervical and thoracic spine showed an epidural and paraspinal abscess at C4-5 (Fig. 3B), D2-3-4, D6-7, and D10-11 (Fig. 4A). The patient underwent anterior decompression and anterior interbody fusion with an autogenous graft bone for the treatment of cervical spondylitis. Conservative care was taken for the thoracic lesion because no neurologic deficit was observed, even though he complained of upper thoracic pain. However, a pathological examination of the biopsy specimen revealed acute inflammation with fungal hyphae. Amphotericin B was switched to itraconazole (100 mg bid per day) because the full amount of Amphotericin B had already been administrated. MR imaging of the thoracic spine taken 6 weeks after antifungal therapy with itraconazole showed a slightly regressed epidural abscess at D10-11 while epidural abscess at D2-3-4 and D6-7 had progressed slightly (Fig. 4B). Ten weeks after anti-fungal therapy, MR imaging of the thoracic spine showed a slightly regressed epidural abscess at D6-7 and no interval change at D2-3-4 and D10-11 (Fig. 4C). The patient reported mild pain at the right hip joint, and the plain roentgenograms of the hip joint revealed no interval changes compared to the previous roentgenograms. Surgery for the right hip was not considered because there was no significant pain at that time. The plain roentgenograms of the spine, performed 4 months after surgery revealed fusion at C4-5 and L3-4-5. The patient's pain was relieved significantly 8 months after anti-fungal therapy with itraconazole. MRI of the cervical and lumbar spine showed solid interbody fusion at C4-5 and L3-4-5. However, ESR and CRP were not normalized (45 mm/hour and 1.87 mg/dL) despite the 8 months administration of itraconazole. Therefore, itraconazole was switched to voriconazole (200 mg bid per day). Six months after voriconazole administration, MRI showed almost complete resolution of inflammation, and the laboratory examination resulted in an ESR of 51 mm/hour and a CRP of 0.24 mg/dL. Although ESR (51 mm/hour) did not reach the normal limits, itraconazole was not administrated further because his clinical conditions, including roentgenographic findings, had improved greatly and the CRP was normalized. The final roentgenograms showed solid interbody fusion of the cervical and lumbar spine as well as spontaneous fusion of the thoracic spine (Fig. 5A-5C). The hip roentgenograms revealed subluxation with degenerative changes of the right hip joint (Fig. 5D). The patient was rehabilitated and is doing well with only intermittent mild pain and a limping gait of the right hip joint.
Discussion
Fungal infections of the spine are uncommon. In the case of AS, the lumbar spine is the most common site of infection, and approximately 30% of patients have neurological symptoms2. Vinas et al.3 reported 39 cases of AS that were confined to the thoracic and lumbar spine. However, it is possible that multiple bone infections by Aspergillus can occur in immunocompromised patients. Fungal infections in the spine must be suspected if an immunocompromised patient without back pain previously reports new back pain and there are no positive radiographic or MRI findings4. This is even more relevant if aspergillomas of the lung is present4. In our case, when the patient had complained of low back pain for the first time, lumbar radiography did not reveal any abnormality. However, after 6 weeks, lumbar radiography revealed destructive changes of the L3-4-5 vertebral bodies. Initially, tuberculous spondylitis was suspected, but aspergillomas were found in the lung, and MRI showed different findings from tuberculous spondylitis. In the present case, four consecutive vertebral bodies were involved and an abnormal paraspinal signal was relatively well-defined on the initial lumbar spine MRI, which indicated tuberculous spondylitis rather than pyogenic spondylitis. However, there was no paraspinal or intraosseous abscess despite the extensive involvement of the four consecutive vertebral bodies and abnormal paraspinal signal. Based on our experience, tuberculous spondylitis cases have a concomitant paraspinal or intraosseous abscess. Therefore, an absence of a paraspinal or intraosseous abscess appears to be unusual in tuberculous spondylitis. All these findings are similar to Ooji's report4. We reported the MR findings of the same patient previously, and highlighted the importance of differentiating AS and tuberculous spoondylitis5. To our knowledge, this is the first case that underwent selective spinal surgery for segments with a neurological deficit and instability in the treatment of multiple Aspergillus involvement of the cervico-thoraco-lumbar spine and a hip joint. Antifungal agents provide the fundamental cure for spinal fungal infections but surgical intervention is necessary in rare cases6,7. There is no set standard duration for which the medical treatment should continue, and the side effects and therapeutic responses should always be considered depending on the patients' clinical condition and radiological response8. The duration of antifungal therapy should also be determined with same consideration. In our case, the full amount of Amphotericin B was administered to treat lumbar spondylitis. However, the patient remained symptomatic with multiple AS including his right hip joint, while ESR and CRP did not decline. Therefore, Amphotericin B was switched to itraconazole for 8 months, followed by the administration of voriconazole (200 mg bid) for 6 months. Cortet et al.9 recommended itraconazole alone or in combination with a mean treatment duration of 5.5 months for the treatment of AS. Mouas et al.10 reported satisfactory results in 11 patients who received a medial duration of voriconazole therapy of 180 days. In our case, after administering itraconazole for 8 months, it was switched again to voriconazole because the patient's response to itraconazole was slow and the CRP had not returned to normal (1.87 mg/dL). After 6 months of the voriconazole treatment, the CRP decreased to 0.24 mg/dL and MRI revealed almost complete resolution of the inflammation.
Surgical intervention can be considered if there is resistance to medical therapy, neurologic deficits, spinal instability and sepsis2. Although the best approach for surgical intervention is difficult to define, the anterior approach combined with an anterior bone graft with or without posterior instrumentation is essential for decompressing the neural structures. Govender and Kumar8 reported good results using an allograft for anterior interbody fusion in the treatment of AS. Bridewell et al.6 reported that AS had the capability of forming a bony bridge between significant defects after debridement. However, significant medical comorbidities may preclude extensive fusion using combined posterior instrumentation. In our case, anterior decompression with fusion was performed using an autogenous iliac bone graft for lumbar spondylitis on L3-4-5, which was the most severe of the segments. Despite using the most appropriate treatment with antifungal agents, his symptoms became aggravated. After performing anterior interbody fusion for lumbar spondylitis with antifungal agents for 3 months, severe neck pain with radiculomyelopathy and dorsal back pain newly developed, and anterior decompression with anterior interbody fusion using autogenous iliac bone for cervical spondylitis were performed. For thoracic spondylitis, it was decided to perform conservative treatment with antifungal agents, even though the patient complained of thoracic back pain because the patient had only tolerated the selective surgical procedure with acceptable risk. On the final roentgenograms and MRI, spontaneous fusion was observed at the thoracic spine, and successful interbody fusion of the cervical and lumbar spine was noted. The hip roentgenograms revealed subluxation. Therefore, the patient was referred to hip surgeons for the mild hip pain, and was given conservative treatment.
In conclusion, selective spinal surgery with antifungal therapy may be an effective treatment for segments with severe pain and neurological deficits in immunocompromised patients with acceptable risk.