|
 |
- Search
| Asian Spine J > Volume 9(2); 2015 > Article |
Abstract
Purpose
The purpose of this study was to document and evaluate the clinical and radiological results of percutaneous vertebroplasty (PV) as a first line treatment in traumatic non-osteoporotic vertebral compression fractures (TNVCFs).
Overview of Literature
PV is commonly used for osteoporotic and neoplastic compression fractures, however its use in traumatic non-osteoporotic compression fractures is uncertain.
Methods
We included 23 patients with traumatic non-osteoporotic TNVCFs and normal bone mineral densitometry scores who were treated with PV. Pain was evaluated at 2 hours, 1 week, 1 month, 6 months, 1 year, and 2 years post procedure using the 10-point visual analogue scale (VAS). Ronald-Morris disability Questionnaire (RDQ) scores were also collected. Statistical analysis included a 2-tailed t test comparing postoperative data with preoperative values. Range of mobility was also evaluated.
Percutaneous vertebroplasty (PV) has been widely and successfully used in the treatment of osteoporotic and neoplastic vertebral compression fractures. Traditionally, vertebroplasty is used for the treatment of painful primary and secondary osteoporotic compression fractures refractory to medical therapy, pain-inducing fractures caused by invading neoplasms, and in cases of painful osteonecrosis [1]. However, the literature regarding the use of vertebroplasty for traumatic, nonosteoporotic, and/or non-neoplastic, compression fractures remains limited, with studies restricted to a small number of patients [2,3,4,5].
The use of vertebroplasty for patients with traumatic non-osteoporotic vertebral compression fractures (TNVCFs) is complicated since the characteristics of the non-osteoporotic bone itself may influence the efficacy of vertebroplasty and the lack of knowledge about this patient population [6].
There is a single report of patients with TNVCFs treated with vertebroplasty secondary to failure of conservative treatment for a period of 4 months [7]. Another case report discussed only a case treated with vertebroplasty in acute trauma [8].
The purpose of this prospective cohort study was to document and evaluate the clinical and radiological results of PV as a first line treatment in TNVCFs.
Twenty three TNVCFs patients with normal bone mineral densitometry (BMD) scores and treated with PV were included. This study was approved by the Institutional Review Board of Menoufiya University. All patients provided written informed consent. Fourteen patients were daily workers, 5 were students, and 4 were employees.
Patients who presented with trauma induced vertebral compression fracture with intolerable pain and approved for vertebroplasty were included in the study. Traumatic event was defined as an event that resulted in sudden physical injury, such as an accident or severe fall. Only patients with traumatic injury who had a normal BMD t-score (-1 or higher) were included in the study.
Patients who had a history of osteoporosis, multiple myeloma, or a concomitant contributory history of steroid use were excluded. Patients with unstable burst fractures or fractures extending into the posterior elements were also excluded from the study.
Patients with traumatic compression fractures were treated with vertebroplasty when their pain was intolerable. Vertebroplasty was performed with the patient under conscious sedation or general anesthesia, as specified previously [9,10]. All vertebroplasty procedures were performed under the guidance of C-arm fluoroscopy, and an 11- or 13-gauge needle was used to traverse the right, left, or both pedicles. The needle was introduced under continuous fluoroscopic guidance into the anterior one third of the vertebral body closest to the midline as possible, without compromising the medial wall of the pedicle or the anterior cortex of the vertebral body. Once the needle had been inserted into the vertebral body, the contrast agent Isovist-300 was injected in anticipation of leakage. The needle was then cleared with saline. The cement, consisting of 40 g of methylmethacrylate powder and 20 mL of monomer liquid were mixed together. Cement was injected into the vertebral body until the injected cement reached the posterior one fourth of the vertebral body, or if epidural, venous, or trans-endplate extra-vasation of cement was observed [9,10,11,12,13]. Patients were kept supine for 2 hours after the procedure.
Patients approved for PV were evaluated pre- and postoperatively by both, quantitative, and qualitative measurements. Quantitative measurements were collected by the Roland-Morris Disability Questionnaire (RDQ) [14] and the visual analog scale (VAS) for "pain at rest" and "pain with activity," with 0 as no pain and 10 as the worst pain ever experienced. Qualitative data were also collected. The preoperative and 2-hour postoperative data were collected in the hospital; follow-up data at 1 week, 1 month, 6 months, 1 year, and 2 year were collected further.
VAS and RDQ scores were analyzed by a 2-tailed t test at each follow-up point to evaluate the change in pain and RDQ score from preoperative values. The VAS and RDQ scores were also averaged at each follow-up period to allow further comparison. The difference between mobility at each follow up time point was calculated by chi-square test (χ2).
Twenty three patients with 29 TNVCFs met the inclusion criteria of the study. The average age of the patients was 36 years of age (range, 16-57 years), and 16 were women. Seventeen patients sustained a fracture following a fall from height and 6 patients were in motor vehicle crashes.
One level was treated in 20 patients, the levels treated varied, with 11/29 (38%) fractures occurring at L1 alone, and 3/29 (10.3%) occurring at L2 alone. The remaining fractures 6/29 (20.7%) occurred at T12 alone, and the levels T12+L1+L2 were treated in the remaining 3 patients 9/29 (31%).
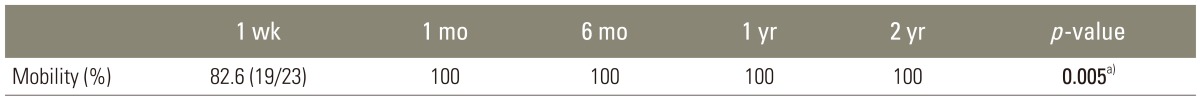
Preoperative data were collected on mobility. 5/23 (21.7%) patients could walk >100 meters, 15/23 (65.2%) patients could walk <100 meters, and 3/23 (13%) patients were bedridden. All patients had significantly improved mobility, by the end of the first postoperative month (Table 1). All patients were evaluated with preoperative X-ray, computed tomography bone window with reconstruction, and spinal MR images. The mean loss of height was 17% (ranging from 10% to 33%). PV was performed on 17/23 patients with conscious sedation and 6/23 with general anesthesia. The average cement volume injected into each vertebra was 2.5 mL (ranging from 2.1 to 3.2 mL). The time between the trauma and the vertebroplasty ranged from 1 to 7 days, depending on patient's arrival in the hospital.
Pain on rest and activity were quantitatively measured in all patients preoperatively; 2 hours postoperatively; and at 1 week, 1 month, 6 months, 1 year, and 2 year. A highly significant decrease was found in "pain at rest" at all follow-up evaluations, as compared with preoperative values (p<0.001). A highly significant decrease in "pain with activity" at the 2-hour postoperative follow-up was also found (p<0.01).
The RDQ scores were also collected and analyzed at all follow-up periods, and a highly significant decrease in RDQ scores at the 1-month follow-up was found (p<0.001). Furthermore, throughout the 2-year follow-up period, the patients experienced, on average, a sustained decrease in pain at rest and with activity (Fig. 1) and in the RDQ scores (Fig. 2), as compared with respective preoperative scores.
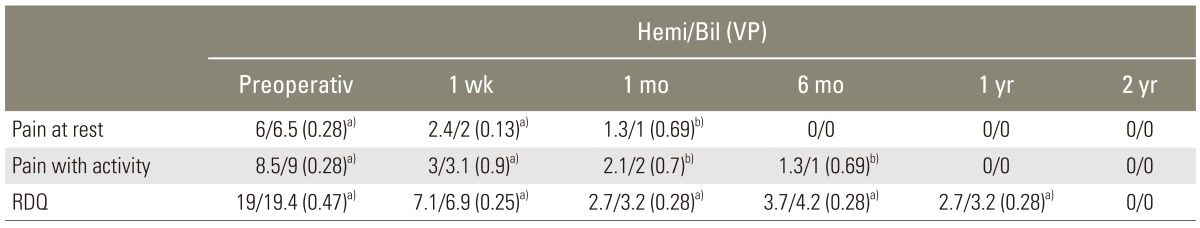
Out of the 20 patients treated for single level TNVCF, 12 patients underwent bilateral vertebral filling PV and 8 patients underwent hemivertebral filling PV. Additionally, 2 of the 3 patients treated with 3 level TNVCFs underwent unipedicular filling PV. Hemi and bilateral vertebral filling had no statistically significant differences in pain at rest and with activity, and RDQ scores (Table 2).
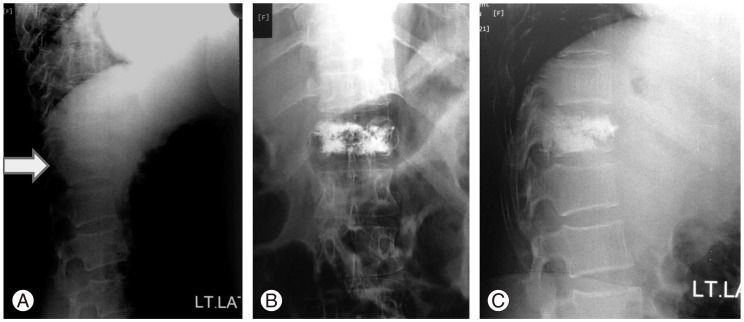
A forty-nine year old female with a history of fall from height was admitted to the hospital with severe intractable pain. She had >20% anterior compression of the T12 and 13 angle of kyphosis. PV was performed on the patient using the bilateral pedicle approach, after obtaining informed consent. A total of 3.2 mL of polymethylmethylacrylate (PMMA) cement was injected in the T12 vertebral body. The patient reported a significant pain reduction at the 2 hour follow-up period, and showed improved mobility on the following day. The improvement in pain score and mobility continued throughout the follow-up (Fig. 3).
PV involves the injection of cement through a needle into a collapsed or weakened vertebra. The currently accepted indications for the technique are (1) osteoporotic vertebral compression fractures causing moderate to severe pain and unresponsive to conservative therapy, (2) painful metastasis and multiple myeloma, (3) painful vertebral hemangioma, (4) vertebral osteonecrosis, and (5) reinforcement of a pathologically weak vertebral body before a surgical stabilization procedure [15].
There is a past history of spinal kyphosis in most of the locally residing patients treated conservatively after traumatic compression fractures, due to lack of bed rest. The study was designed as such, since most of the fracture patients were daily workers and students, and their families could not afford the financial expenses of prolonged bed rest.
The current study was a unique prospective analysis that showed the benefits of PV in achieving a good outcome in TNVCFs cases. The use of vertebroplasty for TNVCFs was particularly important due to the inherent problems with more traditional treatments for these injuries, such as hardware failure and substantial narcotic usage [12,16].
A significant decrease in "pain at rest" was observed at all follow-up evaluations, beginning at 2-hours. Additionally, a significant improvement in "pain with activity" was also observed at the 2-hours follow-up and continued for the entire follow-up period. All patients reported increased mobility and decreased narcotic usage; 82.6% of all patients experienced an increase in mobility by the first week and continued to improve throughout the 2-year follow-up period; and 69.5% of the patients reported a decrease in narcotic usage by the end of first week postoperatively and have completely stopped their narcotic usage by the end of the 1 year follow-up period. All patients who were bedridden or had restricted mobility were able to return to their normal activities, while using non-narcotic analgesics or no medications.
Patients included in this study were treated by vertebroplasty at the initial presentation in the hospital. The interval between the trauma event and vertebroplasty ranged from 1 to 7 days (depending on the patient's arrival at the hospital). This was a much shorter time between fracture and procedure than is generally recommended (usually 6-12 weeks) [11].
Knavel et al. [17] defined hemivertebroplasty as "barium-opacified PMMA predominantly in one side of the vertebral body". Furthermore, if PMMA crossed the midline, they restricted the definition of hemivertebroplasty to patients in whom PMMA traversed only <10% of the width of the predominantly unfilled hemivertebra. They concluded from their retrospective study that, hemivertebroplasty in which PMMA is instilled in only one half of the vertebral body was as efficacious as bilateral PMMA infusion [17]. The results of the current study corroborated Knavel's study, since it showed no statistically significant differences in pain at rest and with activity, and RDQ scores, between hemivertebroplasty and bilateral vertebral filling.
Potential clinical complications of PV documented in either case reports or case series included infection, bleeding , back pain, rib fracture, pulmonary embolism, pneumothorax from punctured lung, transient arterial hypotension, fever, optic neuritis, and other neurological complications [4,11,12,18]. A review of all major vertebroplasty series in well-trained hands had a clinical complication rate ranging from 1% to 10%; osteoporotic patients had a complication rate of approximately 1% to 3%; hemangioma patients had a complication rate of 5%; and patients with metastasis to the vertebra had a complication rate of 10% [4].
The concern of performing vertebroplasty on patients with traumatic fractures is the possible increased rate of cement extravasation and posterior displacement due to possible endplate fractures and damage to the posterior and anterior longitudinal ligaments [4,19].
Additionally, patients without osteoporosis, generally have very hard bone requiring greater force and effort for the needle placement within the vertebral body. This can potentially result in greater injection pressure with subsequent increased risk of a cement leak.
Despite the above mentioned concerns, no major complications were encountered in the study. Asymptomatic extravasations were encountered in only 3 cases i.e., para-vertebral, epidural and disc space extravasations in 1 patient, extravasations of cement into the disc space in another patient, and extravasations in epidural veins in the third patient. No other complications were encountered.
Several small studies have demonstrated good results from vertebroplasty in painful TNVCFs [3,4,7,8]. Two studies of patients with TNVCFs showed a decrease in pain in all subjects with limited extravasation of cement, all of which were asymptomatic [5,7]. The results of the current study, confirmed these earlier results. However, our study included a larger patient population and for the longest follow-up period (2 years) published to date. Additionally, the current results were similar to the vertebroplasty outcomes predominantly in patients with osteoporosis in a previous study on a larger patient series [12]. The similarities in the results of the current and former study [12], demonstrated the efficacy of vertebroplasty for patients with traumatic vertebral compression fractures.
Patients with nonosteoporotic compression fractures have very hard bone, requiring greater force and effort for the placement of the needle within the vertebral bodies. Additionally, due to the attenuated nature of the bone in patients without osteoporosis, there is a potential for decreased capacitance to accept cement, as compared to patients with osteoporosis. We found that the attenuation of the patient's bone did not adversely affect the injection of cement, as the average amount of cement injected in the current study was 2.5 mL per each vertebra. The amount of cement injected was comparable to previously reported cases with osteoporosis [12].
All previous studies in the literature had their own limitations, such as being retrospective, having small groups of patients, lack of patient participation in the entire follow-up period, other confounding medical treatments that might have affected their outcomes and pain relief, and persistence of other causes that produce pain [7,8,20,21]. The current study was a prospective cohort study on a large number of patients with TNVCFs alone, with the exclusion of patients with other medical or surgical problems. All patients were treated on the initial hospital visit without starting medication. The entire patient cohort participated in the 2 years follow-up period.
Patients who present with compression fractures experience a high level of pain and disability. The patients are mostly daily workers or students who have an urgent need for early ambulation. Our study confirmed that PV offers statistically significant benefits in decreasing pain and increasing mobility. It is of great importance that these patients resume daily activities as early as possible. The current study also showed that PV offers statistically significant and long term, sustained good outcomes suggestive of technical effectiveness, durability, and safety as a first line treatment in patients with TNVCFs.
Conflict of Interest
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
1. McGraw JK, Cardella J, Barr JD, et al. Society of Interventional Radiology quality improvement guidelines for percutaneous vertebroplasty. J Vasc Interv Radiol 2003 14:S311–S315. PMID: 14514838.


2. Amoretti N, Hovorka E, Marcy PY, et al. Burst fracture of the spine involving vertebrae presenting no other lesions: the role of vertebroplasty. Clin Imaging 2005 29:379–382. PMID: 16274889.


3. Chen JF, Wu CT, Lee ST. Percutaneous vertebroplasty for the treatment of burst fractures. Case report. J Neurosurg Spine 2004 1:228–231. PMID: 15347011.


4. Chen JF, Lee ST. Percutaneous vertebroplasty for treatment of thoracolumbar spine bursting fracture. Surg Neurol 2004 62:494–500. PMID: 15576113.


5. Huet H, Cabal P, Gadan R, Borha A, Emery E. Burst-fractures and cementoplasty. J Neuroradiol 2005 32:33–41. PMID: 15798611.


6. Stadhouder A, Buskens E, de Klerk LW, et al. Traumatic thoracic and lumbar spinal fractures: operative or nonoperative treatment: comparison of two treatment strategies by means of surgeon equipoise. Spine (Phila Pa 1976) 2008 33:1006–1017. PMID: 18427323.


7. Knavel EM, Thielen KR, Kallmes DF. Vertebroplasty for the treatment of traumatic nonosteoporotic compression fractures. AJNR Am J Neuroradiol 2009 30:323–327. PMID: 19039045.



8. Tender GC, Serban D. Traumatic spinal fracture treated by vertebroplasty: a case report. J Med Case Rep 2012 6:390PMID: 23171525.




9. Jensen ME, Evans AJ, Mathis JM, Kallmes DF, Cloft HJ, Dion JE. Percutaneous polymethylmethacrylate vertebroplasty in the treatment of osteoporotic vertebral body compression fractures: technical aspects. AJNR Am J Neuroradiol 1997 18:1897–1904. PMID: 9403451.


10. Koch CA, Layton KF, Kallmes DF. Outcomes of patients receiving long-term corticosteroid therapy who undergo percutaneous vertebroplasty. AJNR Am J Neuroradiol 2007 28:563–566. PMID: 17353337.


12. Layton KF, Thielen KR, Koch CA, et al. Vertebroplasty, first 1000 levels of a single center: evaluation of the outcomes and complications. AJNR Am J Neuroradiol 2007 28:683–689. PMID: 17416821.


13. McDonald RJ, Trout AT, Gray LA, Dispenzieri A, Thielen KR, Kallmes DF. Vertebroplasty in multiple myeloma: outcomes in a large patient series. AJNR Am J Neuroradiol 2008 29:642–648. PMID: 18202234.



14. Trout AT, Kallmes DF, Gray LA, et al. Evaluation of vertebroplasty with a validated outcome measure: the Roland-Morris Disability Questionnaire. AJNR Am J Neuroradiol 2005 26:2652–2657. PMID: 16286418.


15. Predey TA, Sewall LE, Smith SJ. Percutaneous vertebroplasty: new treatment for vertebral compression fractures. Am Fam Physician 2002 66:611–615. PMID: 12201552.

16. Afzal S, Akbar S, Dhar SA. Short segment pedicle screw instrumentation and augmentation vertebroplasty in lumbar burst fractures: an experience. Eur Spine J 2008 17:336–341. PMID: 18193300.



17. Knavel EM, Rad AE, Thielen KR, Kallmes DF. Clinical outcomes with hemivertebral filling during percutaneous vertebroplasty. AJNR Am J Neuroradiol 2009 30:496–499. PMID: 19147722.



18. Layton KF, Thielen KR, Cloft HJ, Kallmes DF. Acute vertebral compression fractures in patients with multiple myeloma: evaluation of vertebral body edema patterns on MR imaging and the implications for vertebroplasty. AJNR Am J Neuroradiol 2006 27:1732–1734. PMID: 16971624.


19. Verlaan JJ, van de Kraats EB, Oner FC, van Walsum T, Niessen WJ, Dhert WJ. Bone displacement and the role of longitudinal ligaments during balloon vertebroplasty in traumatic thoracolumbar fractures. Spine (Phila Pa 1976) 2005 30:1832–1839. PMID: 16103852.


20. Do HM, Kim BS, Marcellus ML, Curtis L, Marks MP. Prospective analysis of clinical outcomes after percutaneous vertebroplasty for painful osteoporotic vertebral body fractures. AJNR Am J Neuroradiol 2005 26:1623–1628. PMID: 16091504.


21. Kallmes DF, Comstock BA, Heagerty PJ, et al. A randomized trial of vertebroplasty for osteoporotic spinal fractures. N Engl J Med 2009 361:569–579. PMID: 19657122.



Fig. 1
Graph of average pain at rest and with activity based on VAS score, following vertebroplasty. VAS, visual analogue scale; Proep., preoperative.
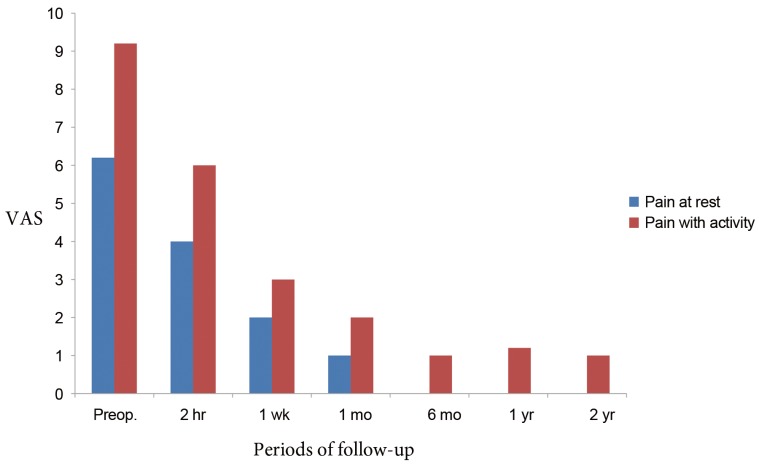
Fig. 2
Graph of average RDQ scores following vertebroplasty. RDQ, Ronald-Morris disability Questionnaire; Proep., preoperative.
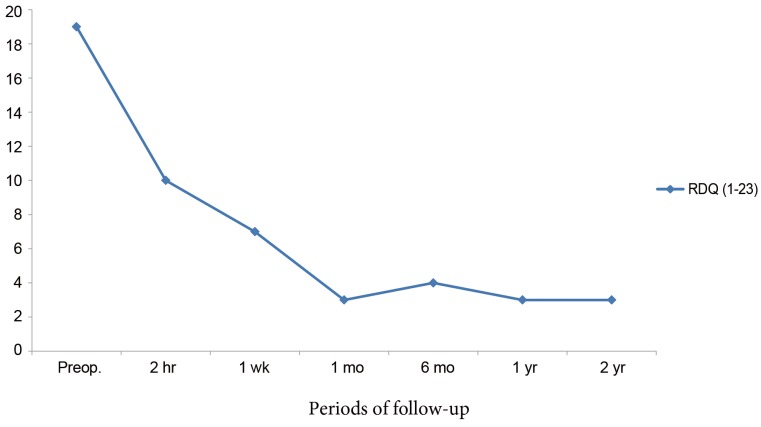
Fig. 3
(A) Lateral plain X-ray showing the T12 compression fracture (arrow denoting fractured T12 vertebra). (B, C) Plain X-ray anteriorposreior and lateral views show adequate filling of the injected cement in T12 vertebra.