Introduction
Congenital spinal canal stenosis is one pathomechanism that causes cervical myelopathy. Most cervical spinal stenosis generally occurs below the level of C21, but occasionally is found above. Myelopathy resulting from upper cervical spinal stenosis due to a defective posterior arch2,3, and a hypoplastic atlas ring with a completely developed posterior arch has been reported.
Case Reports
Case 1
A 79 year old male presented complaining of clumsiness in both hands and walking difficulty.
The symptoms developed spontaneously three months prior to the initial visit without any trauma, which aggravated over the last month. Walking was almost impossible without assistance and the clumsiness was most severer in the right hand.
Physical examination revealed that in the right upper extremity all muscle power below the level of the trapezius markedly decreased to 'poor,' while decreasing slightly to 'good' in the left upper extremity. In the right lower extremities muscle power below the right hip decreased to 'poor.' Sensory examination revealed hypesthesia in the region below the level of the C5 dermatome.
The patient exhibited finger escape sign in the right hand, and the grip and release test showed a decrease to one time within 10 seconds in the right hand and 10 times in the left hand within 10 seconds (normal value: over 20 times in 10 seconds). Simple lateral radiographs showed severe atlas hypoplasia and degenerative changes at all cervical levels. Even though atlantodental interval (ADI) was increased to 3.5 mm, there was no finding of severe instability on flexion-extension lateral radiographs (Fig. 1A). The configuration of the upper cervical spine could be clearly seen in the preoperative three-dimensional computed tomography (3D-CT) images. The atlas ring was quite smaller than normal, and severe compression of the spinal cord by soft tissue posterior to the odontoid process of C2, as well as an intramedullary high signal intensity area could be observed in T2-MRI. Space available for the cord (SAC) in the atlas was measured to be 6.9 mm. (Fig. 1B and C).
Case 2
A 49 year old male presented complaining of a squeezing feeling at the midsection and tingling sensations in both upper and lower extremities.
Diagnosis with ossification of the posterior longitudinal ligament (OPLL) of the cervical spine was made before hospital admission. The symptoms started to develop approximately three months prior to the initial visit. There was no difficulty in walking, but the patient showed Lhemitte's sign when extending the neck abruptly. The patient denied any sensory and motor change on physical examination. Simple lateral radiographs revealed OPLL in the region of C2 through C5 together with atlas hypoplasia (Fig. 2A). Magnetic resonance imaging showed spinal canal stenosis from C1 to C5, and especially marked narrowing of the spinal canal with cord compression at the atlas ring and an intramedullary high signal intensity area (Fig. 2B). Surgical decompressive laminectomy of the posterior C1 ring was performed, relieving compression of the spinal cord, which was thought to be the main cause of the symptoms. A preoperative JOA score of fifteen points recovered up to sixteen points within a year after the operation, and the postoperative cervical condition was observed well maintained in simple lateral radiographs taken fourteen months after the operation (Fig. 2C). In spite of sufficient decompression of the spinal cord on the postoperative MRI, an intramedullary high signal intensity area was still present at the previous region (Fig. 2D).
Case 3
A 62 year old male presented complaining of paresthesia in the fingertips of both hands and feet.
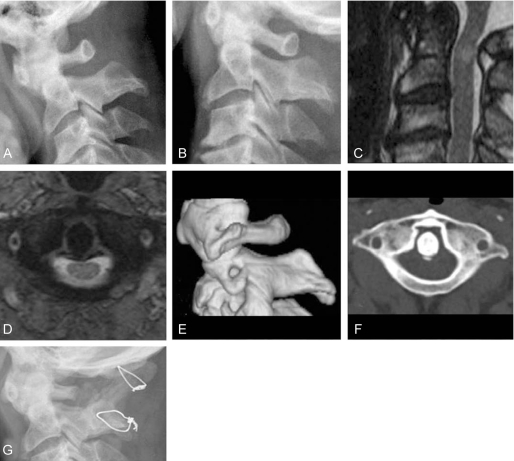
The symptoms started to develop after falling down approximately three months before admission. There was no difficulty in walking, but insignificant clumsiness in fine activities like using chop sticks and buttoning a shirt. Physical examination revealed no definite neurological symptoms except hypesthesia of both hands and feet, nor were any upper motor neuron signs or abnormal reflexes shown. Suboccipital headaches were, however, noted. There were findings of atlas hypoplasia and an increase of ADI to 3.1 mm shown in simple lateral radiographs, and an angular difference of thirteen degrees was measured in flexion-extension lateral radiographs (Fig. 3A and B). MRI revealed severe compression of the spinal cord by stenosis of the hypoplastic atlas and an intramedullary high signal intensity area (Fig. 3C and D). Marked atlas hypoplasia and stenosis could also be observed in the 3D-CT and axial CT scans (Fig. 3E and F). As surgical treatment, a posterior C1 ring laminectomy with autogenous iliac bone graft and occipitoatlanto-axial fusion using wire fixation was performed. Halovest external immobilization was applied postoperatively for three months (Fig. 3G). The patient's symptoms recovered completely from the preoperative JOA score of thirteen points to a JOA score of seventeen points.
Discussion
To understand the congenital malformation of the atlas, it is required to know about the process of its formation and development. Formation of the atlas starts to develop from the three ossification centers originating from the first sclerotome. Both lateral ossification centers begin growing posteriorly within six to seven weeks of embryogenesis to form the posterior arch and unite against each other within four months. The anterior center, however, forms part of the anterior tubercle and arch, and uniting with the two lateral ossification centers at six or seven years after birth8. Therefore, it is considered that the cause of atlas hypoplasia may be premature fusion or incomplete posterior development in the process of union of the two halves5. It is reported that the average AP diameter of the normal atlas is 16~20 mm, and it is generally known that clinical symptoms appear below 10 mm in diameter7. The first report about atlas hypoplasia was made by Wackenheim5, who reported a case of atlas hypoplasia having occipital neuralgia, but not accompanying myelopathy. The first report of atlas hypoplasia with myelopathy was made by Sawada et al.7 who reported one case of surgical treatment for a patient having only 7 mms of anterior-posterior diameter of the spinal canal.
One case report each by Nishikawa et al.5 and Tokiyoshi followed and two additional cases by Phan et al.6 were reported, and most recently Nichikawa et al.5 reported three cases. All these 10 cases are thought to have myelopathy due to atlas hypoplasia. In addition, there are a few case reports of myelopathy caused by atlas hypoplasia associated with pathology of surrounding structures9,10. Sato et al.9 reported two cases of myelopathy by hypertrophy of the odontoid process of the C2 spine and hypertrophic osteoarthritis of the C1-2 lateral mass. Yamashita et al.10 reported a case of myelopathy by atlas hypoplasia associated with pseudotumor posterior to the odontoid process, which was similar to one of the current case series, but it differed in that the current case had no trauma. All together the current 3 cases add up just a few to the previously reported cases. As can be seen in the three current cases, the authors' have shown myelopathy by a compressed spinal cord due to atlas hypoplasia. In Case 1, soft tissue swelling posterior to the odontoid process of the C2 spine was associated, and in Case 2, ossification of the posterior longitudinal ligament at the subaxial region was associated. In Case 3, in spite of the spinal stenosis throughout the entire cervical spine, the assumed main cause of the myelopathy was the stenosis of the atlas because of the intramedullary high signal lesion located anterior to the posterior ring of the atlas in T2 MRI. In the current 3 cases, intramedullary high signal lesions at the maximum compression level were observed at the compressed part of the spinal cord, and decompression through the posterior C1 ring laminectomy was performed accordingly in all cases. In Case 3, because of instability in preoperative flexion-extension lateral radiographs, an occipitocervical fusion was performed after a C1 ring laminectomy and then Halovest external immobilization was applied.
In the current authors' three cases, all of the patients' symptoms were recovered remarkably.
There are very few incidences of myelopathy due to atlas hypoplasia worldwide. By adding these three cases, the authors in treating myelopathic patients suggested to include atlas hypoplasia observed in simple lateral radiographs as one differential diagnosis. Also the authors think that long-term follow up of these and other cases is necessary to better understand the reason why this disease develops in adults only, and not in children, and why it develops spontaneously without any trauma, even though it is assumed to be a congenital malformation. Added with other cases, it may be necessary to establish a disease entity by analyzing common aspects of the natural process of the development of myelopathy in patients with atlas hypoplasia.