Assessment of Great Vessels for Anterior Access of L5/S1 Using Patient Positioning
Article information
Abstract
Study Design
This was a prospective cross-sectional study.
Purpose
The aim was to describe the effect of patient positioning, from supine to lateral decubitus position, on the width of the L5/S1 anterior disk space defined by the great vessels.
Overview of Literature
The application of the lateral decubitus position interbody fusion has been rapidly increasing; however, there are concerns regarding the access to the lumbosacral region due to the great vessels, which necessitates further morphometric data.
Methods
A total of 20 consecutive live patients awaiting lumbar surgery were subjected to two magnetic resonance imaging scans on the same day in both supine and lateral decubitus positions at a single center to investigate the anterior L5/S1 disk space.
Results
The bare anterior L5/S1 disk window was present in all patients of this study population, and the mean width was 27 mm in the supine and 22 mm in the lateral decubitus position, with a mean reduction of 5.2 mm between the positions. The oblique corridor angle was measured at a mean of 33°.
Conclusions
The bare window of L5/S1 disk space was present within this population group, and it was found to be mobile and changed significantly with patient positioning. Therefore, the spine surgeon or the access surgeon must consider the increased potential vascular risk during disk access in lateral decubitus anterior lumbar interbody spinal fusion surgery.
Introduction
The resurgence in anterior lumbar interbody spinal fusion (ALIF) has been a recent emerging trend in lumbar spine surgery. This technique has been largely stimulated by the growing body of evidence for its efficacy [1-4] and the renewed interest resulting from less-than-ideal experiences of posterior-based approaches such as transforaminal or posterior lumbar interbody fusion [5-8] as surgeons emphasize on harmonizing the patient’s sagittal balance [9-11]. Traditionally, the ALIF procedure involved positioning the patient supine and accessing the disk space through retroperitoneal exposure. The peritoneal contents are moved away from the anterior spine to visualize the great vessels that overlie the disk spaces of the lumbar sacral junction. Access is provided between the bifurcated aorta and the inferior vena cava, and these vessels are carefully mobilized to obtain adequate working space for interbody fusion [8]. Surgeons performing the procedure should be prepared to address the potential for visceral and vascular complications, and vascular injury remains one of the most significant concerns as the bleeding, if encountered, is generally significant [1,12,13].
The development and availability of modern spinal instrumentation and retractor systems have prompted a newer iteration of the established ALIF surgical technique through the same access in the lateral decubitus position for the L4/5 and L5/S1 disk space, which has been coined the term oblique lumbar interbody fusion (OLIF) or lateral ALIF [14-16]. Utilization of radiolucent spine-mounted retractor systems with direct illumination allows for a minimally invasive surgical technique. Several anatomical studies have been performed to demonstrate the effectiveness of lateral decubitus positioning in increasing the anterior-to-psoas (ATP) space with gravity-assisted movement of the aorta between L1 and L5 [17-19]. These studies have validated the utilization of the variant form of lateral access ATP surgery. However, there is still a concern for vascular injury to the L5/S1 disk space [20-23]. It is also uncertain whether lateral decubitus positioning affects this risk profile by the potential mobility of the great vessels into the surgical window due to gravity [24].
Studies published till date in the literature have investigated the anatomy of the oblique corridor of the L5/S1 disk space only in a single position. Therefore, the purpose of this study was to document and describe the effect of patient positioning, from supine to intraoperative simulating lateral decubitus position, on the width of the L5/S1 bare anterior disk space defined by the great vessels.
Materials and Methods
1. Participants
We conducted a prospective study of 20 consecutive consenting patients awaiting spinal surgery of the lumbar spine at a single institution between (Spine Ortho Clinic, Melbourne Australia) July and December 2017. The cohort included patients with lumbar degenerative disk disease, including spondylolisthesis, spinal stenosis, and herniated/ruptured disks. Those patients having undergone a previous spine surgery or with trauma, tumor, infections, and tandem stenosis or congenital pathologies affecting the spinal cord were excluded. To eliminate confounding bias, those patients having transitional anatomy at the L5–S1 level (lumbarization or sacralization) were also excluded.
Magnetic resonance imaging (MRI) scans were taken at a single center (MIA Radiology Australia, Frankston Private Hospital), and each patient underwent two MRI scans on the same day in both the supine and right lateral decubitus positions (3T MRI; Siemens, Munich, Germany; image thickness, 2 mm). All images were outputted in DICOM (Digital Imaging and Communication in Medicine) and then converted into Mimics 10.0 (Materialise, Leuven, Belgium) for measurements using the InteleViewer software (Intelerad Medical Systems, Montreal, Canada). Parameters were measured and recorded with T2 sequence sagittal and axial image slices taken at the midpoint of the L5/S1 disk space in parallel with the superior endplate of S1.
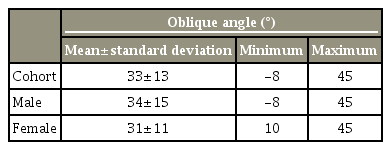
Several quantifiable parameters were arbitrarily described for the purpose of this study. The bare window (BW) at the L5/S1 level was documented as follows: the distance between the medial edge of the left common iliac vein (LCIV) and the right common iliac vein (RCIV) on the axial image, which was recorded in millimeters for absolute figures and percentage figures to quantify the change of width in the anterior disk space by position. The oblique angle (OA) at L5/S1 was also measured; this was defined as the angle between the center of the disk space to the center of the spinal canal and the line that is drawn from where the LCIV touches the anterior annulus to the posterior midpoint of the disk space (Fig. 1). These measurements were recorded for both supine and lateral decubitus positions in the MRI scans by two independent observers, a spine fellow (S.R.) and a consultant radiologist (R.S.), and the averages were recorded.

Measurement parameters at L5/S1. A, right common iliac vein; B, left common iliac vein; O, center of L5/S1 disk; P, posterior disk midpoint; AB, bare window; OPB, oblique angle.
Approval from the Institutional Review Board was not obtained as our institution did not require one for routine clinical care protocols. The patient cohort was prospectively informed of the study design and obtained informed consent for the participation in the study.
2. Statistical analysis
Data were presented as mean±standard deviation. Paired t-test was used for comparing the BW in the supine and lateral positions. Sample t-test was used to compare the BW between sexes. A p-value of <0.05 was defined as statistically significant.
Results
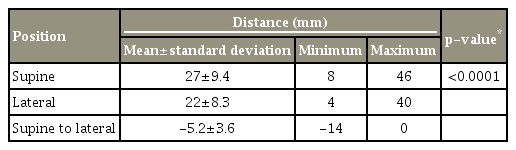
All results are presented in Tables 1 and 2. A total of 20 consenting patients were included in this study. Regarding patient demographics, there were 12 males and eight females, and the average age of the patients was 73 years (range, 69–80 years).
The BW in the supine position was 27±9.4 mm (range, 8–46 mm). The BW in the lateral position was 22±8.3 mm (range, 4–40 mm). The change in BW from the supine to lateral position was −5.2±3.6 mm (range, −14 to 0 mm). The proportion of change in the area of BW at L5/S1 was 20%±12% (range, 0%–45%). This change was statistically significant (p<0.001) and indicated a reduction in the absolute width (mm) between the iliac veins when placed in the lateral decubitus position.
The OA in the lateral position was 33°±13° (range, 8°–45°). These values were 34°±15° (range, 8°–45°) in males and 31°±11° (range, 10°–45°) in females. These values indicate that between the patients, regardless of sex, the obliquity of the great vessel location anterior to L5–S1 disk space remains relatively constant.
Discussion
Recently, there has been a substantial interest in ALIF surgery via the lateral decubitus position as it retains the benefits of highly reliable fusion, significant corrective potential, and minimally invasive nature as well as due to its ease of integration to the workflow for lateral surgeons performing lateral lumbar interbody fusions at higher lumbar levels [1,9,10,12,25,26]. This approach has the potential to reduce the morbidities associated with ALIF such as ileus, tissue retraction, potential vascular injury, and peritoneal breach or disruption [1,12,13]. Often when new surgical methods are introduced without a significant body of data and outcomes, adverse, or unexpected events could occur in the early period of adoption. As such, procedures such as OLIF L5–S1 (Medtronic, Minneapolis, MN, USA) and lateral ALIF (NuVasive, San Diego, CA USA) have been associated with similar complication profiles as those of ALIF, in particular vascular injury. As a result, this has persuaded some governing bodies such as the Japan PMMA (polymethyl methacrylate) to restrict the use of such procedures and mandated specific training and certification before the adoption [22,23]. The feasibility and refinement of this technique in the lateral decubitus position is still desired, and the present study illustrates some anatomical consideration in the surgical planning for lateral access ATP at L5/S1.
In the current study, the BW was clearly present in all subjects irrespective of the positioning at L5/S1 (Fig. 2). Davis et al. [18] conducted a cadaveric study of the oblique corridor in the lateral decubitus position and similarly reported that clear access was found in all subjects at the L5/S1 disk space. Furthermore, Molinares et al. [25] concluded that the use of common iliac vascular retraction methods found in ALIF procedures would have allowed access for an interbody cage to the L5/S1 disk space in all patients in their study.
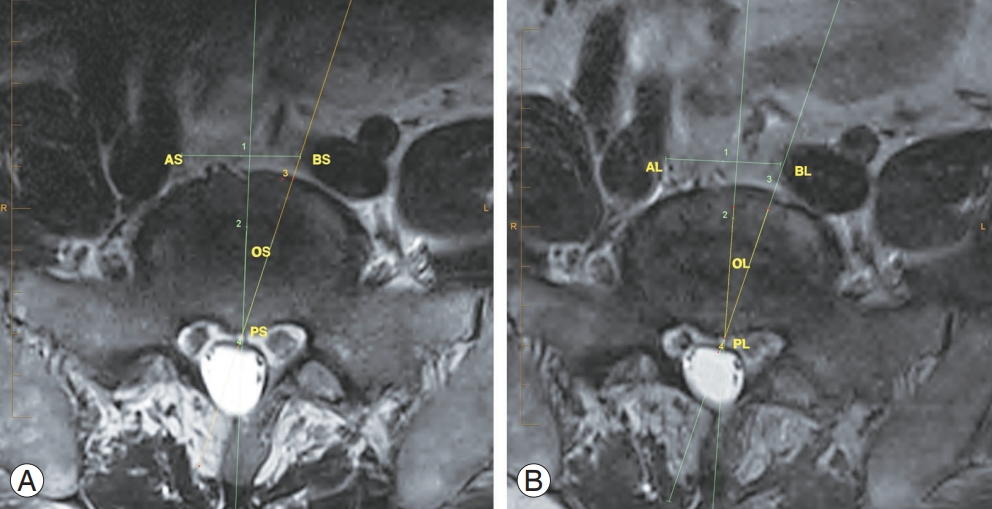
Clear bare window observed in (A) supine position magnetic resonance imaging and (B) lateral decubitus with minimal change in size of L5/S1 disk by position. ASBS & ALBL, L5/S1 bare window; OSPSBS & OLPBL’, oblique angle; AS & AL, right common iliac vein; BS & BL, left common iliac vein; OS & OL, center of L5/S1 disk; PS & PL, posterior disk midpoint.
In our study, the mean BW measurements were 27±9.4 mm (range, 8–46 mm) in the supine position and 22±8.3 mm (range, 4–40 mm) in the lateral position. These measurements were considerably different from those of previous anatomical studies, such as 14.75±6.9 mm [18], 10±8.3 mm [25], and 15.9±9.3 mm [27]. We believe that the larger measurements of our study than those documented in the previous literature could be due to the difference in definitions of the oblique window. The abovementioned studies defined the BW as the distance between the midsagittal line of the inferior end plate of L5 and the medial border of the LCIV in the axial view. In our study, BW was defined as the absolute distance between the two common iliac veins at the level of the midpoint of the L5/S1 disk in the axial view. Therefore, our BW appears to be larger, and we believe that our definition of the BW is more surgically practical for ALIF in the lateral decubitus position. Song et al. [28] shared a similar definition and reported a similar mean area of 29.46 mm, and they concluded that this definition validated the anatomical feasibility of oblique access ATP at L5/S1.
We observed large variability in the BW in our study cohort, which was due to a high or low bifurcation in relation to L5 vertebral body. The largest BW values were 46 and 40 mm, whereas the smallest BW values were 8 and 4 mm in the supine and lateral positions, respectively. This highlights the importance of preoperative measurements or the evaluation of the presence and size of BW in planning for lateral decubitus position ALIF access of L5/S1. Liu et al. [27] described that patients with an oblique corridor of <1.00 cm were impractical for lateral position ALIF at L5/S1. Their guideline was limited by the dimensions of an extreme lateral interbody fusion cage, and it is our opinion that in patients with BW <1.5 cm and the absence of perivascular fat, extreme caution should be taken in this approach.
Currently, there is no study that directly compares the L5/S1 BW size between the supine and lateral decubitus position, which simulates the intraoperative position in lateral ALIF. In the present study, we observed a mean reduction of −5.2±3.6 mm in the BW between the supine and lateral positions that was found to be statistically significant (p<0.001) (Fig. 3). We believe that this effect was due to the gravitational downward pull on the LCIV and the left common iliac artery. A similar observation was reported by Deukmedjian et al. [24] in their morphometric study wherein they found the iliopsoas to be a static complex and the greater vessels to be mobile when repositioned from the supine to lateral decubitus position. In addition, the range of reduction was −14 to 0 mm, which implies that in some instances the oblique corridor disappeared with positioning (Fig. 4). Due to this, the spine surgeon must consider the increased potential of vascular risk during disk access to the L5/S1 disk space in lateral decubitus ALIF. We recommend that patients undergoing lateral decubitus ALIF should be routinely screened by preoperative MRI evaluation in the lateral position to accurately assess and evaluate the feasibility of lateral surgical access to the L5/S1 disk space.

Reduction in size of bare window area of L5/S1 disk by position. (A) Supine position MRI and (B) lateral decubitus MRI. ASBS & ALBL, L5/S1 bare window; OSPSBS & OLPBL’, oblique angle; AS & AL, right common iliac vein; BS & BL, left common iliac vein; OS & OL, center of L5/S1 disk; PS & PL, posterior disk midpoint; MRI, magnetic resonance imaging.
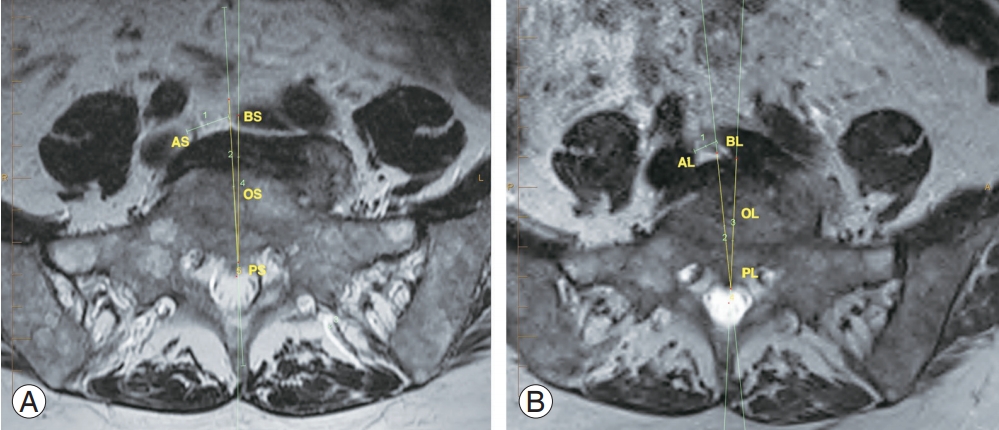
Reduction in size of bare window area of L5/S1 disk by position, with left common iliac vein crossing over the midline. (A) Supine position MRI and (B) lateral decubitus MRI. ASBS & ALBL, L5/S1 bare window; OSPSBS & OLPBL’, oblique angle; AS & AL, right common iliac vein; BS & BL, left common iliac vein; OS & OL, center of L5/S1 disk; PS & PL, posterior disc midpoint; MRI, magnetic resonance imaging.
We investigated the OA to evaluate the natural oblique corridor access angle for the L5/S1 disk space in the lateral decubitus position. This natural corridor angle may be an important surrogate indicator for the angle of orthogonal maneuver that is required to correctly orient the ALIF interbody cage. The OA was measured at a mean of 33° (range, −8° to 45°) from the mid-axis of the disk space. This obliquity in angle is consistent with the described technique of OLIF L5/S1 (Medtronic). In addition, the OA can be used to design a lateral access ATP-specific interbody device that could mitigate the required orthogonal maneuver.
Our study has several limitations. First, there is the known limitation associated with the small sample size. Second, we did not analyze patient demographics and clinical parameters such as body weight and trunk girth to assess their effect on mobilization of the great vessels between positioning. Third, simulating the intraoperative lateral decubitus position in an MRI was challenging, and we may not have achieved the true lateral orthogonal position.
Conclusions
This study demonstrated that the BW of L5/S1 is present within the population group of this study. This BW was mobile and reduced by 20% between the supine and lateral decubitus positioning as the LCIV was brought closer into the field of interest. This result emphasizes that a spine surgeon must consider the increased potential vascular risk during disk access in lateral decubitus ALIF surgery for L5/S1. Moreover, the OA measured in this study was 33° and this parameter should be considered when planning and placing interbody devices, as it may provide guidance regarding potential derotation maneuvers or when centralizing the devices.
Acknowledgements
We would like to thank Dr Bob Dempster for his efforts with this project.
Notes
No potential conflict of interest relevant to this article was reported.
Author Contributions
John Choi: conception and design, drafting of the manuscript, critical revision of the manuscript; Isaac Rhee: acquisition and data, analysis and interpretation of data, statistical analysis; and Sameer Ruparel: acquisition and data.