The Influence of Posture on Instability Evaluation Using Flexion–Extension X-Ray Imaging in Lumbar Spondylolisthesis
Article information
Abstract
Study Design
Prospective clinical study.
Purpose
To determine the optimal posture for instability evaluation using flexion–extension X-ray imaging in patients with lumbar spondylolisthesis.
Overview of Literature
Currently, flexion–extension X-ray imaging is the most practical approach for the evaluation of lumbar instability. In flexion–extension X-ray imaging, achievement of the greatest segmental motion with flexion–extension movement is necessary. However, to our knowledge, currently, there is no standardized posture for determining lumbar instability.
Methods
Twenty-three individuals with lumbar spondylosis related to the fourth vertebra underwent flexion–extension X-ray imaging in different postures (standing, sitting, and lateral decubitus positions), lumbar magnetic resonance imaging (MRI), and low back pain Visual Analog Scale (VAS) evaluation on the same day. Intervertebral angle, percent slippage, and intervertebral disc area ratio for different postures during flexion and extension were compared using Tukey’s method. The effect of low back pain and the association between MRI facet effusion and these measurements were investigated according to posture.
Results
The percent slippage during extension (p=0.036), change in the percent slippage between flexion and extension (p=0.004), and change in the intervertebral angle (p=0.042) were significantly different between the sitting and lateral decubitus positions. There were also significant differences between the standing and lateral decubitus positions in the change in intervertebral angle (p=0.010). In patients with VAS score <40, there were significant differences in the intervertebral angle (p=0.011) between the standing and lateral decubitus positions, percent slippage (p=0.048), and intervertebral disk ratio (p=0.008) between the sitting and lateral decubitus positions. We found no relationship between MRI facet effusion and posture in terms of instability.
Conclusions
In this study, intervertebral instability was best evaluated in the lateral decubitus position when using flexion–extension X-ray imaging for patients with fourth lumbar vertebral spondylolisthesis.
Introduction
Lumbar instability is an important cause of low back pain (LBP) [1]; however, the optimal method to evaluate lumbar instability remain controversial [2,3]. Various methods, such as simple radiography, computed tomography (CT), and magnetic resonance imaging (MRI), have been used to diagnose lumbar instability [4]. During CT and MRI scanning, patients are typically placed in the supine position; however, the narrow space in these devices hampers the functional imaging of the spine [5]. Thus, flexion–extension radiography is currently the most practical approach for the evaluation of lumbar instability.
The use of flexion–extension radiography was first reported by Knutsson [6] in 1944. In this type of imaging, it is necessary to obtain the greatest segmental motion with flexion–extension movement that is improved in the sitting or standing position [6-8]. Wiltse and Hutchinson [8] and Nishimura et al. [5] stated that the functional imaging of the spine should be performed with the patient in the standing position while imaging in the frontal and side views and considering the natural physiological curvature.
In contrast, flexion–extension radiography has been frequently used in the lateral decubitus position [9]. Shigematsu et al. [10] compared the instability determined using flexion–extension radiography between the standing and lateral decubitus positions in patients with fourth lumbar vertebral spondylosis and found that the intervertebral angle during flexion was significantly decreased in the lateral decubitus position. However, they only investigated few cases, the definition of imaging was ambiguous in their study, and pain during imaging was not considered. Moreover, Nishimura et al. [5] reported that in lumbar spine functional imaging, the lateral decubitus position during flexion and the standing and lateral decubitus positions during extension were optimal. Nevertheless, their study involved healthy individuals rather than patients with unstable lumbar spondylosis.
Recently, it has been reported that “facet effusion” in lumbar MRI correlates with lumbar instability [11]; however, the correlation between this feature and flexion–extension radiography-based instability measurements remains unclear.
In this study, we investigated whether posture (standing, sitting, and lateral decubitus positions) during flexion-extension radiography affects the instability assessment; whether LBP affects instability assessment on flexion–extension X-ray imaging, and whether facet effusion on MRI correlates with flexion–extension radiography findings.
Materials and Methods
1. Participants
This study was approved by the appropriate institutional ethics committee in Uda City Hospital (approval no., 001) and conducted as per the principles of the Helsinki Declaration. Informed consent was obtained from each participant.
We enrolled spondylolisthesis patients who visited the orthopedic outpatient department of Uda City Hospital with the main complaint of LBP or lower extremity pain between April 2016 and June 2017. Male and female patients with mild scoliosis or spondylolisthesis were included. Age was not considered for study inclusion. The exclusion criteria were as follows: a history of lumbar surgery, trauma involving spinal vertebral fractures, slips at levels other than the lumbar vertebrae, scoliosis with a Cobb angle of >10° [12], and rheumatoid arthritis.
2. Imaging
Flexion and extension radiography images were obtained in the standing, sitting, and lateral decubitus positions. We instructed the patients to fix their pelvis as much as possible during the imaging procedure (Fig. 1). In the standing position, while keeping the lower limb stretched, the patients held a rod at the ventral side on the anterior superior iliac spine during flexion and held the rod at the dorsal side on the sacroiliac joint during extension. Moreover, in the sitting position, while bending the hip and knee joints at an angle of about 90°, the patients had a cushion on the ventral side during flexion and on the dorsal side during extension. While in the lateral decubitus position, the patients bent their lower limbs as far as possible for imaging during flexion and extended their lower limbs as much as possible for imaging during extension. The distance from the radiography source was standardized to 140 cm [10].

Postures used during imaging. (A) Standing position. (B) Sitting position. (C) Lateral decubitus position.
We evaluated LBP using a Visual Analog Scale (VAS), the LBP VAS, while imaging the flexion–extension radiography images. We recorded a VAS score of 0 when the patient experienced no pain and 100 when he/she reported maximum pain. We also performed lumbar MRI to confirm the presence of facet effusion on the same day as the radiography.
3. Measurements
On the basis of the radiography images, the following items were evaluated for flexion and extension in the three postures: (1) intervertebral angle, (2) percent slippage, and (3) intervertebral disc area ratio (Fig. 2). We evaluated the latter ratio to eliminate the influence owing to the enlargement of radiographs [10]. Thereafter, we compared the measured values of each of the three items in flexion and extension among the three postures (standing, sitting, and lateral decubitus position). We also compared the differences between the values measured in flexion and extension in the three postures.
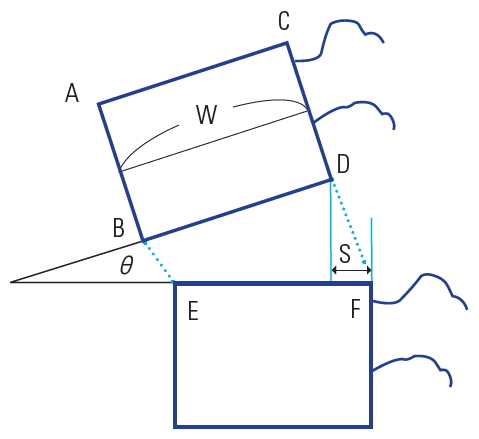
Evaluation items were intervertebral angle; % slippage; intervertebral disc area ratio in flexion–extension X-ray imaging. Intervertebral angle: θ; % slip: S/W×100; intervertebral disc area ratio: BDEF/ABCD×100. % Slip: percentage of the slip distance to longitudinal diameter of the vertebral body; intervertebral disc area ratio: ratio of area of sliding intervertebral disc to sliding vertebra.
The patients were divided into the following two groups: those with LBP VAS scores above the mean (≥40) and those with scores below the mean (<40) [13]. Subsequently, we compared the change in the intervertebral angle, percent slippage, and intervertebral disc area ratio between these two groups to assess whether LBP affected the instability measurements according to posture.
Our studies focused on the L4/5 facet joint. Facet effusion was defined as edema in the L4/5 facet joint on the lumbar MRI [14]. To investigate the relationship between instability as per the imaging position and facet effusion, we divided the patients into the following two groups as those with and those without L4/5 facet effusion on MRI.
4. Statistical analysis
Data were statistically compared using analysis of variance and Tukey’s honestly significant difference test for performing multiple comparisons between the postures. All the statistical analyses were performed using IBM SPSS software ver. 24.0 (IBM Corp., Armonk, NY, USA), and a p-value of <0.05 was considered to indicate statistical significance.
Results
From April 2016 to June 2017, 229 patients with fourth lumbar vertebral spondylolisthesis visited the orthopedic surgeon at our hospital. Patients with a history of lumbar surgery (n=14); those with trauma, including spinal vertebral bone fracture (n=50), those with slips at other than at the fourth lumbar vertebral level (n=17), and those with a Cobb angle >10° (n=58) were excluded [12]. No patients had rheumatoid arthritis. Of the remaining 90 patients, 67 were unveiling to participate in the study. Finally, 23 patients (six men and 17 women; mean age, 70 years; range, 43–87 years) were enrolled. The surveyed patient symptoms included LBP and lower extremity pain. All the patients complained of lower limb pain, and all except one also complained of back pain. One patient had a pacemaker installed, and therefore could not undergo MRI; in another patient, the LBP VAS score was not determined.
1. Instability measurements according to the posture
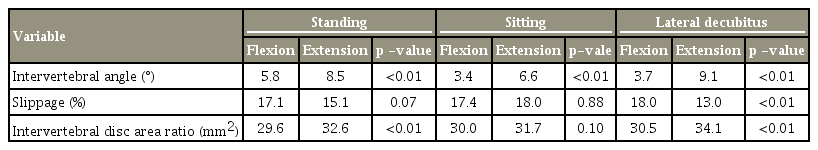
We first compared the instability measurements according to the posture. The data of 23 patients were evaluated and are summarized in Table 1. There was a significant difference in the percent slippage during extension between the sitting and the lateral decubitus positions (sitting 18.0% versus lateral decubitus 13.0%, p=0.036); however, no significant difference was observed among the postures for the other measured parameters.
2. Instability parameter changes between flexion and extension according to the posture
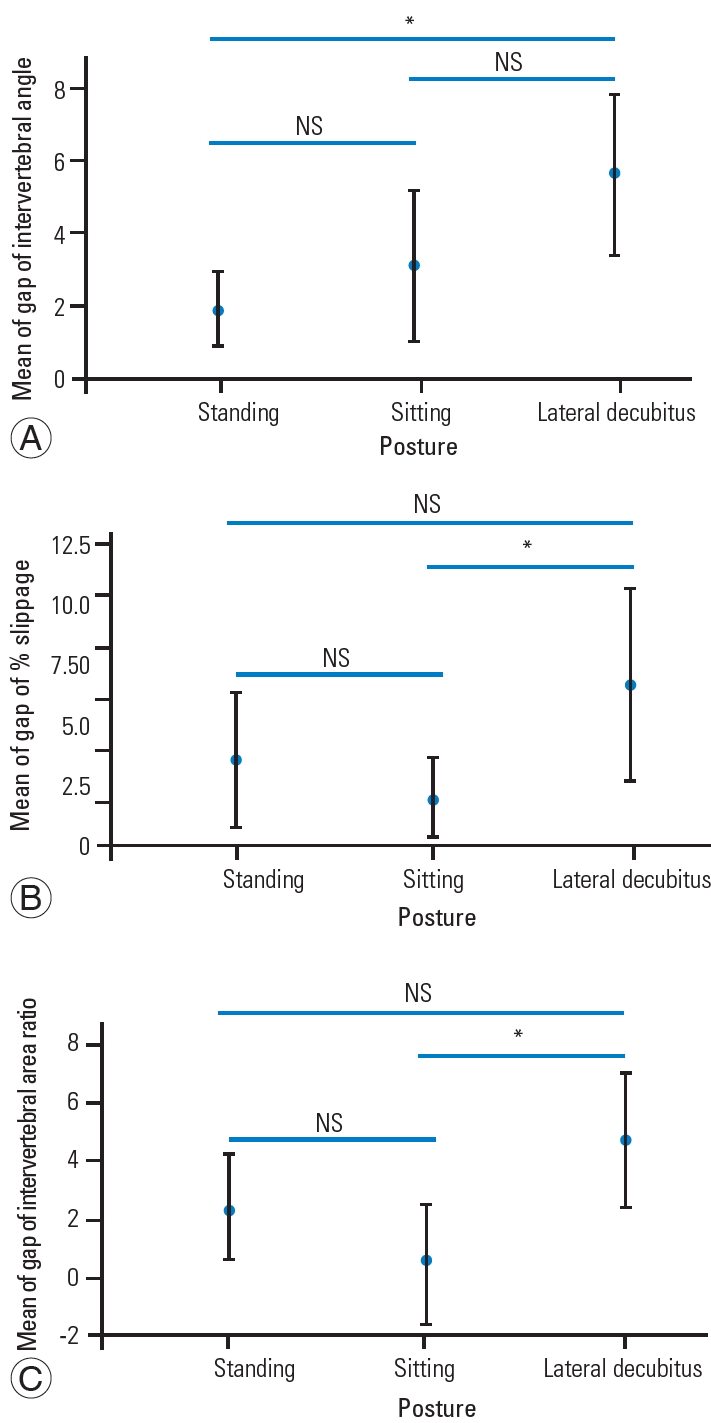
As the next step, we compared the instability among the three postures in terms of the differences between flexion and extension (Fig. 3).
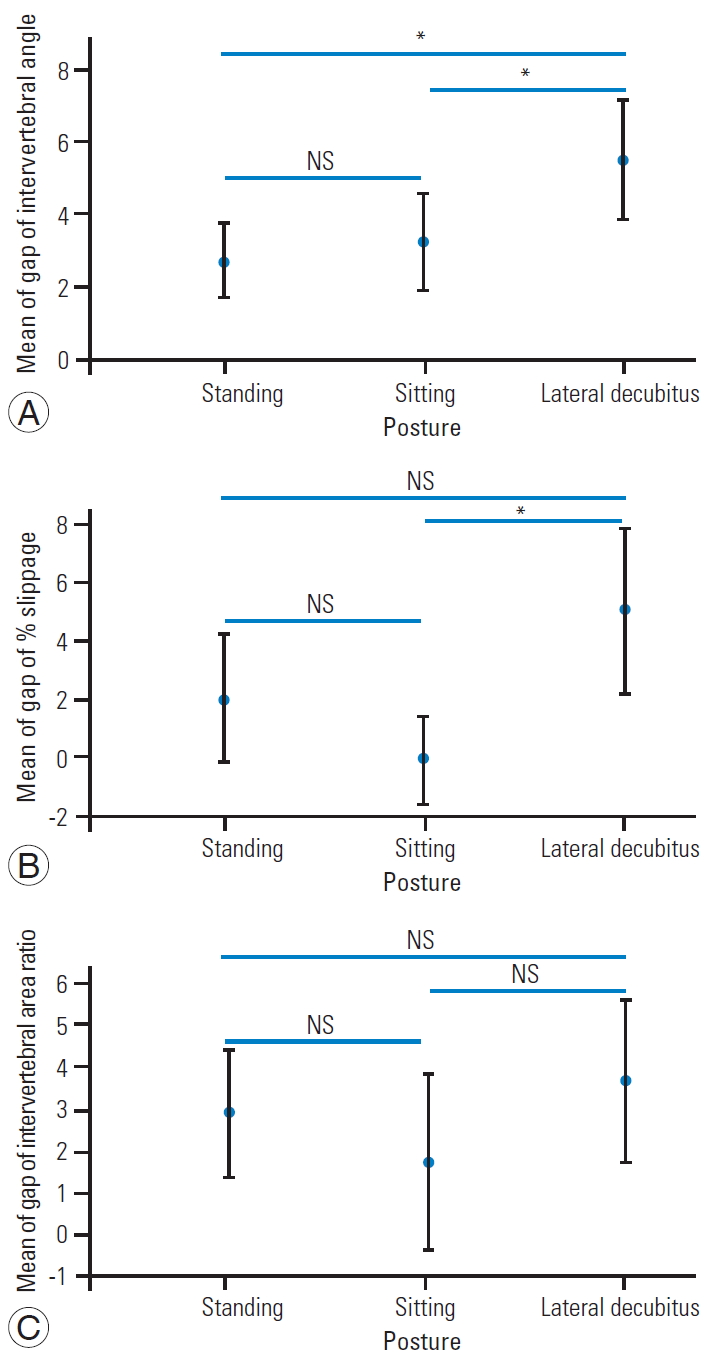
(A–C) Comparison of the instability among postures in the change between flexion and extension position. NS, not significant. *p<0.05.
1) Intervertebral angle
There was a significant difference in the change in the intervertebral angle between flexion and extension in the standing and the lateral decubitus positions (standing 2.7° versus lateral decubitus 5.4°, p=0.010), as well in the sitting and the lateral decubitus positions (sitting 3.2° versus lateral decubitus 5.4°, p=0.042). The greatest difference in the intervertebral angle between flexion and extension was noted in the lateral decubitus position.
2) Percent slippage
There was a significant difference in the change in the percent slippage between flexion and extension in the sitting and the lateral decubitus positions (sitting -1.2% versus lateral decubitus 5.0%, p=0.004). In contrast, the change in the percent slippage was not significantly different between the standing and the sitting positions or between the standing and lateral decubitus positions. The greatest change in the percent slippage between flexion and extension was observed in the lateral decubitus position.
3) Intervertebral disc area ratio
There was no significant difference in the change in the intervertebral disc area ratio between flexion and extension among the three postures.
3. Effect of low back pain Visual Analog Scale on instability measurements according to the posture
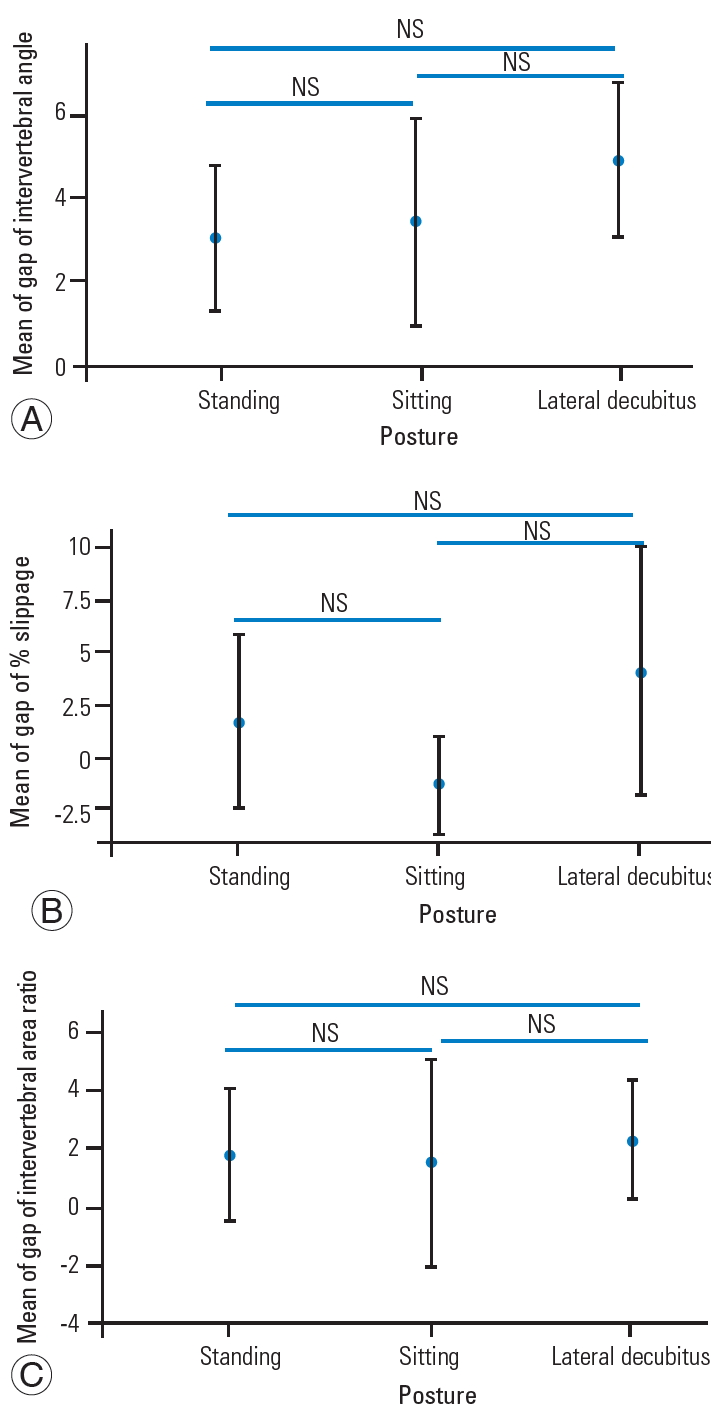
We then compared the instability among the three postures according to LBP, as defined by the LBP VAS score. Among the patients (8/22, 36%) with a LBP VAS score ≥40, there was no significant difference in any parameter among the three postures. In contrast, among the patients (12/22, 64%) with a LBP VAS <40 (Fig. 4), there was a significant difference in the change of the intervertebral angle between the standing and the lateral decubitus positions (standing 1.9° versus lateral decubitus 5.6°, p=0.011). Additionally, there was a significant difference in the change in percent slippage between the sitting and the lateral decubitus positions (sitting 0.20% versus lateral decubitus 5.7%, p=0.048). Furthermore, there was a significant difference in the change in the intervertebral disc area ratio between the sitting and the lateral decubitus positions (sitting 0.52 mm2 versus lateral decubitus 4.8 mm2, p=0.008).
4. Magnetic resonance imaging facet effusion and instability parameters in flexion–extension radiography
Next, we investigated the relationship between MRI facet effusion and flexion–extension radiography. Edema formation on the L 4/5 facet was defined as positive for effusion on the right, left, or both the sides. As one of the 23 patients had a pacemaker, the other 22 patients underwent MRI; of these, 45% were positive for facet effusion. Our analyses revealed no significant difference between MRI facet effusion and posture in terms of instability (Fig. 5).
Discussion
Flexion–extension radiography is crucial in the evaluation of the presence or absence of instability in lumbar degenerative spondylolisthesis; however, currently, to our knowledge, there is standardized posture for use during flexion–extension radiography. Thus, in this study, we investigated the optimal posture for instability evaluation with flexion–extension radiography in patients with lumbar spondylolisthesis. We found that intervertebral instability could be best evaluated with the patients in the lateral decubitus position when using flexion–extension radiography.
While performing flexion–extension radiography, it is crucial to obtain the greatest segmental motion with flexion–extension movement. Wiltse and Hutchinson [8] and Nishimura et al. [5] stated that patients should be in the standing position for flexion–extension radiography. Lowe et al. [15] reported a 26% increase in slippage in the standing position than that in the lateral decubitus position during flexion–extension radiography; however, the sitting and the lateral decubitus positions have also been used in flexion–extension radiography. In this study, we performed imaging using the following three postures: standing, sitting, and the lateral decubitus position. The difference in the segmental motion between flexion and extension was the largest in the lateral decubitus position. In 1994, Wood et al. [9] reported that during flexion–extension radiography in the lateral decubitus position, the largest segmental movement could be obtained, without significant patient discomfort [9]. Shigematsu et al. [10] and Nishimura et al. [5] reported that the dynamic motion in the lateral decubitus position resulted in greater slipping segmental motion. These findings are in agreement with those reported in the present study.
Thus far, there have been no reports on the relationship between pain and imaging posture for lumbar instability. Therefore, we examined the influence of LBP, as assessed by the LBP VAS score, on the instability measurements relative to the posture. These studies revealed no significant difference in the measurements among the three postures in patients with a LBP VAS score ≥40. In contrast, in patients with a LBP VAS score <40, significant differences were found in the parameters between the standing and the lateral decubitus positions and between the sitting and lateral decubitus positions. These findings indicate that patients cannot perform flexion and extension movement well in the presence of severe LBP; the segmental movement is therefore smaller, resulting in a lack of differences among the postures. In contrast, patients with mild LBP can perform the flexion and extension movements with greater ease because this motion is less likely to be hindered by pain. The increased segmental movement causes a significant influence of posture on measurements. The effect is greatest in the degree of sliding in the lateral decubitus position during flexion–extension radiography and in the actual clinical setting; we believe that this position must be more useful than the standing and the sitting positions. As mentioned above, patients with severe LBP could not fully perform the flexion and extension movements; thus, their actual instability may have been underestimated. In spondylolisthesis patients with less instability, the results of posterior decompression are good; however, in those with more instability, the results are more likely to be poor, and several reports have suggested that the addition of a fusion procedure provided good results [16,17]. In other words, underestimation of the intervertebral instability may result in poor postoperative results. Therefore, it is important to preoperatively evaluate instability and believe that this finding is clinically important and should be noted by spine surgeons.
The relationship between MRI facet effusion and instability measurements according to posture was evaluated because MRI facet effusion and lumbar instability are reported to be related [11,18]. Hasegawa et al. [14] stated that an increased facet joint volume indicates spinal instability in the degenerative lumbar spine. Lattig et al. [19] and Oishi et al. [20] measured the greatest distance between the apparent articular surfaces to determine facet effusion size. Lattig et al. [19] found that, in general, mean effusions >1.77 mm on either side were associated with instability, whereas Oishi et al. [20] found unstable motion in patients with effusion sizes >1.3 mm. Furthermore, Lattig et al. [19] stated that the extent of the left/right difference in effusion was associated with the presence of rotational translation. In this study, MRI facet effusion positivity was examined in all three postures; however, there was no significant difference among the postures.
Finally, although the definition of instability in lumbar spondylolisthesis patients in the standing posture has previously been reported [3,21-26], the amount of change in the lateral decubitus position during flexion–extension imaging requires further assessment. Some researchers have considered >3 mm slippage in a neutral position, >3 mm translation, and >10° angulation as indicative of excessive motion (instability) [3,21,27]. However, others have considered a change of >10° in the disc angle or a change of >3 mm in translation in the standing or lateral decubitus radiographs as a sign of instability [22-26]. A combination of >3 mm slippage and >3 mm translation was associated with severe symptoms and is considered to indicate surgery [21]. These definitions of instability have often been reported during standing radiography procedures. In clinical practice, during imaging in the standing position, and particularly when performing whole-spinal column imaging, it is essential to consider lumbar fixation surgery in procedure selection.
A main limitation of the current study is the relatively small sample size. However, it might be difficult to enroll more patients because of the study design that includes radiation exposure. Second, although many reports have indicated an association between lumbar instability in patients with lumbar degenerative spondylolisthesis and MRI facet effusion [11,18], we found no association between MRI facet effusion and instability measurements according to the posture. This lack of association may be related to our sample size. Third, we only focused on four spondylolisthesis cases in this study because uniform evaluation was considered necessary. In clinical settings, the fourth vertebra was the level that was most frequently affected by spondylolisthesis [28,29]. Therefore, we do not know whether other vertebral levels with spondylolisthesis show the same phenomenon.
Conclusions
To our knowledge, no standardized posture for determining lumbar instability has been established. The results of the present study emphasize the value of performing imaging in the lateral decubitus position. This position is useful for flexion–extension radiography in patients with mild LBP. Lumbar instability cannot be adequately assessed in patients with severe LBP, and instability will be underestimated. New definitions of instability for imaging in the lateral decubitus position, rather than those used for imaging in the standing position, need to be designed for application in the clinical setting.
Notes
No potential conflict of interest relevant to this article was reported.
Author Contributions
Dr. Takeshima conceived and designed the study and was involved in data acquisition. Dr. Shigematsu, Dr. Nakagawa, and Prof. Tanaka provided critical revision and supervision for the manuscript. All authors discussed the results and contributed to the final manuscript.
Acknowledgements
The authors thank Nahoko Morimoto, Shizuka Okuda, Yuka Yamane, Takehiro Yoshioka, Kouji Yamamoto, Mitsuo Matsumoto, Ryo Takada, Masanori Yoshimura, Takao Konishi, and Toshihumi Takashima for their technical assistance with the flexion-extension X-ray imaging.