Proximal Junctional Kyphosis: Diagnosis, Pathogenesis, and Treatment
Article information
Abstract
Proximal junctional kyphosis (PJK) is a common radiographic finding after long spinal fusion. A number of studies on the causes, risk factors, prevention, and treatment of PJK have been conducted. However, no clear definition of PJK has been established. In this paper, we aimed to clarify the diagnosis, prevention, and treatment of PJK by reviewing relevant papers that have been published to date. A literature search was conducted on PubMed using "proximal junctional", "proximal junctional kyphosis", and "proximal junctional failure" as search keywords. Only studies that were published in English were included in this study. The incidence of PJK ranges from 5% to 46%, and it has been reported that 66% of cases occur 3 months after surgery and approximately 80% occur within 18 months. A number of studies have reported that there is no significantly different clinical outcome between PJK patients and non-PJK patients. One study showed that PJK patients expressed more pain than non-PJK patients. However, recent studies focused on proximal junctional failure (PJF), which is accepted as a severe form of PJK. PJF showed significant adverse impact in clinical aspect such as pain, neurologic deficit, ambulatory difficulties, and social isolation. Numerous previous studies have identified various risk factors and reported on the treatment and prevention of PJK. Based on these studies, we determined the clinical significance and impact of PJK. In addition, it is important to find a strategic approach to the proper treatment of PJK.
Introduction
Proximal junctional kyphosis (PJK) has become the greatest challenge in surgery for spinal deformity. PJK is detected by radiologic findings indicating that a pathologic problem has developed internally around the adjacent segment after a spinal fusion. PJK is not an instantaneous symptom but is considered one of various ongoing adjacent segmental problems. Some PJK patients may display no symptoms whereas others, referred to as proximal junctional failure (PJF) patients, express clinical symptoms accompanied by pain, walking disturbance, and neurologic deficit, and reoperation may be required in some severe cases [1]. Spine specialists have suggested various explanations to understand these cases of PJK. In this review, we compare and summarize the diagnosis, incidence, pathogenesis, and treatment of PJK from review of current literature, with the aim of proposing a new direction for further research into PJK.
Discussion
The authors searched papers published up to July 2015 using the PubMed databases with "proximal junctional", "proximal junctional kyphosis", and "proximal junctional failure" as the search keywords.
A total of 594 papers were found on PubMed, excluding non-English language papers and duplicated papers. This number includes only papers that discussed the incidence, definition, risk factors, treatment, and prevention of PJK. Based on this finding, 40 articles were included in this review.
1. Definition
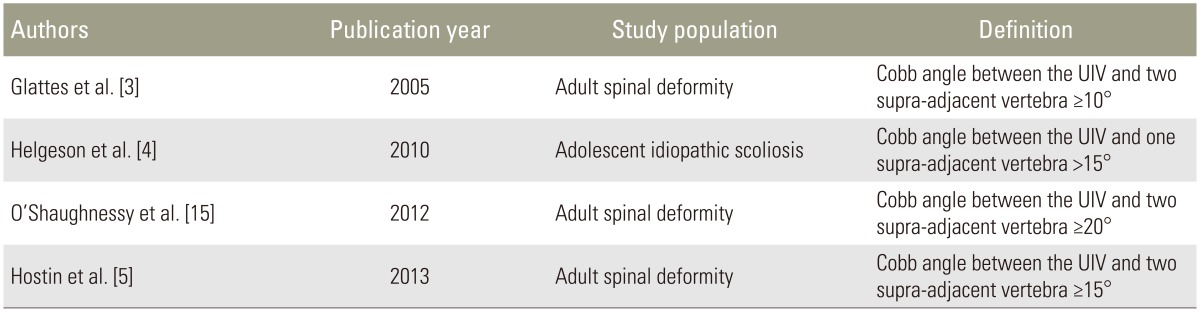
In order to diagnose PJK, a proper working definition of PJK should first be established. As suggested by the terminology, an abnormal kyphotic deformity occurs at the uppermost instrumented vertebra (UIV), a finding that was observed systematically and reported for the first time by Lee et al. [2], who defined a case of PJK as "a patient with adolescent idiopathic scoliosis having kyphosis 5 degrees higher than normal at the proximal level of the instrumented fusion" after conducting posterior spinal fusion. However, the various definitions of PJK have not yet been integrated, and PJK continues to be defined in a variety of ways.
Glattes et al. [3] defined PJK as a case "showing a proximal junctional sagittal Cobb angle—which is composed of the lower endplate of the uppermost instrumented vertebra (UIV) and the upper endplate of the two supra-adjacent vertebrae—some 10 degrees higher than a preoperative measurement."
Helgeson et al. [4] claimed that more than 15 degrees of abnormal kyphotic angulation should occur when PJK is measured at one adjacent vertebra above the UIV. These authors suggested that conventional measurement at two adjacent vertebrae above the UIV does not reflect a physiological basis, and disruption of the facet capsule and interspinous ligament were considered to be the causes of PJK.
However, Hostin et al. [5] defined PJK as "showing more than 15 degrees of angulation at two supra-adjacent vertebrae above the UIV" based on the results of a large multicenter and retrospective study. In addition, in many other papers, PJK has been defined as a case "showing more than 15 degrees of Cobb angle at two adjacent vertebrae above the UIV" [67891011121314]. Furthermore, O'Shaughnessy et al. [15] and Bridwell et al. [16] defined PJK as a case "showing more than 20 degrees of Cobb angle at two levels above the UIV." In particular, Bridwell et al. [16] argued that more than 20 degrees is not a standard for revision surgery of PJK, although it can be a critical cutoff value as a threshold for worse patient-reported outcomes.
Sacramento-Dominguez et al. [17] performed 152 measurements in 19 scoliosis patients and compared the reproducibility of the PJK angle at one level and two levels above the UIV. To validate the result of each measurement, the intra-surgeon concordance correlation coefficient ranged from 0.78 to 0.92, which showed a very high degree of reproducibility, while the inter-concordance correlation coefficient ranged from 0.55 to 0.80, showing a moderate to high degree of reproducibility. Both one level and two levels showed a positive result for reproducibility. To summarize the abovementioned findings, there is no clear definition of PJK, but based on previous studies PJK can be categorized into four classes and clinical PJK can be diagnosed based on these definitions (Table 1).
2. Pathogenesis and risk factors
The pathogenesis of PJK has yet to be established. Suggested mechanisms include the following: (1) extensive paraspinal muscle dissection at the upper instrumented vertebra, (2) disruption of the supraspinous and interspinous ligaments (posterior tension band), (3) improper end-vertebra selection, (4) proximal severe disc degeneration, (5) compression fracture at the most instrumented vertebra, (6) instrumentation failure at the proximal construct, and (7) facet violation [318]. In addition, many studies have investigated the risk factors of PJK in order to better understand the pathogenesis of PJK.
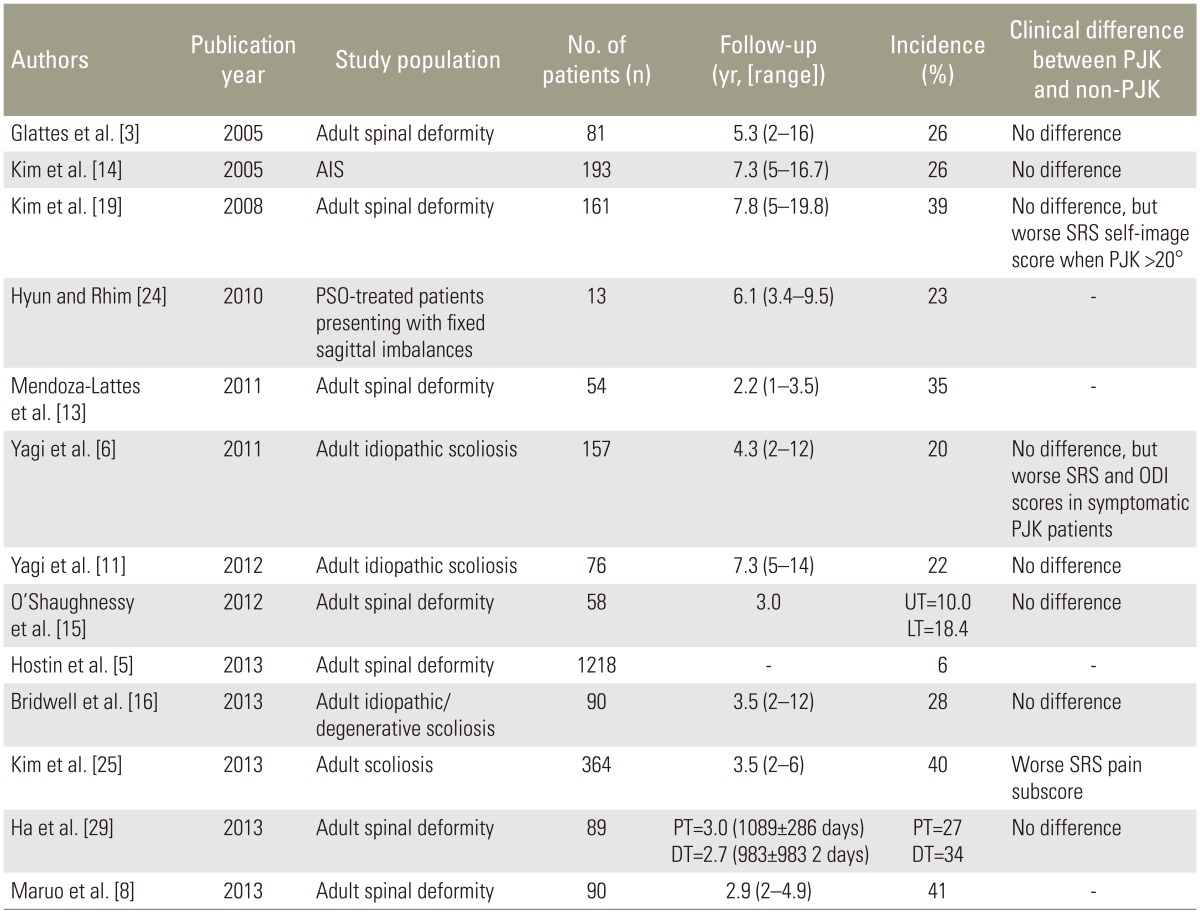
The following major risk factors for PJK have been suggested: older age (>55 years) [161920]; large abnormal preoperative sagittal parameters [26810111214]; the use of pedicle screws [410121421]; thoracoplasty procedures [101214]; greater curvature correction [812162022]; posterior and anterior-posterior spinal fusion (i.e., disruption of the posterior tension band/posterior intervertebral elements) [6911161921]; and fusion to the lower lumbar spine and sacrum [6910111315]. In addition, low bone marrow density [11] and a patient's comorbidity and high body mass index [16] are discussed as potential risk factors (Table 2). However, clear evidence supporting the number of instrumented levels and the UIV level, which are regarded as the strongest influences, is not yet available [9141623].
3. Incidence
Hostin et al. [5] reported an incidence of PJK of 6%, Yagi et al. [6] reported an incidence of 20% among adult scoliosis patients, Kim et al. [19] reported an incidence of 39% after 7.8 years of follow-up, and Maruo et al. [8] reported an incidence of 41%. The reported incidence in all reports ranges from 6% to 41% (Table 2). The incidence of PJK also varies depending on the level of UIV. O'Shaughnessy et al. [15] reported a lower thoracic incidence of 18.4% and upper thoracic incidence of 10%.
PJK tends to appear shortly after an operation. Kim et al. [19] suggested that PJK appears within 8 weeks of surgery, whereas Yagi et al. [11] reported that 66% of PJK cases appeared within 3 months and Wang et al. [10] stated that 80% of cases of PJK could be diagnosed within 18 months.
4. Clinical appearance and severity
PJK can present in a spectrum from simple radiologic findings to symptoms with a significant clinical impact. Numerous studies on the differences between cases of PJK that are clinically obvious and cases with only radiological findings have been conducted.
Several studies have reported that there are no significant differences in Scoliosis Research Society scores and clinical symptoms between non-PJK patients and PJK patients [361424]. In contrast to these results, Kim et al. [25] performed a large-scale study in which they analyzed 364 patients. The PJK patient group showed a significantly higher incidence of pain, with pain prevalent in 29.4% of the PJK patient group compared with only 0.9% of the non-PJK patient group. In particular, the presence of pain in the upper back was higher among PJK patients with a 12.5-fold odds ratio. Regarding this issue, Hart et al. [7] reported that PJK appears within a spectrum of disease severities from benign PJK without clinical impact to PJF, which eventually has significant adverse impact, and that 47.4% of patients with PJF underwent revision surgery.
In several studies, PJF is reported as one entity in the disease spectrum of PJK that includes kyphosis and structural failure of the body and the posterior ligament complex [2627]. As such, PJF patients may experience pain, neurologic deficit, ambulatory difficulties, social isolation, and/or inability to maintain a horizontal gaze [1111925]. Smith et al. [28] suggested that it was necessary to pay special attention to PJF, which is crucial from the clinical perspective because adult patients with spinal deformity tend to have long constructs, but do not necessarily exhibit worse clinical outcomes.
In particular, fracture, implant failure, and myelopathy due to stenosis at the UIV or UIV+1 that appears within 6 months of an early proximal junctional failure (EPFJ) were defined [28]. The authors reported a 25% higher incidence of EPFJ, which appeared most commonly at the lower thoracic spine level and was not related to postoperative sagittal balance.
5. Prevention
Even more important than treatment is the prevention of PJK. In order to prevent PJK, the risk factors should be sufficiently considered before surgery. Above all, the sagittal alignment of a patient should be checked, and then the proper revision should be conducted by osteotomy depending on the flexibility or rigidity of the patient's deformity. At this point, the UIV level should be set with neutral and stable vertebra in order to reduce the prevalence of revision for patients with adult deformity [30]. Making a decision on the UIV level, however, is not as simple as it sounds. If the UIV is decided at T8 or a lower level for shorter fusions, the prevalence of PJK might be increased [15163132], whereas increasing the fusion level to the proximal level in order to prevent simple PJK could lead to perioperative complications, which could in turn cause other problems. Some studies have reported that pedicle screws increase the possibility of facet violation and the creation of a rigid construct, such that long-segment instrumentation using pedicle screws might increase the prevalence of PJK.
Helgeson et al. [4] compared the prevalence of PJK in a multicenter retrospective study. The authors compared the four groups of hook-only constructs, hybrid constructs (pedicle screws and hooks), pedicle-screw only constructs, and pedicle-screw constructs with hooks only at the most cephalic level during a 2-year follow-up, and reported that the most significant increase in PJK was observed in the group of pedicle-only constructs.
As a preventive measure, various trials to reduce the prevalence of PJK using hooks have been reported. Hassanzadeh et al. [33] used transverse process hook and pedicle screws at the UIV for patients who had already undergone more than five levels of instrumentation surgeries. After a 2-year follow-up, 29.6% of the group with pedicle screws showed symptoms of PJK, but no cases of PJK were observed in the patient group with hooks. Kim et al. [12] also reported a lower prevalence of PJK in cases where hooks rather than only pedicle screws were used.
Regarding decisions on the lowest instrumented vertebra (LIV), various factors should be considered. Some studies have argued that fusion of the sacrum is a risk factor [6910111315] and that sufficient consideration when deciding on fusion at a lower level is required. However, it must be remembered that if L5 is decided as the LIV, degeneration of the L5–S1 disc will progress and thus a revision operation may be required [34].
In addition, damage to parts of the posterior column such as the facet joint capsule or interspinous ligament during the operation must be minimized to allow it to function as a posterior tension band [21]. In the case of the osteoporotic bone, the development of not only PJK, but also of PJF, could occur because of the prevalence of compression fractures and loosening of the pedicle screw at the UIV. Therefore, prevention of PJK through osteoporosis treatment should be considered. However, the use of bisphosphonate in spinal fusion remains controversial [35], and instead the improvement in bone quality and effective establishment of bone union could be implemented using teriparatide [3637].
Hart et al. [27] reported that use of vertebroplasty at the UIV is effective in preventing compression fractures. In their study, 15 of 28 women older than 60 years were operated on with cement augmentation, whereas the remaining 13 women were not treated; none of the former group showed signs of PJK, whereas 15.3% of the latter group displayed secondary PJK due to collapse of the vertebral body. Moreover, in their biomechanical cadaveric study, Kebaish et al. [38] reported preventive effects when they conducted vertebroplasty at both the UIV and one higher level of vertebrae. However, cement may change the load transfer and ultimately lead to the fracture and collapse of adjacent vertebrae [26]. Although these are simple case reports, it should be noted that there are also reports warning of further severe fracture with augmentation at the UIV [39].
6. Treatment
PJK is a simple radiologic finding and a continuously progressive disease. If it develops as symptomatic PJK it appears as a type of PJF. There are no evidence-based guidelines on the treatment of PJK. Once a patient has a problem around the proximal junction, evaluating the existence of clinical symptoms should be prioritized. If there are no symptoms prompt treatment is not required in most cases, but if severe symptoms exist or a deformity of the proximal junction progresses rapidly surgical treatment will be required. Hart et al. [7] suggested more specific decision-making criteria for surgery. Based on their research on 57 PJF patients, they reported the factors that most influenced PJF revision surgery were high PJK angulation, high sagittal vertical axis, trauma, and female gender. However, other commonly considered factors including soft tissue versus bony failure, patient age, level of fusion, and upper thoracic versus thoracolumbar proximal junction showed no correlation. When conducting surgical treatment, a neural decompression procedure with process of extending and realigning the instrumentation is required in most cases. If the spine is flexible, a stable level should be found at the proximal level of the UIV from a previous surgery. If the spine is rigid, the global sagittal alignment should be revised using a method of osteotomy, such as Smith-Peterson osteotomy or pedicle subtraction osteotomy. Above all, an entire spine lateral radiograph from a standing position should be taken and the fundamental causes of the problem should be determined in order to prevent any further occurrence.
Conclusions
The development of implants for spinal surgery has allowed multilevel spinal instrumentation. As a result, PJK, as one of the related complications, has received attention in recent years. The increased interest of spine surgeons in PJK has resulted in a number of research papers, and the epidemiology and risk factors associated with PJK have become known through these studies. Despite the high prevalence of PJK, a collective definition of PJK has not yet been clearly established, and further research needs to be conducted. In addition, a standardized consensus concerning the pros and cons of operating on PJK patients is required. Even though a number of studies on PJK have been conducted [40], spine surgeons continue to hold different opinions and perspectives about the treatment of PJK. Finally, further PJK guidelines and a standard classification that not only include symptoms, radiologic findings, pathogenesis, severity of PJK, treatment, and prognosis, but are also easy to understand and apply to PJK treatment, need to be elaborated.
Summary
· A clear definition of PJK has not been established, but it is mostly defined as a Cobb angle between the UIV and two supra-adjacent vertebra ≥10°–20°.
· In reported cases, the incidence of PJK ranged from 6% to 41%, and it was observed to appear shortly after an operation.
· PJK is a progressive type of disease that develops from a simple radiologic finding into symptomatic PJK, which appears in the form of PJF that might have a catastrophic outcome.
· The risk factors for PJK are well known and acknowledged. Based on this knowledge, a precise preoperative plan should be established in order to prevent PJK.
· A standardized consensus for further understanding and treatment of PJK is required.
Notes
Conflict of Interest: No potential conflicts of interest relevant to this article are reported.