|
 |
- Search
| Asian Spine J > Volume 15(2); 2021 > Article |
|
Abstract
Overview of Literature
It is known that two fused vertebral bodies take the similar shape of the single body with inwaisting, with or without caudal flaring of the fused body, and that the fused body can cause the fusion disease at the adjacent segment that can be a risk factor for potential neurological compromise.
Methods
Radiograms of the 11 study subjects (six men and five women), aged 22ŌĆō90 years who visited the outpatientsŌĆÖ clinic for various neck complaints without trauma history were examined. C4ŌĆō5 synostosis was an incidental finding in all the subjects.
Results
All the fused bodies were inwaisted and had anterior caudal breaking but no interior corporal flaring. Adjacent segment disease was not found in eight patients aged <40 years. Disk degeneration was found at C3ŌĆō4 and C5ŌĆō6 in three patients each and at C6ŌĆō7 in two patients. Disk degeneration was limited to the adjacent segments.
It is known that block vertebrae of the cervical spine are a rare but well-known condition. Some authors consider congenital cervical block vertebrae as an accidental radiographic finding that is not related to any disease, while others conjecture that the block vertebrae might cause secondary degenerative changes and mobility disturbance of the adjacent segments. Based on this information, we designed the current study. The authors noticed that each motion segmentŌĆÖs response was biomechanically different owing to the differed sagittal alignment at each level, the difference in natural mobility, their bearing load size, and axis [1-3].
The current study is one of the serial study projects at the different fused levels and is to assess the normally aligned C4ŌĆō5 synostosis on the adjacent segment. This is the fourth study by the author of the current study.
Radiographs of 11 patients (six men and five women) aged 22ŌĆō90 years with congenital synostosis of C4ŌĆō5 were investigated (Figs. 1ŌĆō3). All the cases were accidentally while performing diagnosed on radiography (Table 1). Severity of disk degeneration was expressed as follows: normal height as -, narrowing suspected as (┬▒), mild narrowing (<25%) as +, moderate narrowing (50%) as ++, relatively severe narrowing (75%) as +++, and very severe narrowing (over 75%) as ++++.
None of the patients ostensibly showed a short neck. Block vertebral body showed more remarkable inwaisting and anterior inferior corporal lipping. Among eleven patients, only three aged >45 years developed disk narrowing in the two cranial and two caudal adjacent segments (cranial: C2ŌĆō3 and C3ŌĆō4; caudal: C5ŌĆō6 and C6ŌĆō7). The severity of disk degeneration ranged from ┬▒ (suspected early disk degeneration) to +++ (relatively severe disk narrowing). The incidence of age-related (decadal) disk degeneration is shown in Table 2. Only three patients aged >51 years showed disk degeneration. However, only one patient aged >81 years showed relatively severe disk degeneration while two patients aged 56 years and 61 years showed ┬▒ to + degree of degeneration.
There have been numerous reports in the literature suggesting that the congenitally formed block vertebrae of a part of the cervical spine may alter the kinematics and cause extra-stress onto the adjacent non-fused segments, hypothetically resulting in early progressive disk degeneration. Generally, fusion may result in increased intradiskal pressure at the adjacent levels and would impair the nutrition of the disk; however, this interpretation is conflicting. To clarify the issue, the current study investigated the morphology of the fused vertebrae and degeneration of the possible adjacent disk. Leivseth et al. [4] showed that the caudal adjacent disk height of the fused vertebrae was significantly reduced, while the height of the cranial adjacent disk was normal. However, in the current authorsŌĆÖ series, both the cranial and caudal adjacent disks were affected. Thus, the result of the current authorsŌĆÖ study does not accord with the observations of Leivseth et al. [4].
Generally, it has been conjectured that fusion might result in an unphysiological motion pattern of adjacent segments and that the former motion of the fused segment might be transferred to the open cranially or caudally adjoining segments. However, the presented evidence is conflicting, and it is difficult to speculate on the detrimental effect of block vertebra on the adjacent mobile segment because the initial state of the mobile segments adjacent to the block vertebra is unknown.
Why a motion deficit due to fusion must be compensated only for in the adjacent segment instead of all open segments? In none of the subjects, hypermobility was complicated at the adjacent segment in the current authorsŌĆÖ series. In the current series, only three patients (27.3%) aged Ōēź56 years developed spondylosis. Although the current authors cannot discern the contribution of synostosis apart from natural history, our data provide important information regarding adjacent segment disease (ASD).
Fig.┬Ā1.
(AŌĆōF) Lateral radiographs of six patients with congenital C4ŌĆō5 synostosis show the inwaisted fused vertebrae without disc degeneration in any of the adjacent mobile segments. M, male; F, female.
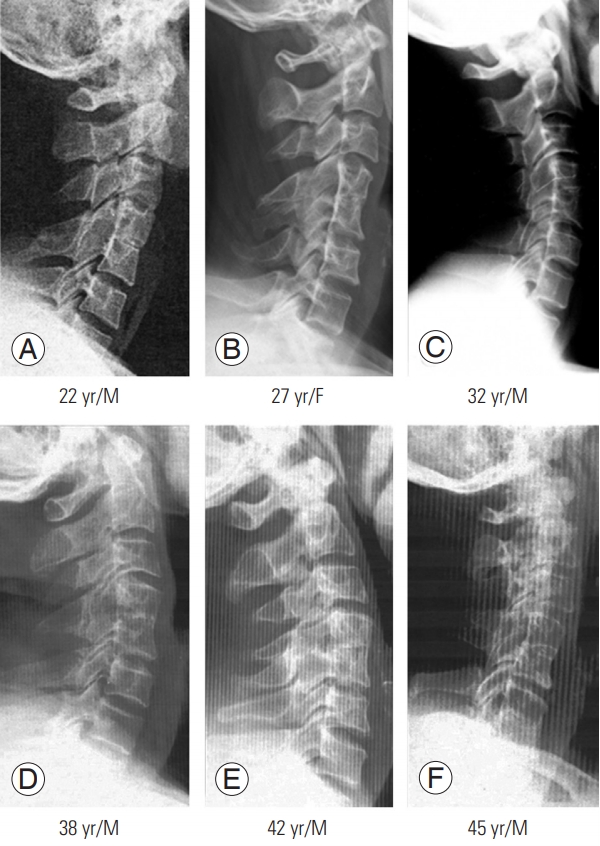
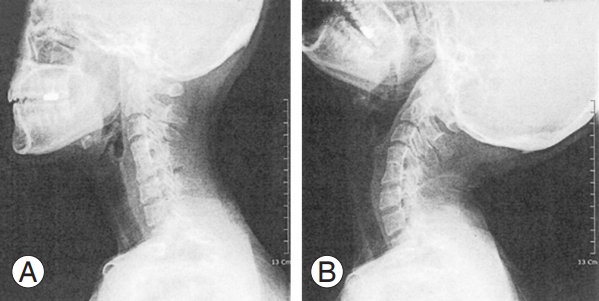
Fig.┬Ā2.
Sagittal radiographs of three patients with congenital C4ŌĆō5 synostosis (AŌĆōC), aged from 56 to 90 years, show slightly inwaisted fused vertebral body and slightly flared lower part of the fused body. But severe spondylotic changes were observed at two proximal and caudate discs, respectively. M, male; F, female.

Table┬Ā1.
Disc conditions of cephalad and caudad levels in patients with congenital C4ŌĆō5 synostosis
Table┬Ā2.
Age-related distribution of the spondylotic mobile segments in 11 patients (six males and five females) with congenital C4ŌĆō5 synostosis
References
1. Moon MS, Moon YW, Kim SS, Moon JL. Morphological adaptation of the bone graft and fused bodies after non-instrumented anterior interbody fusion of the lower cervical spine. J Orthop Surg (Hong Kong) 2006 14:303ŌĆō9.


2. Moon MS, Kim SS, Lee BJ, Moon JL, Lin JF, Moon YW. Radiographic assessment of congenital C2-3 synostosis. J Orthop Surg (Hong Kong) 2010 18:143ŌĆō7.


3. Moon MS, Kim JM. The effect of mechanical forces on vertebral growth: a preliminary report. J West Pac Orthop Assoc 1974 11:1ŌĆō26.