Postoperative Severe Headache Following Cervical Posterior Surgical Fixation from C2 Distally
Article information
Abstract
Study Design
Retrospective study.
Purpose
To identify the prevalence of severe headache occurring after cervical posterior surgical fixation (PSF) and to evaluate the clinical and radiological findings associated with severe headache after surgery.
Overview of Literature
Several studies have reported on the axial pain after cervical surgery. However, to our knowledge, the incidence of severe headache after cervical PSF has not been elucidated.
Methods
The medical records and radiological assessment of patients who underwent surgical treatment from August 2002 to May 2012 were reviewed to identify the prevalence and risk factors for severe headaches occurring following PSF from C2 distally. Neck disability index scores (NDI) (the item for neck pain), the type of C2 screw, number of cervical fused levels (1–6), and smoking habit were calculated preoperatively and postoperatively. In addition, radiological parameters (T1 slope angle, C1/2 angle, C2–7 Cobb angle, C2–7 sagittal vertical axis and C1-implant distance) were assessed for all patients. Severe headache was defined as a high NDI headache score (>4 out of 5).
Results
Eighty-two patients met the inclusion criteria. The mean age was 59.2 years (range, 21–78 years), and the mean number of fused levels was 5.1. The mean follow-up period was 2.9 years (range, 1–10.9 years). While only one severe headache occurred de novo postoperatively in a patient in the C3 or C4 distally group (total 30 patients, average age of 50.2 years), 11 patients in the C2 distally group (p=0.04) had severe headache occur postoperatively. The radiological parameters were not significantly different between the postoperative milder headache and severe headache (SH) groups. The SH group had a significantly higher preoperative NDI score (neck pain) (p<0.01).
Conclusions
Newly occurring severe headaches can occur in 18% of patients after PSF from C2 distally. The patients with newly occurring severe headaches had significantly higher preoperative NDI score (neck pain).
Introduction
Neck pain originates from paraspinal tissue, but chronic neck pain with concomitant headache may have underlying spine pathology, such as cervical degenerative disc disease [1]. Following cervical posterior surgical fixation (PSF) from C2 distally (PSF from C2 distally), we found that some patients began experiencing severe headache, which was not a symptom previously. Other cases had continued headache symptoms or the headache was aggravated after surgery. The factors surrounding the incidence of severe headache after cervical posterior fixation are not clear, and it is unknown whether PSF from C2 distally would be an effective procedure for treating severe headache. In addition, the actual reason for newly occurring severe headache after PSF from C2 distally has been unclear.
The authors hypothesized possible reasons why a severe headache may occur after PSF from C2 distally: (1) the implant may influence the bony structure, (2) severe muscle tension may occur due to the severe forward bending alignment of the head, and (3) C1–C2 hyperlordosis can result in C2 foraminal stenosis when attempting to maintain horizontal gaze. To the best of our knowledge, this is the first study of severe headache occurring after PSF from C2 distally. Its purpose is to identify the prevalence of severe headache occurring after PSF from C2 distally and to evaluate the clinical and radiological findings associated with severe headache after surgery.
Materials and Methods
1. Patient selection and clinical investigation
This study was approved by the Institutional Review Board at Washington University School of Medicine. We performed a retrospective review on both prospectively and retrospectively collected data for this study. The medical records and radiological assessment of patients who underwent surgical treatment from 2002 to 2012 were reviewed to identify the prevalence of and risk factors for severe headache occurring after PSF from C2 distally. Patients with less than one year follow-up, incomplete clinical data and questionnaire or occipito-cervical spontaneous fusion by ankylosing spondylitis were excluded. We also excluded patients from statistical analysis who had postoperative severe headache due to penetration of the C2 screw into the cortex of the C2 pars area directly irritating the C2 nerve root.
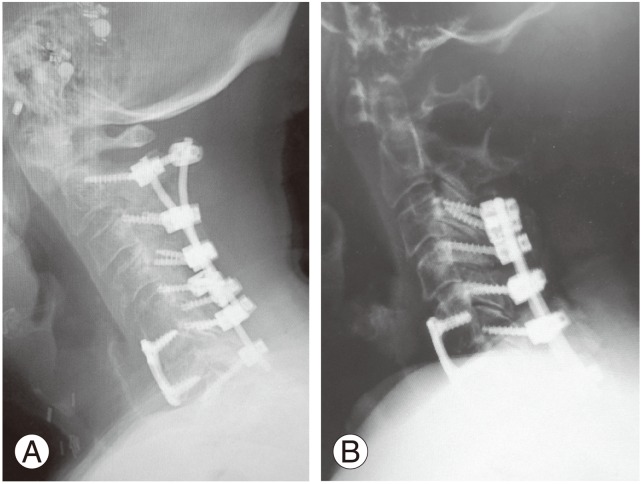
Neck disability index (NDI) scores, the C2 screw type (pedicle screw, pars screw, laminar screw, transarticular screw or combination), cervical fused levels (1–6), and smoking habit were recorded preoperatively and postoperatively. We used the NDI (headache and neck pain items) to assess patients' headache and neck pain. The NDI is a reliable, valid and sensitive instrument for self-reporting measures [2]. It includes a headache severity index, thus, we graded preoperative and postoperative headache as milder headache (grade 0–3) or severe headache (SH) (grade 4 or 5). We also compared SH which first occurred after PSF from C2 distally with SH that occurred after PSF from C3 or C4 distally (30 patients), for which we adopted the same inclusion criteria (Fig. 1).
2. Radiologic evaluation
The following radiological spinal parameters were assessed: (1) T1 slope angle (the angle between a horizontal line and the upper end plate of T1), (2) C1–C2 lordosis angle (the angle of intersection between a line connecting the anterior tubercle to the posterior margin of the C1 spinous process and a line parallel to the inferior end plate of C2), (3) C2–7 Cobb angle, (4) C2–7 sagittal vertical axis (SVA: the distance between the plumb line dropped from the center of C2 and the posterior superior corner of C7) [3] and (5) C1-implant distance (the distance from the most proximal implant to C1 arch on neutral lateral cervical X-ray) (Fig. 2).
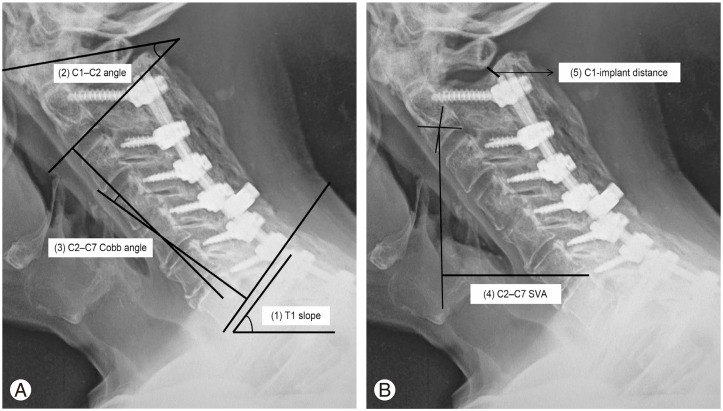
(A) Radiological parameters. (1) T1 slope angle: the angle between a horizontal line and the upper end plate of T1. (2) C1–C2 lordosis angle: the angle of intersection between a line connecting the anterior tubercle to the posterior margin of the C1 spinous process and a line parallel to the inferior end plate of C2. (3) C2–7 Cobb angle. (B) Radiological parameters. (4) C2–7 sagittal vertical axis (SVA): the distance between the plumb line dropped from the center of C2 and the posterior superior corner of C7. (5) C1-implant distance: the distance from the most proximal implant to C1 arch on neutral lateral cervical X-ray.
3. Statistical analysis
Data were analyzed using SPSS ver. 20.0 (IBM Co., Somers, NY, USA). We used Mann-Whitney U-tests for non-normally-distributed variables and chi-square tests for categorical variables. The threshold for significance was a p-value of <0.05.
Results
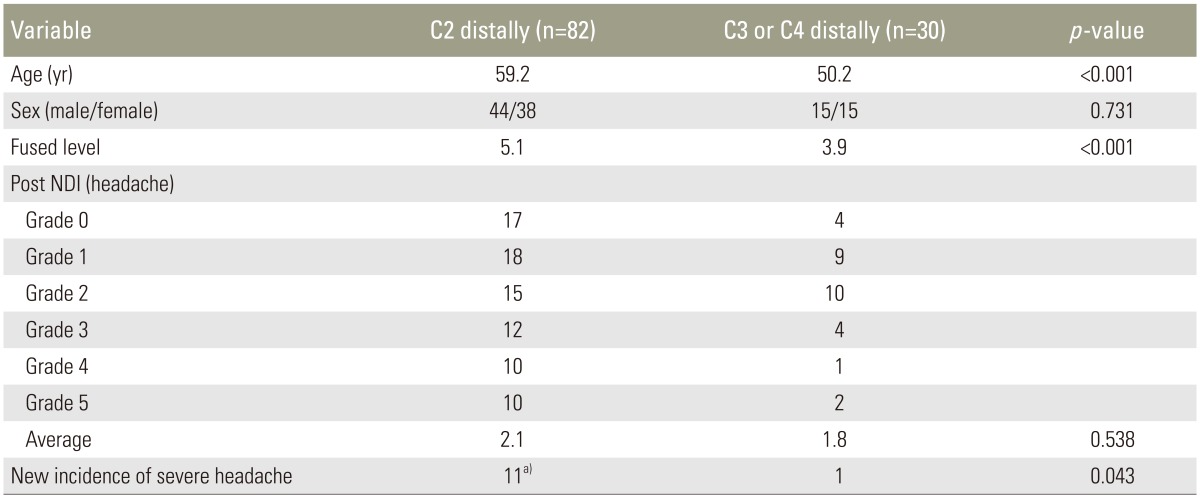
1. Severe headache after PSF from C2 distally compared with PSF from C3 or C4 distally
Eighty-two patients met the inclusion criteria for patients receiving PSF from C2 distally. There were 44 males and 38 females, with an average age of 59.2 years (range, 21–78 years). The mean follow-up periods were 2.9 years (range, 1–10.9 years). The mean number of cervical fused levels was 5.1 (1–6 levels). On the other hand, in the PSF C3 or C4 distally group, 30 patients (average age of 50.2 years) met the inclusion criteria (Table 1). While only one patient in the PSF from C3 or C4 distally group had severe headache newly occur after surgery, severe headache newly occurred postoperatively in 11 patients in the PSF from C2 distally group (p=0.04).
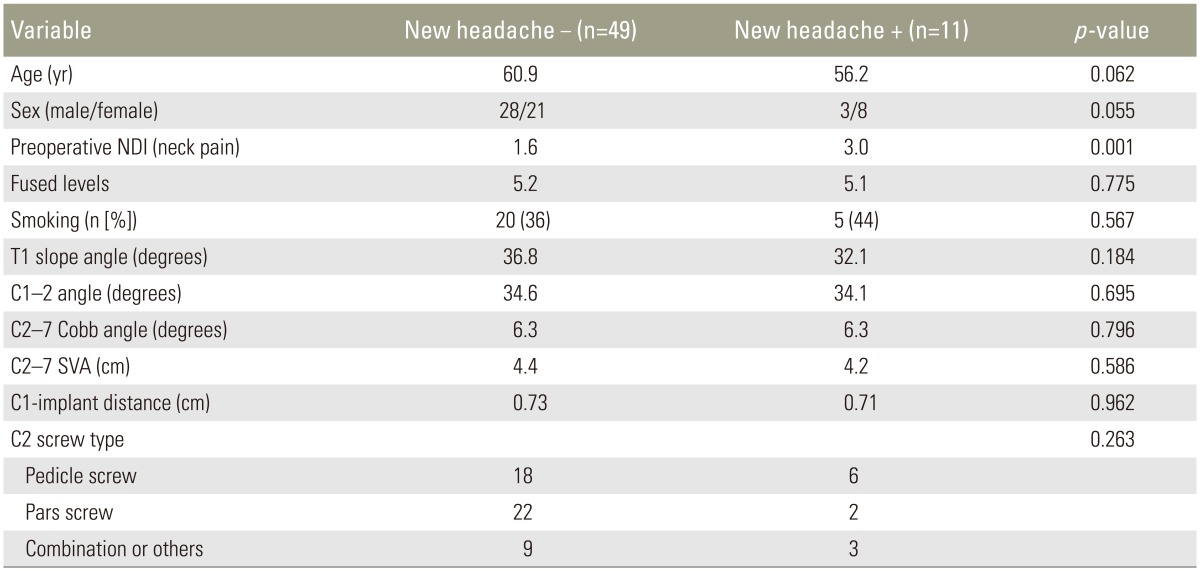
2. Clinical and radiological findings in 60 patients who demonstrated milder headache preoperatively
Among all PSF from C2 distally patients, 60 patients demonstrated preoperative milder headache. Of these 60 patients, 49 patients continued to have milder NDI headache scores (new headache-group) postoperatively, while 11 patients had newly occurring severe headache (new headache+group) postoperatively. The radiological parameters (T1 slope angle, C1–C2 angle, C2–7 Cobb angle, C2–7 SVA and C1 implant distance) were not significantly different from both groups. The new headache+group had significantly higher score for preoperative NDI for neck pain (p<0.01) (Table 2).
Discussion
No previous studies have evaluated severe headache after cervical PSF. In the present study, we found that a newly occurring severe headache after cervical PSF was more frequent in C2 distally fusions than in C3 or C4 distally fusions. We hypothesized that three risk factors might be associated with postoperative severe headache. First, adults with positive C2–7 SVA or cervical malalignment might increase C1–C2 lordosis in an effort to maintain horizontal gaze. Subsequently, the C2 nerve root would be impinged due to the hyperlordosis of C1, and this could cause C2 nerve irritation and severe headache. Secondly, if the patient had a longer C2–7 SVA, the tonus of the neck muscles could remain under considerable and prolonged tension, which could cause severe headache. Thirdly, a proximal implant such as a rod or screw head can irritate the bony structure or C2 nerve root and cause severe headache. To evaluate the hypothesis and risk factors, we evaluated clinical and radiological findings including T1 slope angle, C1–C2 lordosis angle, C2–7 Cobb angle, C2–7 SVA and C1-implant distance. However, these radiological spinal parameters were not significantly associated with severe headache after PSF from C2 distally. Among all patients, 20 patients still had severe headache after this procedure. Of note, 11 patients (10%) among 60 patients who had preoperative milder headache presented with newly occurring severe headache after surgery. In addition, cervical PSF treated cervicogenic severe headache effectively in 13 patients among the 22 patients who had preoperative severe headache.
The reason for the new prevalence of severe headache following cervical PSF is still unknown. Although axial symptoms (severe neck pain) after cervical laminoplasty have been reported in the literature [456], there has been no report on severe headache occurring after cervical posterior surgery. In recent years, a few studies reported axial symptoms occurring after cervical laminectomy with fixation [78]. Zhang et al. [7] reported that after laminectomy and lateral mass screw fixation, 40% of the patients showed axial symptoms postoperatively. This study showed that axial symptom severity correlated positively with the rate of muscle atrophy. Du et al. [8] reported the incidence of axial symptoms at 37.5% after laminectomy with lateral mass screw fixation, and loss of lordosis was positively related to axial symptom severity. They concluded that axial symptoms were the result of a complication induced by multiple factors and mechanisms after posterior cervical surgery and the explicit pathogenesis required further investigation. Some authors have reported that axial pain after cervical laminoplasty occurred due to neck muscle disruption, especially because of detachment of muscle insertions from the C2 or C7 spinous processes, or deep extensor muscles [91011]. As to the cause of the occurrence of severe headache after PSF C2 distally, in the similar way we considered it to be due to the removal of the muscles attached from C2 spinous process to allow the insertion of the screw.
On the other hand, Tang et al. [3] used radiological parameters such as C2–7 lordosis angle and C2–7 SVA to evaluate the relationship between regional cervical sagittal alignment and postoperative outcomes for patients who received multilevel posterior cervical fusion. They demonstrated that the severity of neck pain and disability increases with positive sagittal malalignment following surgical reconstruction. Contrary to their results and the first part of our hypothesis, in our present study, there were no significant associations with between radiological parameters such as cervical lordosis and C2–7 SVA and severe headache. This suggests that there was no C2 impingement around the C1/2 area due to the hyperlordosis of C1/2 and that greater C2–7 SVA distance did not increase pressure from the muscles around the neck and skull. Various factors such as revision surgery and a preoperative higher NDI score (neck pain and headache) had significant effects on newly occurring severe headache in this study.
On the other hand, Jansen et al. [12] reported an association between cervicogenic, hemicranial attacks and vascular irritation or compression of the C2 nerve root. They used electron microscopy to reveal focal, morphological changes of the C2 nerve root and the ganglion itself. They concluded that these morphological changes were possibly the result of chronic vascular compression. In addition, several authors proposed that one of the most important structures involved in the pathogenesis of occipital headache is the lateral C1–C2 joint [131415]. Ehni and Benner [13] described a group of elderly patients suffering from an occipital neuralgic pain syndrome aggravated by neck motion due to degenerative changes in a C1–C2 arthrosis.
Several limitations of our study must be acknowledged. First, this was a retrospective study. Second, we did not evaluate the O–C1 and C1–2 joints by computed tomography or magnetic resonance imaging. Severe osteroarthritis of these joints might cause severe headache, and previous literature reported on this in a series of case reports. However, none of those cases demonstrated C1/2 osteoarthritis on plain open-mouth X-ray. Third, we did not perform a C2 nerve block or facet block as a diagnostic tool of severe headache in every case. Thus, we did not determine the actual cause of the severe headache either preoperatively or postoperatively.
However, to the best of our knowledge, this study is the first to report the prevalence of severe headache after PSF from C2 distally and to assess the risk factors for severe headache after PSF from C2 distally through clinical and radiological findings. Thus, the current study should be useful for the spine surgeon making a decision about PSF from C2 distally as an operative treatment for cervical disorders.
Conclusions
Of 60 patients which had milder headache preoperatively, 11 (18%) had severe headache after PSF from C2 distally. A higher preoperative NDI score (neck pain and headache) increased the risk for newly occurring severe headache after PSF from C2 distally.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.