|
 |
- Search
| Asian Spine J > Volume 16(5); 2022 > Article |
|
Abstract
Purpose
This study is conducted to assess the trends in the charges and usage of computer-assisted navigation in cervical and thoracolumbar spinal surgery.
Overview of Literature
This study is the first of its kind to use a nationwide dataset to analyze trends of computer-assisted navigation in spinal surgery over a recent time period in terms of use in the field as well as the cost of the technology.
Methods
Relevant data from the National Readmission Database in 2015–2018 were analyzed, and the computer-assisted procedures of cervical and thoracolumbar spinal surgery were identified using International Classification of Diseases 9th and 10th revision codes. Patient demographics, surgical data, readmissions, and total charges were examined. Comorbidity burden was calculated using the Charlson and Elixhauser comorbidity index. Complication rates were determined on the basis of diagnosis codes.
Results
A total of 48,116 cervical cases and 27,093 thoracolumbar cases were identified using computer-assisted navigation. No major differences in sex, age, or comorbidities over time were found. The utilization of computer-assisted navigation for cervical and thoracolumbar spinal fusion cases increased from 2015 to 2018 and normalized to their respective years’ total cases (Pearson correlation coefficient=0.756, p=0.049; Pearson correlation coefficient=0.9895, p=0.010). Total charges for cervical and thoracolumbar cases increased over time (Pearson correlation coefficient=0.758, p=0.242; Pearson correlation coefficient=0.766, p=0.234).
Conclusions
The use of computer-assisted navigation in spinal surgery increased significantly from 2015 to 2018. The average cost grossly increased from 2015 to 2018, and it was higher than the average cost of nonnavigated spinal surgery. With the increased utilization and standardization of computer-assisted navigation in spinal surgeries, the cost of care of more patients might potentially increase. As a result, further studies should be conducted to determine whether the use of computer-assisted navigation is efficient in terms of cost and improvement of care.
Computer-assisted navigation has been widely adopted in spinal surgery because of its ability to aid in visualization, especially in complex spinal cases. Over the past three decades, advancements in technology have resulted in improved outcomes in orthopedic oncology, total knee arthroplasty, total hip arthroplasty, trauma surgery, and spinal surgery [1]. With the continuous increase in healthcare costs in the United States, efforts have been devoted to analyzing the effectiveness and value of novel technologies [2].
Approximately 1.62 million spinal procedures are performed in the United States each year, and this number is predicted to gradually increase over the next decades [3–5]. For example, thoracolumbar fusion procedures had a 63% increase in prevalence from 2004 to 2015 [4]. Similarly, the rate of cervical fusion procedure increased from 23.7 to 50.6 per 100,000 population from 1997 to 2012 [5]. Cervical and thoracolumbar spinal procedures are expected to increase over the next 2 decades [4,5]. Therefore, trends in the costs and utilization of technologies during these procedures, specifically computer-assisted navigation, should be assessed because of the rise in the number of thoracolumbar and cervical surgical cases coupled with the increasing concern over costs and resource utilization in healthcare [6].
Previous studies explored the application of computer-assisted navigation in orthopedics and analyzed its impact on patient outcomes in specific orthopedic subspecialties [7,8]. Some prior studies claimed that computer-assisted navigation in orthopedic surgery has gained increased acceptance in practice in recent years [7], but studies have yet to examine the trends associated with the utilization of computer-assisted navigation for cervical and thoracolumbar spinal surgery on a broader scale via a national-level database. In the present study, computer-assisted navigation procedures involve stereotactic navigation through computed tomography or fluoroscopic images to provide a projection of a patient’s anatomy (Fig. 1). This procedure provides insights into complex anatomy that will help surgeons better navigate previously hard-to-visualize areas. Some commonly used systems include Medtronic O-arm, StealthStation, Iso-C C-arm, and NaviVision [9]. Given the increased adoption of computer-assisted navigation for spinal surgery in the past decade, this study aims to assess the trends in the cost and utilization of computer-assisted navigation in cervical and thoracolumbar spinal surgery to better inform the surgeons of changes in practice.
Data recorded in 2015–2018 in the National Readmission Database (NRD), which contains data from approximately 18 million discharges in the United States every year, were retrospectively analyzed. In particular, data from 28 geographically dispersed states were collected, accounting for 58.7% of all the US hospitalizations. With the NRD, readmissions can be examined regardless of the expected payer type. However, the Healthcare Cost and Utilization Project (HCUP) Data Use Agreement forbids the reporting of frequencies fewer than 11 to account for healthcare privacy concerns when this database is used.
The International Classification of Diseases 10th revision (ICD-10) codes were implemented in the 3rd quarter of 2015. The ICD-9 and ICD-10 codes were utilized for the 2015 dataset because of the change in the 3rd quarter, and the ICD-10 codes were solely used for 2016–2018 datasets. The sampling weights provided by HCUP were used to adjust the analysis for all discharges in the United States. The institutional review board exemption was obtained from our institution for this study. The requirement for informed consent from individual patients was omitted because of the retrospective design of this study.
All the patients who underwent cervical and thoracolumbar spinal surgery with the aid of computer-assisted navigation were identified using ICD-9 and ICD-10 procedure codes. Of these patients, those who underwent elective and nonelective procedures were kept for subgroup analysis. Table 1 provides a list of all the ICD codes utilized in this study.
Patient characteristics, including demographic information (sex and age), diagnoses, and health insurance payer type, were obtained from the NRD.
Preoperative comorbidities were also identified using ICD-9 and ICD-10 via the R comorbidity package, which is utilized to calculate Charlson and Elixhauser comorbidity scores. Each value within R comorbidity corresponds to a particular preexisting medical condition identified in either the Charlson or Elixhauser index. Charlson and Elixhauser indices are two of the most well-known and utilized metrics of predicting patient outcome because of specific comorbidities. For the Charlson comorbidity index, which was developed by Charlson et al. [10], 17 comorbidities and their respective weights were included. A given patient’s comorbidities were then factored in to estimate the mortality risk. The same procedure was performed with the Elixhauser comorbidity index; however, Elixhauser et al. [11] defined 30 comorbidities for utilization [12].
Patients’ total charges, which are reported by the NRD and adjusted for inflation by using the consumer price index, were analyzed.
Data were statistically analyzed using SciPy ver. 1.6.1 (https://scipy.org/). The association between time and the number of patients receiving spinal surgery with computer-assisted navigation, the total charges of patients, and the ratio of patients with Medicare to patients with private insurance were examined through linear regression analysis.
A total of 48,116 cervical spine cases were included: 1,880 in 2015, 10,999 in 2016, 16,790 in 2017, and 18,447 in 2018 (Pearson correlation coefficient=0.756, p=0.049) (Table 2, Supplement 1).
The cases that utilized computer-aided navigation were normalized to the total number of cervical cases in each respective year to account for the potentially increasing number of cervical cases through the years. The proportions from 2015 to 2018 were 0.0432, 0.1438, 0.202, and 0.233, respectively (Pearson correlation coefficient=0.970, p=0.030) (Fig. 2).
A total of 27,093 thoracolumbar cases were included: 2,169 in 2015, 5,171 in 2016, 9,045 in 2017, and 10,708 in 2018 (Pearson correlation coefficient=0.9895, p=0.010) (Table 2, Supplement 2).
The cases that utilized computer-aided navigation were normalized to the total number of thoracolumbar cases in each respective year to account for the potentially increasing number of thoracolumbar cases through the years. The proportions in 2015, 2016, 2017, and 2018 were 0.0365, 0.0497, 0.0639, and 0.0666, respectively (Pearson correlation coefficient=0.969, p=0.031) (Fig. 3).
Of the patients who underwent cervical surgery with the use of navigation in 2015, 8.56% had 3+ Charlson comorbidities, and 14.0% of those that did not involve navigation had 3+ comorbidities. In 2018, 22.5% of patients who underwent cervical navigation surgery had 3+ comorbidities, whereas 13.2% who had surgery without navigation had 3+ comorbidities. For patients who had thoracolumbar navigation, 3.92% had 3+ comorbidities in 2015, and 15.1% who did not undergo the procedure with navigation had 3+ comorbidities in that same year. In 2018, 8.24% of patients with thoracolumbar navigation had 3+ comorbidities, and 11.7% of patients with nonnavigation had 3+ comorbidities (Table 3).
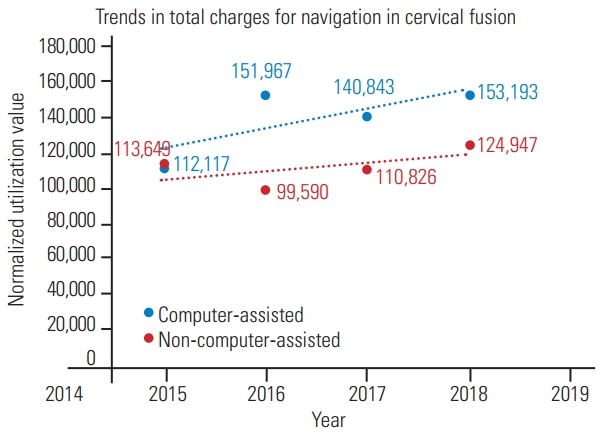
The average total charges of patients who received computer-assisted navigation during cervical fusion surgery in 2015, 2016, 2017, and 2018 were $112,117, $151,967, $140,843, and $153,193, respectively, after adjustments for inflation were made (Pearson correlation coefficient=0.758, p=0.242). These values were compared with the average total charges for nonnavigated cervical cases (2015, $113,649; 2016, $99,590; 2017, $110,826; and 2018, $124,947). The average charges for nonnavigated cases were grossly and significantly (p=0.046) lower than those for navigated cases (Fig. 4). The ratios of patients with Medicare to those with private insurance were 0.949 and 0.868 in 2015 and 2018, respectively.
The average total charges of patients who received computer-assisted navigation during thoracolumbar fusion surgery in 2015, 2016, 2017, and 2018 were $148,134, $150,900, $148,217, and $163,838, respectively (Pearson correlation coefficient=0.766, p=0.234). These values were compared with the average total charges for nonnavigated thoracolumbar fusion cases (2015, $119,860; 2016, $145,773; 2017, $149,522; and 2018, $156,675). The average charges for nonnavigated cases were overall grossly but not significantly (p=0.31) lower than the charges for navigated cases (Fig. 5). The ratio of patients with Medicare to those with private insurance increased from 1.17 in 2015 to 1.36 in 2018.
New technologies often emerge in the healthcare industry primarily to improve patient outcomes. They are accessible, cost effective, and accurate. For instance, computer-assisted navigation, a technological system invented in the early 1990s and first applied in orthopedics in 1997, has the potential to improve surgical outcomes by helping surgeons with navigational planning and procedural reproducibility [1,12]. Our study found a consistent increase in utilization from 2015 to 2018. Cervical and thoracolumbar cases with navigation significantly increased and remained significant even after normalization was made for the total number of fusion cases in each year. This finding indicated that the adoption of computer-assisted navigation utilization increased from 2015 to 2018. The associated total charges for cervical and thoracolumbar spinal surgery also increased during this period even when adjustments were made for inflation. However, neither thoracolumbar cases nor cervical cases had a significant increase in total charges. The average charges for the cases that utilized computer-assisted navigation were compared with those for noncomputer navigated cervical and thoracolumbar spinal surgery cases to reveal a potential increase in the cost burden of patients. The number of navigation-aided cases was consistently higher than that of nonnavigation cases. This difference was statistically significant for cervical cases but not for thoracolumbar cases. Therefore, cervical fusions utilizing navigation might cause an additional cost burden to patients.
As the utilization of navigation in cervical and thoracolumbar spine surgeries grows, the cost of care for more patients likely increases because of the utilization of a more advanced technology. Computer-assisted navigation has been proven to be more expensive than traditional methods when it is used intraoperatively in some orthopedic surgery types, such as total knee arthroplasty [12]. In the case of cervical and thoracolumbar spinal surgery, our evidence showed that the total charges for patients generally increased from 2015 to 2018. Our comparison of nonnavigated costs over time highlighted a potentially increasing cost burden specific to computer-assisted navigation in spinal surgery. As such, the possible rising cost burden coupled with an increased implementation of this technology should be further analyzed to determine the effectiveness of computer-assisted navigation in improving patient care and surgeon capabilities. With spinal surgeries under recent criticisms for their associated cost for patients [13], trends in the total charges of computer-aided navigation-utilizing procedures over time should be examined to predict the effect of this technology on the industry in the future. The computer-aided navigation charges over time observed in this study increased, so the perceived benefit of this technology to a surgeon’s performance and patient outcomes in cervical and thoracolumbar spine procedures should be explored. Previous studies claimed that the use of computer-aided navigation can improve the accuracy of pedicle screw placement in thoracic spinal surgery; however, future studies should explore the effect of navigation on patient outcomes [14,15].
Indications for computer-aided navigation utilization during cervical surgery differ from those during thoracolumbar surgery. Although computer-aided navigation is more typically used in thoracolumbar surgery for three-dimensional visualization, minimally invasive surgery, and pedicle screw implementation [15,16], it is used less typically in cervical surgery to assist surgeons with instrumentation in patients with atypical spine anatomy [17]. Therefore, costs, utilization, and demographics varied among the cervical and thoracolumbar populations in this study.
The distribution of the age and gender of patients receiving computer-aided navigation for cervical and thoracolumbar fusion has not changed significantly over time. Additionally, the insurance coverage distribution has remained largely unchanged over time, and the number of thoracolumbar patients covered by Medicare has slightly increased compared with that of patients covered by private insurance. We hypothesized that this increase in the number of patients covered by Medicare for computer-aided navigation-utilized thoracolumbar surgeries was due to the more routine use of computer-aided navigation, specifically for thoracolumbar procedures. Computer-aided navigation has become commonly used for operating in the thoracolumbar region [8,16], so more of these cases are likely covered by Medicare plans. This finding might account for the increase in the thoracolumbar population and the lack of increase in the percentage of Medicare-covered patients among cervical cases.
Another notable large discrepancy between 2015 and 2018 was the readmission rate. For cervical cases utilizing computer-aided navigation, the rate of 90-day readmission increased substantially from 2.9% in 2015 to 27.0% in 2018. Computer-aided navigation is utilized in cervical cases involving typically complex spinal anatomy [17], such as C1–C2 deformity. Revision surgery readmission rates likely increased substantially from 2015 to 2018 because of the increased adoption of computer-aided navigation for complex cervical cases in patients with increased comorbidities. For cervical and thoracolumbar surgeries performed with computer-aided navigation, the percentage of patients who had higher Elixhauser and Charlson comorbidity scores (>3) increased between 2015 and 2018, indicating potentially more difficult and complex cases because of the higher likelihood of comorbidities (Table 3).
More specifically, the percentage of patients with 3+ comorbidities in the navigated cervical group over time substantially increased compared with that of the nonnavigated cervical group (13.94% versus –3.4%, respectively). This finding differed from the comparison between the thoracolumbar navigated and nonnavigated groups. In the thoracolumbar cases, the percentage difference over time in patients with 3+ comorbidities was more similar (4.32% versus –3.4%, respectively). This observation could explain the differences in the increased readmission rates over time in cervical navigated cases and thoracolumbar cases. Patients with higher Charlson comorbidity indices have a higher readmission risk of revision or associated medical complications, thus increasing the readmission rates of cervical cases over time. Similarly, the change in 90-day readmission rates of the navigated thoracolumbar cases increased between 2015 (4.0%) and 2018 (13.4%). However, this increase in percentage was lower than that of the cervical results.
The increased percentage of patients with higher Elixhauser and Charlson comorbidity scores in 2018 compared with that in 2015 led to an increase in the 90-day readmission rate in thoracolumbar fusion cases. Prior comorbidities were shown as independent predictors of readmission, so the higher comorbidity scores were a potential reason for higher readmission rates [18,19]. Likewise, Whitmore et al. [20] showed that the increasing Charlson comorbidity score is associated with a significantly higher risk of complications in patients undergoing spinal surgery. Moreover, the increase in readmissions and comorbidity scores likely contribute to the increase in charges for cervical and thoracolumbar navigation cases. Thus, the trend of increasing cost over time cannot be entirely attributed to the growing utilization of this new technology, that is, as comorbidities and readmissions increase, average charges potentially increase.
A notable trend in thoracolumbar and cervical cases in terms of the proportion of elective and nonelective procedures was observed. In comparison with the percentage in 2015, the percentage of elective cervical and thoracolumbar procedures in 2018 decreased; conversely, the percentage of nonelective procedures subsequently increased although these changes were much more dramatic for the cervical cases (Table 2). In other fields, nonelective cases are more associated with intraoperative complications and postoperative adverse outcomes [20]. Based on this hypothesis, an interpretation of our findings is that nonelective cases are overall more likely to be complicated from the start than elective procedures [21]. However, further studies should be conducted to elucidate this discrepancy. We also hypothesized that this trend of increasing proportion of nonelective cases could be associated with the increase in computer-assisted navigation utilization. As more surgeons become comfortable using this advanced technology in their operating room, they are potentially more likely to use it during atypical procedures, such as nonelective cases.
Although ICD-10 codes are specific to the use of computer-aided navigation in thoracolumbar or cervical spinal surgery, no ICD-9 codes specific to either type of procedures are established. As a result, the patient populations of NRD datasets that use ICD-9 codes (2015) should be estimated using ICD-9 codes for the general use of computer-aided navigation coupled with ICD-9 codes for either thoracolumbar or cervical spinal surgery. The low number of cervical cases that utilized computer-aided navigation from the NRD is partly attributed to coding estimation, that is, an ICD-9 code specific to cervical computer-aided navigation cases is unavailable; as such, we used a combination of computer-aided navigation-specific codes and cervical fusion surgery-specific codes. The 2015 data incorporated ICD-9 and ICD-10 codes because of the national coding alteration that occurred in October of that calendar year. This change in the coding system could contribute to the trends found in this analysis, so future studies should include data recorded in 2019 onward to confirm the continuation of the trends identified in this study. The number is low because most cervical cases (>80%) are anterior fusion cases [22,23], which are usually not subjected to computer-aided navigation because instrumentation in these procedures can normally be placed without aided visualization [7,22]. Additionally, this study found that the adoption of navigation in cervical cases was greater than that in thoracolumbar cases. This finding was likely due to the more complex anatomy of the cervical region, but this assumption could not be made because of the limitations of the NRD’s classification system for patient diagnosis. Future studies should focus on comparing prior diagnosis of the abnormal spinal anatomy between cervical and thoracolumbar navigated cases and their associated clinical outcomes and costs. We postulated that the utilization of navigation in spinal surgery will continue to increase over time as more surgeons are trained on computer-aided navigation. More data will have to be collected beyond 2018 to further assess utilization and total charge trends over the past 4 years and identify if they align with the results obtained in this study.
The prevalence of computer-aided navigation in cervical and thoracolumbar spinal surgery significantly increased from 2015 to 2018 even when the overall increase in cervical and thoracolumbar fusion cases was considered. This finding indicates that the proportion of these surgeries involving navigation increases. The use of these technologies is also associated with an increase in total charges for patients even when adjustments for inflation are made and when the cost trends of nonnavigated spinal cases are compared. Further research should be conducted to determine whether computer-aided navigation is necessary and cost effective for patients, especially when it is used for spinal procedures. With the advent and increased acceptance of computer-assisted technology and methods, appropriate analysis should be performed to ensure that the use of this technology indeed provides cost effective benefits to patients undergoing cervical and thoracolumbar spinal fusion surgeries.
Notes
Author Contributions
Conception and design: Varun Arvind, Jun S. Kim, Samuel K. Cho; data acquisition: Calista L. Dominy, Justin E. Tang, Varun Arvind; analysis of data: Calista L. Dominy, Justin E. Tang; drafting of the manuscript: Calista L. Dominy, Justin E. Tang, Brian H. Cho, Stephen Selverian, Kush C. Shah; critical revision: all authors; supervision: Varun Arvind, Brian H. Cho, Jun S. Kim, Samuel K. Cho; and all authors read and approved the final manuscript.
Notes
Supplementary Materials
Supplementary materials can be available from https://doi.org/10.31616/asj.2021.0258. Supplement 1. Cervical demographic results, 2015–2018. Supplement 2. Thoracolumbar demographic results, 2015–2018.
Fig. 1
Utilization of computer-aided navigation for cervical fusion surgery from 2015 to 2018, normalized for total number of cervical fusions performed each year.
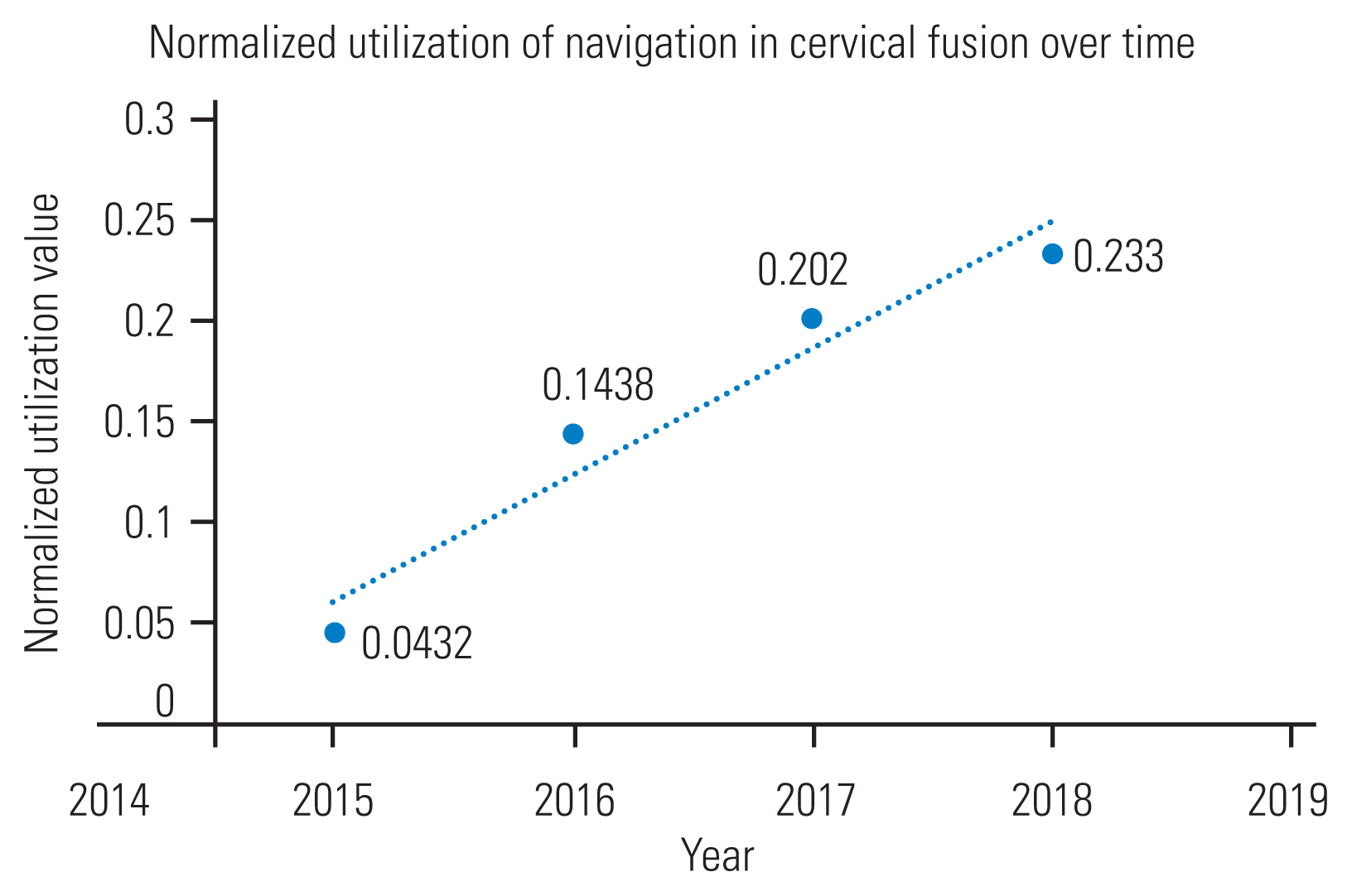
Fig. 2
Utilization of computer-aided navigation for thoracolumbar fusion surgery from 2015 to 2018, normalized for total number of thoracolumbar fusion cases per year.
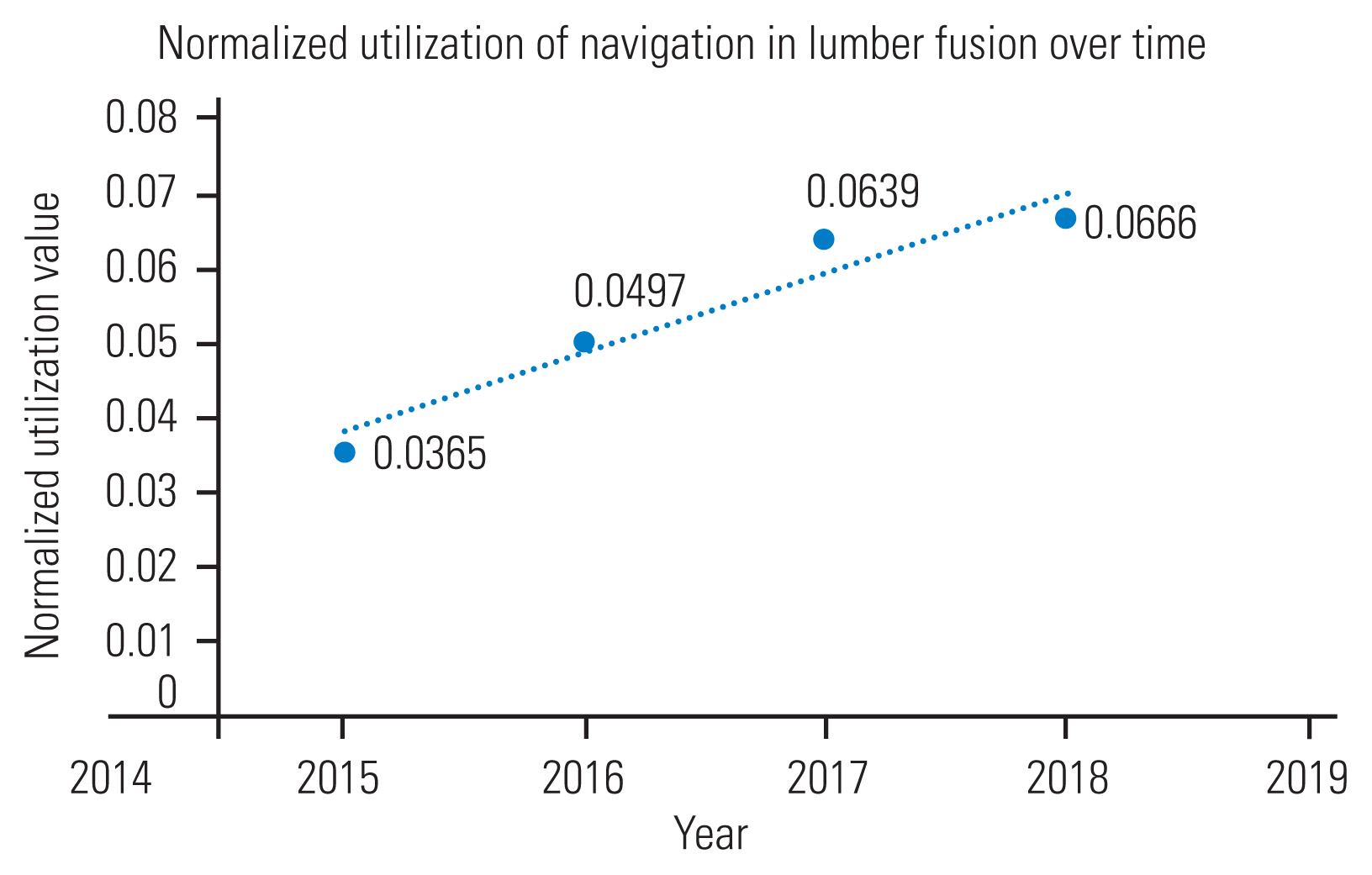
Fig. 4
Total charges for computer-aided navigation in thoracolumbar fusion surgery from 2015 to 2018.
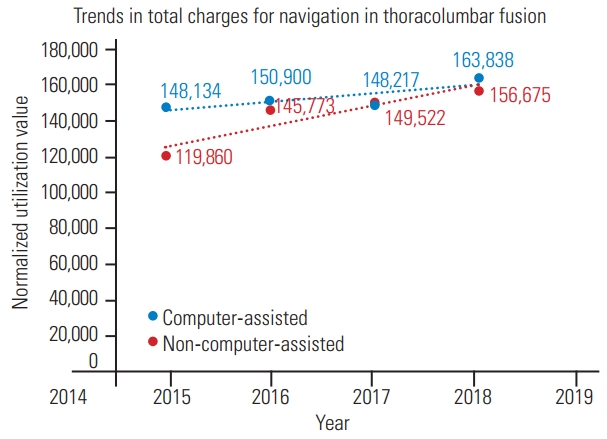
Fig. 5
Total charges for computer-aided navigation in thoracolumbar fusion surgery from 2015 to 2018.
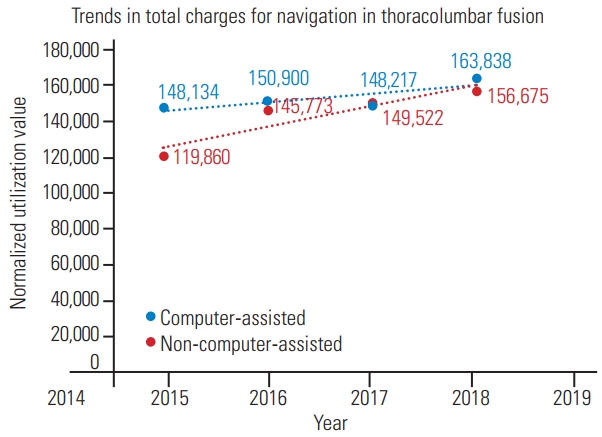
Table 1
Inclusion ICD-9 and ICD-10 codes
Table 2
Demographics for cervical and thoracolumbar cases for years 2015 and 2018
| Characteristic | Cervical | Thoracolumbar | ||
|---|---|---|---|---|
|
|
|
|||
| 2015 (N=1,880) | 2018 (N=18,447) | 2015 (N=2,169) | 2018 (N=10,708) | |
| Sex | ||||
|
|
||||
| Female | 980 (52.1) | 9,339 (50.6) | 1,191 (54.9) | 5,600 (52.3) |
|
|
||||
| Male | 900 (47.9) | 9,108 (49.7) | 978 (45.1) | 5,108 (47.7) |
|
|
||||
| Age (yr) | ||||
|
|
||||
| <18 | 76 (4.04) | 1,176 (6.4) | 57 (2.6) | 382 (3.6) |
|
|
||||
| 18–49 | 471 (25.1) | 5,117 (27.7) | 465 (21.4) | 1,772 (16.5) |
|
|
||||
| 50–59 | 451 (24.0) | 3,635 (19.7) | 506 (23.3) | 2,086 (19.5) |
|
|
||||
| 60–69 | 474 (25.2) | 4,420 (24.0) | 599 (27.6) | 3,202 (29.9) |
|
|
||||
| 70–79 | 333 (17.7) | 885 (4.8) | 433 (20.0) | 2,670 (24.9) |
|
|
||||
| ≥80 | 75 (3.99) | 405 (4.9) | 109 (5.0) | 596 (5.6) |
|
|
||||
| Primary payer | ||||
|
|
||||
| Medicare | 746 (39.7) | 6,807 (36.9) | 955 (44.0) | 5,218 (48.7) |
|
|
||||
| Private insurance | 786 (41.8) | 7,845 (42.5) | 815 (37.6) | 3,835 (35.8) |
|
|
||||
| Medicaid | 186 (9.89) | 2,649 (14.4) | 191 (8.8) | 874 (8.2) |
|
|
||||
| Self-pay | 34 (1.81) | 443 (2.4) | 17 (0.8) | 129 (1.2) |
|
|
||||
| Other/unknown | 128 (6.81%) | 650 (3.5) | 191 (8.8) | 652 (6.1) |
|
|
||||
| Discharge status | ||||
|
|
||||
| Routine | 1,244 (66.2) | 12,567 (68.1) | 1,382 (63.7) | 6,606 (61.7) |
|
|
||||
| Home health care | 325 (17.3) | 2,931 (15.9) | 423 (19.5) | 2,354 (22.0) |
|
|
||||
| Transfer to short-term hospital | 15 (0.8) | 168 (0.9) | a) | 56 (0.5) |
|
|
||||
| Transfer to other facility | 284 (15.1) | 2,510 (13.6) | 346 (16.0) | 1,639 (15.3) |
|
|
||||
| Against medical advice | b) | 71 (0.4) | a) | 20 (0.2) |
|
|
||||
| Died in hospital | a) | 198 (1.1) | a) | 33 (0.3) |
|
|
||||
| Surgery characteristics | ||||
|
|
||||
| Elective | 1,411 (75.1) | 9,033 (49.0) | 1,785 (82.3) | 8,354 (78.0) |
|
|
||||
| Nonelective | 469 (24.9) | 9,339 (51.0) | 383 (17.7) | 2,354 (22.0) |
|
|
||||
| Readmission within 90 days | 54 (2.87) | 4,987 (27.0) | 86 (4.0) | 1,438 (13.4) |
Table 3
Elixhauser and Charlson comorbidity scores
References
1. Deep K, Shankar S, Mahendra A. Computer assisted navigation in total knee and hip arthroplasty. SICOT J 2017 3:50.



2. Passias PG, Brown AE, Alas H, et al. A cost benefit analysis of increasing surgical technology in lumbar spine fusion. Spine J 2021 21:193–201.


3. Antonios JK, Korber S, Sivasundaram L, et al. Trends in computer navigation and robotic assistance for total knee arthroplasty in the United States: an analysis of patient and hospital factors. Arthroplast Today 2019 5:88–95.



4. Martin BI, Mirza SK, Spina N, Spiker WR, Lawrence B, Brodke DS. Trends in lumbar fusion procedure rates and associated hospital costs for degenerative spinal diseases in the United States, 2004 to 2015. Spine (Phila Pa 1976) 2019 44:369–76.


5. Salzmann SN, Derman PB, Lampe LP, et al. Cervical spinal fusion: 16-year trends in epidemiology, indications, and in-hospital outcomes by surgical approach. World Neurosurg 2018 113:e280–95.


6. Deyo RA, Mirza SK, Martin BI, Kreuter W, Goodman DC, Jarvik JG. Trends, major medical complications, and charges associated with surgery for lumbar spinal stenosis in older adults. JAMA 2010 303:1259–65.



7. Mimidis G, Mavrogenis AF, Savvidou OD, et al. Computer-assisted navigation in knee surgery. J Long Term Eff Med Implants 2012 22:313–22.


8. Karkenny AJ, Mendelis JR, Geller DS, Gomez JA. The role of intraoperative navigation in orthopaedic surgery. J Am Acad Orthop Surg 2019 27:e849–58.


9. Gasparini A. Comorbidity: an R package for computing comorbidity scores. J Open Source Softw 2018 3:648.


10. Charlson ME, Pompei P, Ales KL, MacKenzie CR. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987 40:373–83.


11. Elixhauser A, Steiner C, Harris DR, Coffey RM. Comorbidity measures for use with administrative data. Med Care 1998 36:8–27.


12. Trieu J, Schilling C, Dowsey MM, Choong PF. The cost-effectiveness of computer navigation in primary total knee replacement: a scoping review. EFORT Open Rev 2021 6:173–80.




13. Fiani B, Quadri SA, Farooqui M, et al. Impact of robot-assisted spine surgery on health care quality and neurosurgical economics: a systemic review. Neurosurg Rev 2020 43:17–25.



14. Han W, Gao ZL, Wang JC, et al. Pedicle screw placement in the thoracic spine: a comparison study of computer-assisted navigation and conventional techniques. Orthopedics 2010 33.

15. Wu H, Gao ZL, Wang JC, Li YP, Xia P, Jiang R. Pedicle screw placement in the thoracic spine: a randomized comparison study of computer-assisted navigation and conventional techniques. Chin J Traumatol 2010 13:201–5.

16. Scholler K, Jablawi F. Navigation in lumbar spinal surgery: when is it useful? Orthopade 2019 48:59–68.

17. Wallace N, Schaffer NE, Freedman BA, et al. Computer-assisted navigation in complex cervical spine surgery: tips and tricks. J Spine Surg 2020 6:136–44.



18. Phruetthiphat OA, Otero JE, Zampogna B, Vasta S, Gao Y, Callaghan JJ. Predictors for readmission following primary total hip and total knee arthroplasty. J Orthop Surg (Hong Kong) 2020 28:2309499020959160.



19. Koh J, Galvin JW, Sing DC, Curry EJ, Li X. Thirty-day complications and readmission rates in elderly patients after shoulder arthroplasty. J Am Acad Orthop Surg Glob Res Rev 2018 2:e068.



20. Whitmore RG, Stephen JH, Vernick C, et al. ASA grade and Charlson comorbidity index of spinal surgery patients: correlation with complications and societal costs. Spine J 2014 14:31–8.


21. Ando T, Adegbala O, Villablanca P, et al. Incidence, predictors, and in-hospital outcomes of transcatheter aortic valve implantation after nonelective admission in comparison with elective admission: from the nationwide inpatient sample database. Am J Cardiol 2019 123:100–7.