A New Clinical Tool for Scoliosis Risk Analysis: Scoliosis Tele-Screening Test
Article information
Abstract
Study Design
Methodological, observational clinical study.
Purpose:
This study aimed to develop a virtual screening test to detect scoliosis risk initially by parents without the need for medical visit during the coronavirus disease 2019 pandemic.
Overview of Literature
The scoliosis screening program has been implemented to early detect scoliosis. Unfortunately, access to health professionals was limited during the pandemic. However, during this time, interest in telemedicine has increased remarkably. Recently, mobile applications related to postural analysis were developed, but none permits evaluation by parents.
Methods:
Researchers developed the Scoliosis Tele-Screening Test (STS-Test), which included drawing-based images of body asymmetries, to assess the scoliosis-associated risk factors. The STS-Test was shared on social networks, allowing the parents to evaluate their children. After test completion, the risk score was generated automatically, and children with medium and high risks were then advised for medical consultation for further evaluation. The test accuracy and consistency between the clinician and parents were also analyzed.
Results:
Of the 865 tested children, 358 (41.4%) consulted clinicians to confirm their STS-Test results. Scoliosis was then confirmed in 91 children (25.4%). The parents were able to detect asymmetry in 50% of the lumbar/thoracolumbar curvatures and 82% of the thoracic curvatures. In addition, the forward bend test revealed favorable agreement between parents and clinicians (r=0.809, p<0.0005). Internal consistency of the esthetic deformities domain in the STS-Test was also excellent (α=0.901). This tool was 94.97% accurate, 83.51% sensitive, and 98.87% specific.
Conclusions:
The STS-Test is a new parent-friendly, virtual, cost-effective, result-oriented, and reliable tool for scoliosis screening. It allows parents to actively participate in the early detection of scoliosis by screening their children for the risk of scoliosis periodically without the need to visit the health institution.
Introduction
Scoliosis is a three-dimensional complex structural deformity characterized by a lateral deviation of the spine above 10° on coronal spine radiography, accompanied by axial rotation and sagittal plane deviations [1]. It has several different types that affect children and adolescents. Currently, the most common type is “adolescent idiopathic scoliosis” (AIS). AIS generally develops during the period from puberty onset to growth plate closure, between the ages of 10 years and 18 years, and its prevalence is reportedly 2%–3% [2–4].
The scoliosis screening program has been implemented for many years in most countries worldwide to early detect scoliosis. Although it is recommended scientifically, its cost-effectiveness remains controversial. Nevertheless, it remains to be the most valid method.
During the coronavirus disease 2019 (COVID-19) pandemic, school education was suspended, and access to health professionals was limited. Thus, interest in telemedicine and the number of studies on virtual examinations have remarkably increased [5,6]. In recent years, certain mobile applications related to postural analysis have been developed; however, none of these methods is suitable for parents to use. To address the question of how suspected scoliosis can be noticed by parents, a research team of experts have developed the Scoliosis Tele-Screening Test (STS-Test). This tool allows parents to evaluate their children on the risk of scoliosis without the need to visit any health institution, where families had a restricted access because of the COVID-19 pandemic.
This methodological and observational clinical study aimed to develop a tele-screening test that enables parents to personally detect scoliosis and observe the spine periodically. The reliability and validity of this tool was also determined.
Materials and Methods
The study conformed to the principles of the Declaration of Helsinki. It was conducted between July 2020 and January 2021, with approval from the Trakya University Medical Ethics Committee (date: September 14, 2020; approval no., 2020/287), and was registered at ClinicalTrials.gov (registration no., NCT04873986). All parents/caregivers of the patients included in the study provided written informed consent.
1. Assessment tools
Researchers developed the STS-Test, which includes drawing-based images of body asymmetry associated with scoliosis. In cases of suspected scoliosis, Trunk Aesthetic Clinical Evaluation (TRACE), Adams’ forward bend test (FBT), full spine posterior-anterior radiographs, and lateral radiographs were also evaluated.
2. Development of the STS-Test
The research team consisted of seven experienced scoliosis specialists (five physiatrists and two physiotherapists). They discussed possible methods that can be performed in a virtual environment to evaluate scoliosis, and eventually created a virtual scoliosis screening test. The researchers’ common database contained images of body asymmetries of patients with scoliosis with different deformity characteristics. These images were then analyzed for the development of the STS-Test’s scoring system. Through expert opinions and consensus, the scoring system was ultimately created. The risk of scoliosis was determined by considering the visual body asymmetries in the shoulder, scapula, thorax, waist, and pelvis, in addition to the FBT. Additional risk factors were also considered.
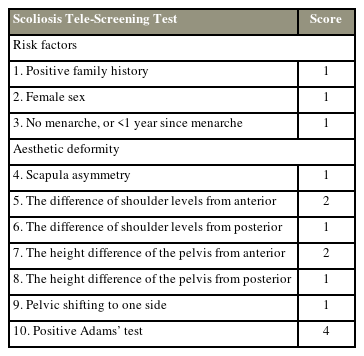
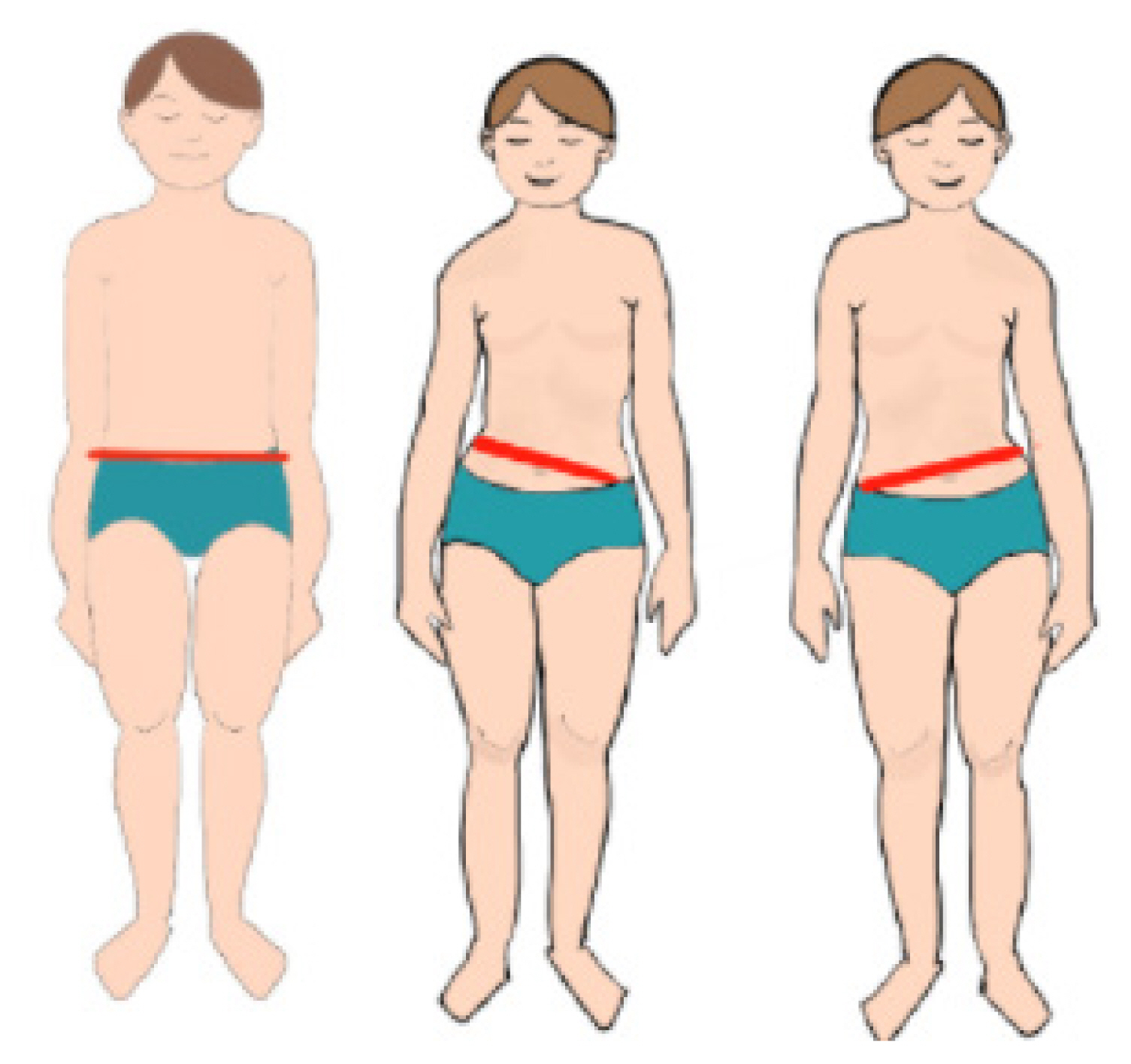
The STS-Test comprises risk factors and esthetic deformity domains: three items evaluating the risk factors related to scoliosis development and seven items evaluating possible esthetic deformities observed in scoliosis. The total score was obtained by adding all the scores of these ten items. The item that includes the FBT, which is the most widely used and valid test for scoliosis screening, was decisive in creating risk groups and was allotted 4 points [7]. The risk factors included family history, female sex, no menarche, and <1 year since menarche; each was allotted 1 point. The reasons for including these risk factors were as follows: scoliosis is more common and progressive in females; patients with a positive family history of scoliosis have a higher risk of developing scoliosis than those without; and menarche indicates the remaining growth potential in girls, and higher growth potential is associated with an increased risk for scoliosis [8–11]. The chronological age was not considered because it is not a precise indicator. Other body asymmetries caused by scoliosis were added to the total score, and risk groups were then determined (Table 1).
3. Pilot study
A pilot study including 50 parents was conducted to confirm whether the test is understandable and has application difficulties. After the revisions, the researchers agreed on a final version (Appendix 1).
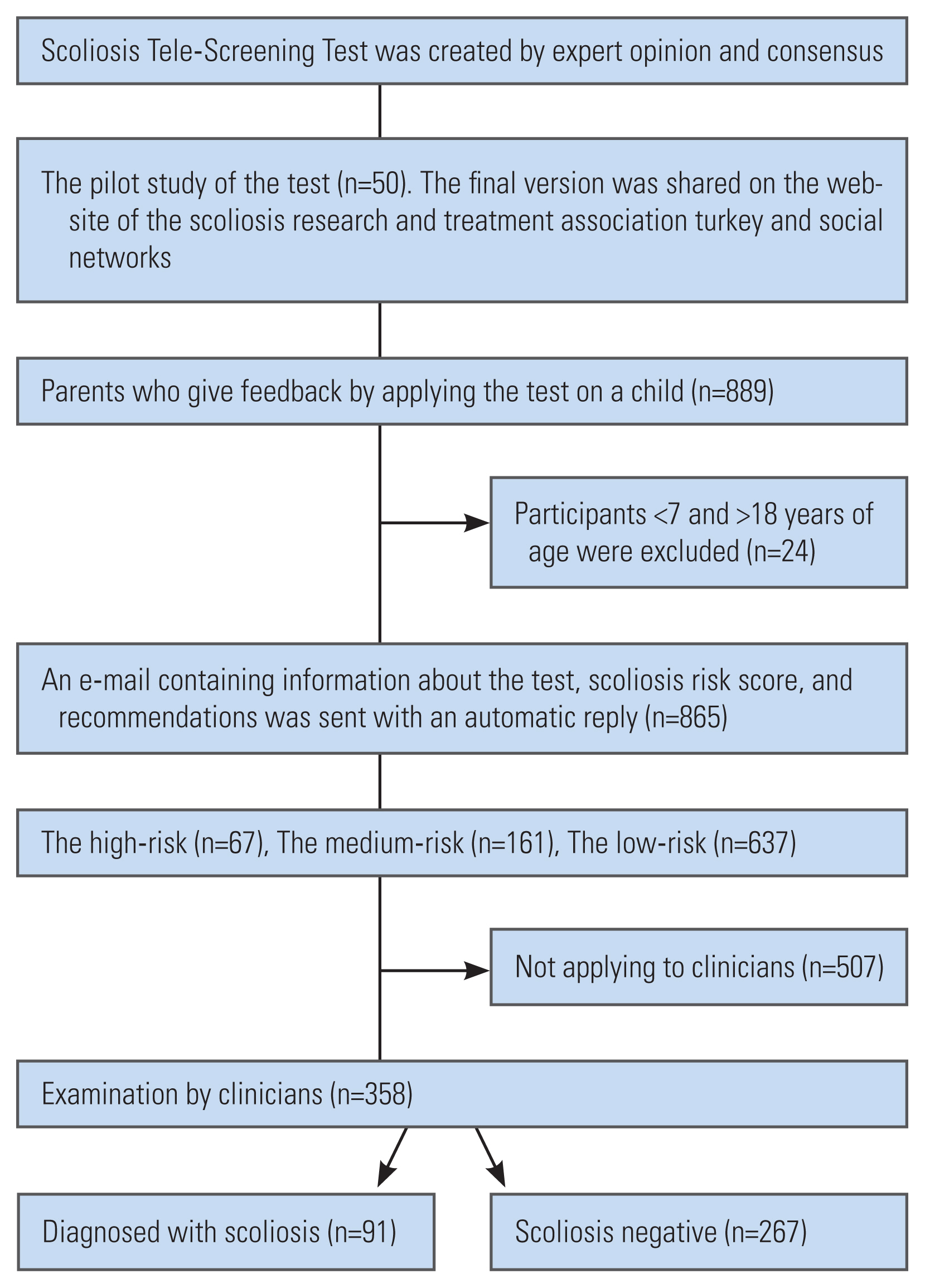
4. Participants and procedure
The final version was shared on the websites and social networks of the Scoliosis Research and Treatment Association, Turkey. The information note states that the STS-Test should not be performed for children with neurological diseases, previous spinal surgery, and inability to stand. A total of 889 parents applied the test to their children, but the responses of participants under seven and above 18 years old were excluded. Ultimately, 865 responses were eligible for the analysis. After the parents/evaluator completed the test, the risk score was generated automatically by the system and then shared with them via an e-mail containing information about scoliosis, the risk score, and recommendations.
Children with medium and high risks for scoliosis according to the risk category were advised to visit the research centers for further evaluation. Parents who could not reach these centers were asked to take pictures of their children wearing underwear while standing on a flat floor in the natural straight posture from the back and the FBT position for the virtual evaluation. These photographs were then sent to the researchers via e-mail. The researchers evaluated the TRACE and FBT from the photographs and gave their expert opinions to the parents via e-mail. Children with suspected scoliosis were recommended to consult a scoliosis specialist. For those who could visit the research center, they were examined by a physiatrist and evaluated using TRACE and FBT. Suspected scoliosis was confirmed using spine radiography (Fig. 1). The location, direction, and Cobb angle were recorded in the database. Parents’ sociodemographic characteristics, scoliosis knowledge/awareness level, and STS-Test–related satisfaction were also determined.
TRACE is an esthetic assessment tool used by clinicians to evaluate trunk asymmetries in patients with scoliosis [12]. TRACE provides a global score based on four subscales: shoulder (0–3), scapulae (0–2), hemithorax (0–2), and waist (0–4). The total score, which varies between 1 and 12, is obtained by adding one point to the sum of the 4-item score, with high scores indicating increased trunk asymmetry. Furthermore, FBT is one of the principal screening tests for scoliosis and demonstrates the rotational component of scoliosis [13].
5. Statistical analysis
Statistical data were analyzed using IBM SPSS Statistics for Windows ver. 23.0 (IBM Corp., Armonk, NY, USA). Numerical variables are presented as mean and standard deviation. Categorical variables are presented as frequencies and percentages. Kolmogorov-Smirnov tests for normality were used to determine the distribution. According to the distribution, differences between two independent groups were compared using the Mann-Whitney U test or independent sample t-test; for comparing more than two groups, the Kruskal-Wallis test was used. Categorical variables were analyzed using Pearson’s chi-square test. A p-value of ≤0.05 was considered statistically significant. Moreover, Pearson’s and Spearman’s correlation coefficients were used to investigate the correlations between parameters. Internal consistency was measured using Cronbach’s α to assess the degree to which items on the STS-Test are interrelated; it is interpreted as follows: excellent ≥0.9; good ≥0.8; and low ≤0.7. The specificity, sensitivity, negative predictive value, positive predictive value (PPV), and test accuracy of the STS-Test were also calculated. In addition, correlations of the STS-Test with TRACE, FBT, and scoliosis diagnosis were analyzed.
Results
The STS-Test was applied to 865 children (511 females and 354 males) by their parents. Table 2 lists their risk classification results. Out of 865 children, 358 (41.4%) were asked to confirm their STS-Test results by clinicians; among them, 91 (25.4%) were diagnosed with scoliosis, and 267 (74.6%) were confirmed to be negative. Table 3 summarizes the radiological results and clinical features of patients with scoliosis. Of the 54 thoracic curvatures, 44 (82%) were positive for the FBT item in the STS-Test (Question 10). However, parents recognized 50% of the asymmetries in 81 lumbar/thoracolumbar curvatures. Furthermore, 26 (32%), 34 (42%), and 29 (36%) children had anterior pelvic asymmetry (Question 5), posterior pelvic tilt (Question 8), and posterior pelvic shift (Question 9), respectively.
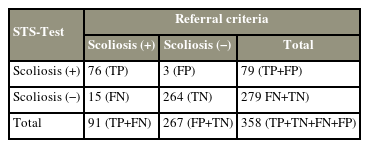
The STS-Test scores positively correlated with scoliosis diagnosis by a physiatrist. The FBT (Question 10) performed by parents also strongly correlated with the FBT performed by clinicians (Table 4). The Cronbach’s α of internal consistency (inter-items) for the esthetic deformity domain in the STS-Test was 0.901, which indicates excellence. Table 5 summarizes the referral criteria for the STS-Test’s accuracy based on the FBT and examination (including radiological confirmation, if necessary) conducted by a clinician.
Regarding the education level, 68.1% of the parents were university graduates, and 19% were high school graduates. The STS-Test was reported to be easy to apply by 93.3% of the parents and useful by 97.7%. In addition, 97.1% of the parents considered suggesting this tool to their relatives, and 96.8% thought that screening should be continued.
Discussion
The STS-Test, which was developed during this study, is a new telemedicine-based assessment tool for the early detection of scoliosis. This tool was applied to 865 children by their parents, of which 358 were advised to consult clinicians to confirm the STS-Test results. Among these 358 children, 25% were diagnosed with scoliosis by clinicians. The STS-Test highly correlated with routine clinical scoliosis screening tests used for detecting scoliosis risk. The agreement between the risk analyzes obtained using the STS-Test performed by the parents and face-to-face spine assessment by a physiatrist was determined. In this study, the STS-Test was highly specific (99%) and highly sensitive (84%) for scoliosis risk analysis, and parents’ overall satisfaction with this virtual tool was quite high.
All screening programs aim to detect patients who have a high-risk of developing scoliosis. The scoliometer, FBT, and Moiré topography are the most common methods used worldwide for scoliosis screening. The more screening tests are used, the more accurate the screening is. In addition, the sensitivity and PPV of screening programs vary according to whether single or multiple screening tests are used and by the selected threshold for a positive screening result [7]. The sensitivity and specificity of scoliosis screening depend on what method is used. In particular, the scoliometer depends largely on the experience of the clinician, the cutoff point, and the magnitude of scoliosis [7]. Although the FBT is fast, sensitive, and cost-effective, it insufficiently evaluates minor curvatures and lumbar curvatures [2]. The accuracy of screening is highest (93.8% sensitivity and 99.2% specificity) when three separate screening tests are used; when only the FBT is used (84.4%), the sensitivity decreases [7]. Furthermore, TRACE evaluates asymmetry only from the posterior aspect and ignores pelvic asymmetry. In contrast, the STS-Test combines esthetic evaluation, the FBT, sex, menarche, and family history of scoliosis, thereby increasing its accuracy. This tool was found to be 94.97% accurate, 83.51% sensitive, and 98.87% specific. According to the results of the present study, the STS-Test was sensitive and specific for detecting scoliosis, comparable to the examination conducted by the clinician (Table 5). While the PPV for the STS-Test alone was 96.20%, the highest PPV was 81.0% when combining the FBT, scoliometer measurement, and Moiré topography [7–16].
Of all the thoracic curvatures, 82% could be noticed easily with the FBT item in the STS-Test. Esthetic deformity caused by scoliosis is more pronounced in the thoracic curvatures, thereby easily recognized by parents, with the FBT at a rate comparable to that of the clinicians. The FBT performed by parents strongly correlated with that performed by the clinicians, indicating good agreement (r=0.809, p<0.0005). However, the esthetic effect of lumbar/thoracolumbar curvatures, except for larger curves, does not provide conspicuous findings as much as the thoracic curvatures. In fact, the parents could detect 50% asymmetries in the STS-Test. Yılmaz et al. [2] reported that FBT insufficiently detects minor curvatures, especially the lumbar or thoracolumbar curvatures. Therefore, the images of esthetic deformities of the pelvis caused by lumbar/thoracolumbar curvatures were better incorporated in the STS-Test. Potential overlooking of the lumbar/thoracolumbar curvatures was predicted at the planning stage and considered in the risk score, thereby strengthening the STS-Test.
The STS-Test categories were not created only as positive or negative to avoid unnecessary anxiety with regard to the disease in the low-risk group. In addition, if the score was created as positive or negative, the patients could be overlooked until a certain cutoff value was reached; subsequently, treatment would be delayed because of a sudden switch to the high-risk group without it being noticed. Therefore, dividing the score into three risk groups was more appropriate because it can help detect any changes over time before switching from the low-risk group to the high-risk group in the long term. In addition, it allows for early diagnosis and intervention when it reaches the medium-risk group from the low-risk group.
Yoon et al. [6] presented a remote spinal examination method and suggested that this methodology will be useful for spine care providers to perform full spine evaluations through telemedicine. Similarly, Piche et al. [17] stated that the virtual spine examination might be comparable to the traditional face-to-face physical examination for low back pain in certain aspects. These studies were usually based on a virtual examination, and our study differs in terms of parent assessment. The STS-Test provides an active role for parents in preventive health services. This new screening tool might be even comparable to the face-to-face physical examination for scoliosis. Literature has suggested that a prediagnosis could be established with various virtual examinations. The combination of the FBT, imaging review, and virtual analysis of the esthetic appearance might sufficiently establish an accurate initial diagnosis in some patients with scoliosis. Iyer et al. [18] stated that telemedicine examination is not meant to replace physical examination but rather serves as a surrogate or marker for findings that are traditionally known for establishing a diagnosis [19]. When deformities such as scoliosis are considered within the growth period, medical consultation every 6 months seems impossible and unnecessary if no sign related to scoliosis is noted, even in the absence of a pandemic. However, scoliosis will still develop despite the lack of signs, because it can develop at any point of time during growth.
This study demonstrates that parents can play an active role as observers in the early detection of scoliosis. The STS-Test might be used in larger groups because it is a user-friendly, cost-effective scoliosis screening test. Furthermore, it might be an alternative to school screening and a beneficial model for health policies.
1. Limitations
One of the study’s limitations is that radiological confirmation could not be performed for everyone to avoid unnecessary radiation exposure. In addition, the STS-Test requires participants who are literate and can use the Internet. The study had a high sociocultural profile. Thus, if the study includes parents with low education levels, the STS-Test’s sensitivity and specificity may be different. Moreover, children below 10 years old may have negatively affected the accuracy because maintaining the desired position during the assessment could be challenging.
2. Strength
This study has contributed to the early diagnosis of scoliosis by increasing awareness among parents. The STS-Test is a highly accurate assessment tool that allows the parents to screen their children periodically because it is time-independent and repeatable at any period throughout the children’s growth. Especially during the COVID-19 pandemic, the risk of scoliosis of children can still be determined by their parents without the need to consult clinicians initially. Although the STS-Test was developed for scoliosis, it provides a perspective for future studies to evaluate other spine and chest deformities.
Conclusions
The STS-Test is a parent-friendly, virtual, cost-effective, result-oriented, reproducible, and reliable new tool for screening scoliosis. It can be easily applied by parents in a short time with high accuracy, either to determine the risk of scoliosis or to observe the spine periodically throughout the children’s growth period.
Notes
Author Contributions
Conception and design, data acquisition, analysis of data, drafting of the manuscript, critical revision, administrative support, and supervision of the preparation of this article: all authors.
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
References
Appendices
Appendix 1 The Scoliosis Tele-Screening Test
Dear participant,
Scoliosis is a three-dimensional deformity that causes asymmetries in the trunk and chest due to deviation of the human spine to the right or left. The risky period for scoliosis is the period when growth continues. For this reason, it is important that parents check their children’s spine in terms of scoliosis risk, especially at the age of 10, and consult a physician in case of scoliosis suspicion. Early diagnosis provides early treatment opportunities for scoliosis. Apply this test to your children in the 7–18 age group who can stand, after completing the test, you can learn your child’s scoliosis risk score by clicking the button. Scoliosis risk will try to be predicted with the score your child receives after this test. The absence of scoliosis in your child as a result of this test does not indicate that scoliosis will not develop. Check your child’s spine regularly every 6 months. If your test score is within the medium or high-risk limits, we recommend that you consult an expert. Do not apply this test to your children diagnosed with neurological diseases or who have undergone spinal surgery.
What is the name and surname of your child? (If you prefer, you can write the initial letter of the name):
How old is your child: ________ ________
Date of Survey: . . ./. . ./. . .
This questionnaire is designed for you to check your child’s spine. Observe your child’s spine from the front, behind, and from the positions described to you, and mark the most appropriate answer.
-
1. Does anyone in your family have scoliosis?
□ No
□ Yes, my child who will be tested, has scoliosis
□ Her/his sibling has
□ Her/his cousins have
-
2. What is the gender of your child?
Girl
Boy
-
3. If your child is a girl, how long has it been since her menarche?
□ She has not yet
□ 1–3 months
□ 3 month–1 year
□ 1–2 years
□ More than 1 year
-
4. When you look at your child from the front, is there any difference between shoulder level?

□ No there is not, shoulders seem equal.
□ Yes, there is. one shoulder is higher than the other.
□ I couldn’t decide.
-
5. When you look at your child from the front, is there any difference between hip level?
□ No there is not, pelvis bone seems equal.
□ Yes, there is. One side is higher than the other.
□ I couldn’t decide.
-
6. When you look at your child from the back is there any difference between shoulder level?
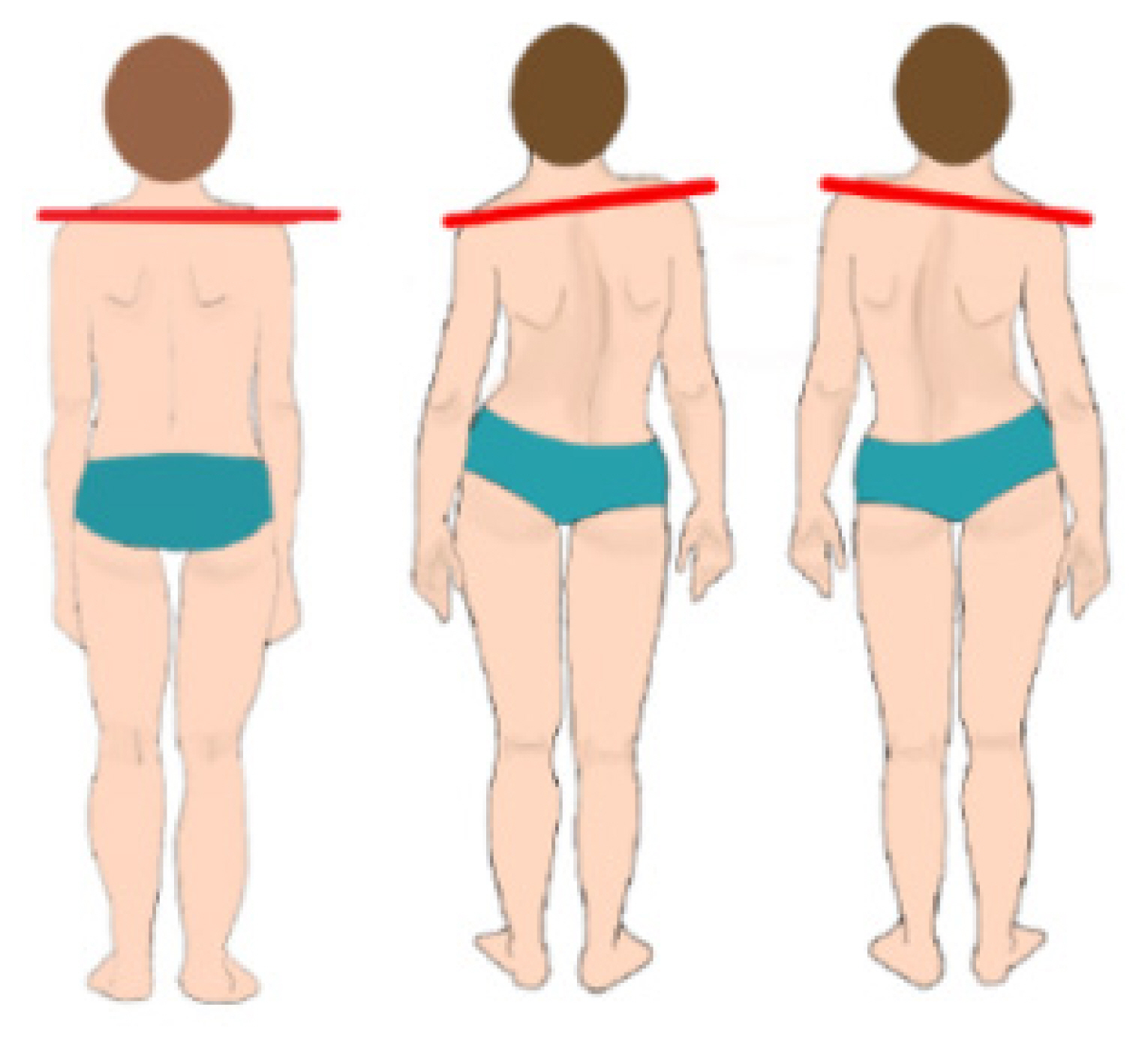
□ No there is not, shoulders seem equal.
□ Yes, there is. One side is higher than the other.
□ I couldn’t decide.
-
7. When you look at your child from the back, is there a difference between end levels of scapula?
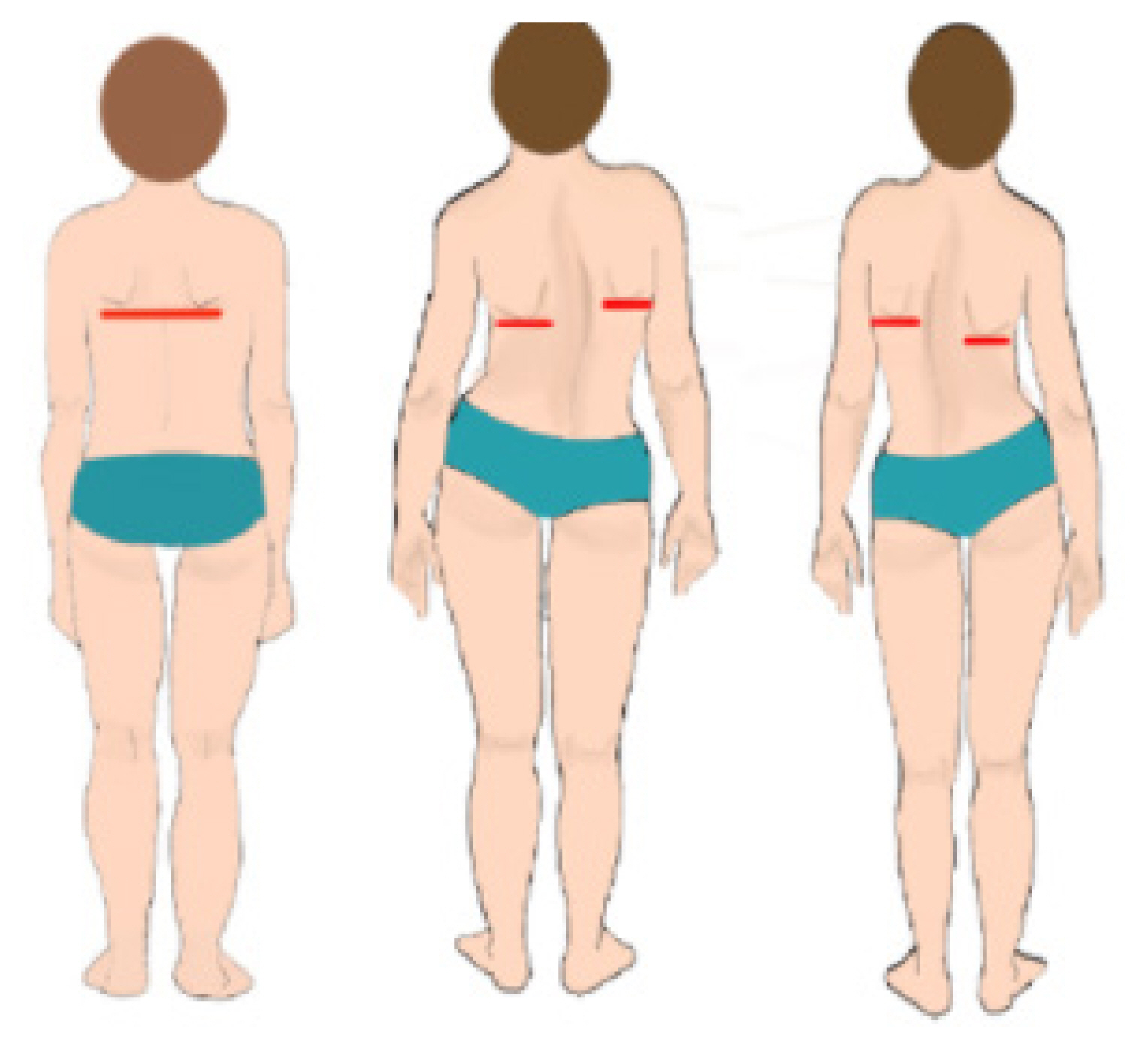
□ No there is not, scapula bone seems equal.
□ Yes, there is. One side is higher than the other.
□ I couldn’t decide.
-
8. When you look at your child from the back, is there a difference between hip levels?
□ No there is not, pelvis bone seems equal.
□ Yes, there is. One side is upper than the other.
□ I couldn’t decide

-
9. When you look at your child from the back, is there a side (lateral) shift on his/her hip?
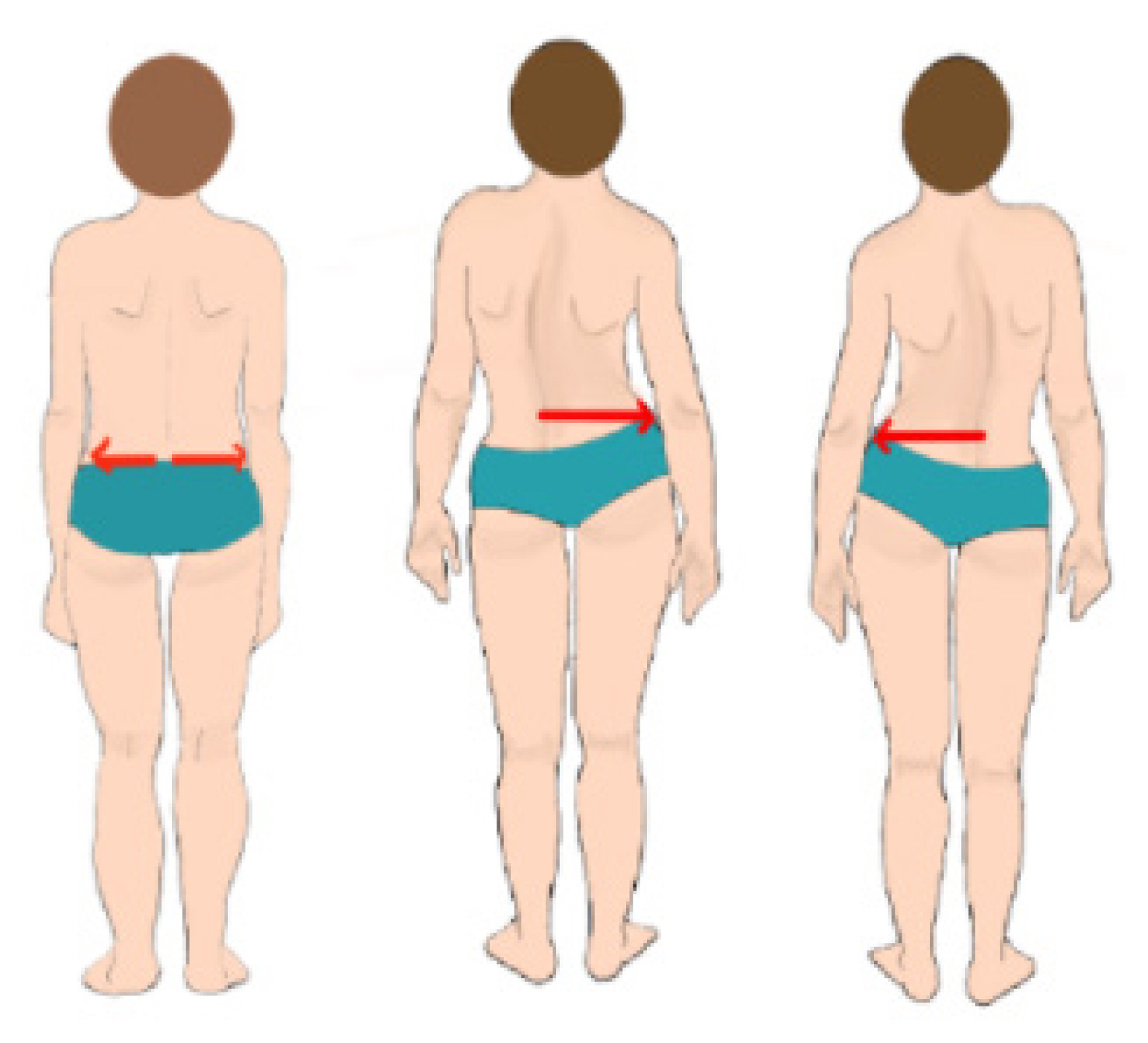
□ No, there is not. The hip seems in the midline.
□ Yes, there is. One hip seems shifted to one side.
□ I couldn’t decide.
-
10. Do you see a prominent rib hump on her/his right or left back side compared to the other side when your child is in the forward bending position? (The forward bending position should be as in the example picture in the upper right corner, with knees straight, the palm of the hands looking forward to each other, and shoulder and knee joint aligned. In this position, the child should be looked or observed from behind).
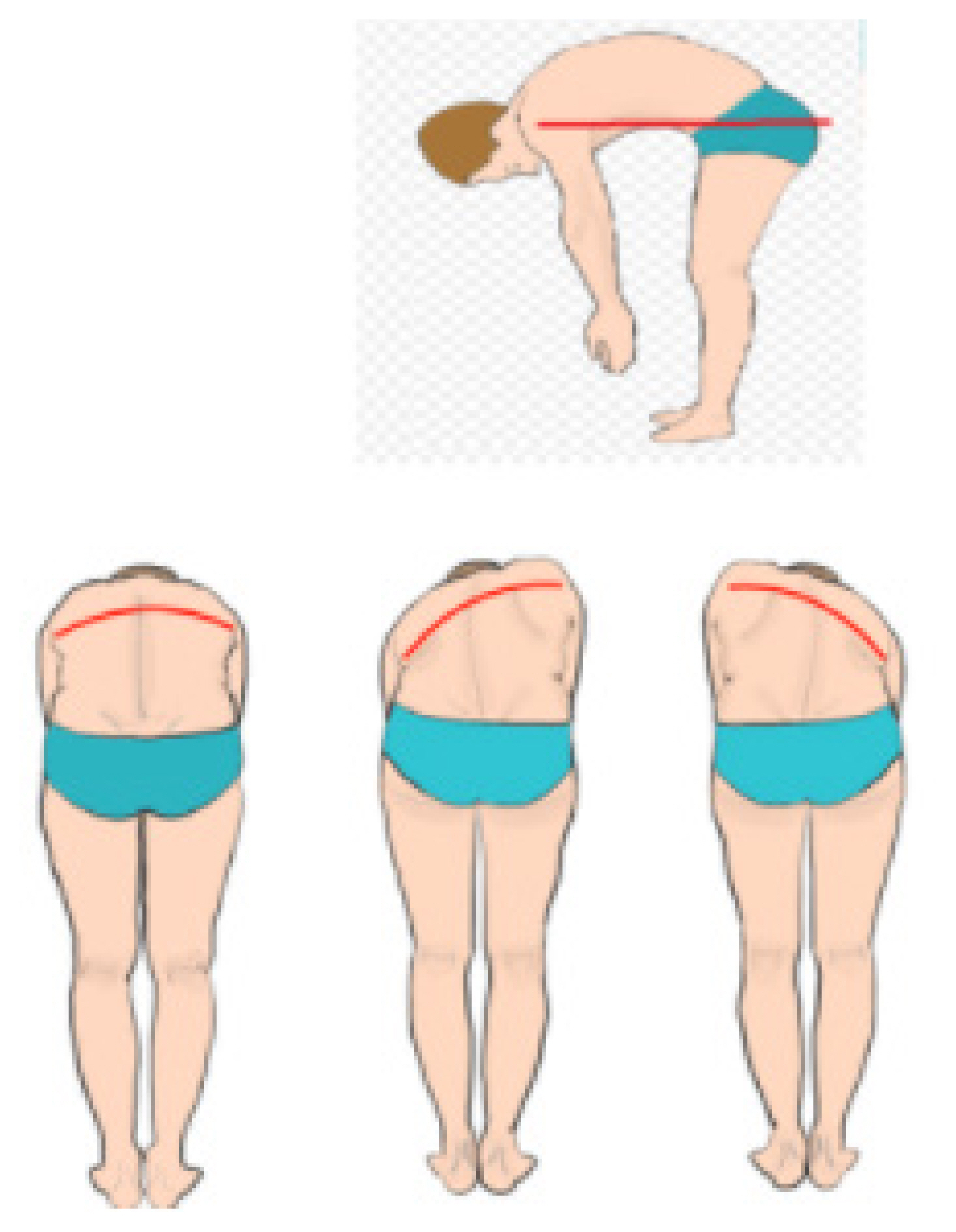
□ No, I cannot see a difference between two side.
□ Yes, there is a hump on one side.
□ I couldn’t decide.