Does Segmental Kyphosis Affect Surgical Outcome after a Posterior Decompressive Laminectomy in Multisegmental Cervical Spondylotic Myelopathy?
Article information
Abstract
Study Design
Retrospective analysis.
Purpose
To compare results of laminectomy in multisegmental compressive cervical myelopathy (CSM) with lordosis versus segmental kyphosis.
Overview of Literature
Laminectomy is an established procedure for decompression in CSM with cervical lordosis. However in patients with segmental kyphosis, it is associated with risk of progression of kyphosis and poor outcome. Whether this loss of sagittal alignment affects functional outcome is not clear.
Methods
We retrospectively reviewed 68 patients who underwent laminectomy for CSM from 1998 to 2009. As per preoperative magnetic resonance images, 36 patients had preoperative lordosis (Group 1) and 32 had segmental kyphosis (Group 2). We studied age at the time of surgery, duration of preoperative symptoms, recovery rate, magnitude of postoperative backward shifting of spinal cord and loss of sagittal alignment.
Results
Mean follow up was 5.05 years (range, 2–13 years) and mean age at the time of surgery 61.88 years. Group 1 had 20 men and 16 women and Group 2 had 19 men and 13 women. Mean recovery rate in Group 1 was 60.32%, in Group 2 was 63.7% without any statistical difference (p-value 0.21, one tailed analysis of variance). Two patients of Group 1 had loss of cervical lordosis by five degrees. In Group 2 seven patients had progression of segmental kyphosis by 5–10 degrees and two patients by more than 10 degrees. Mean cord shift was more in Group 1 (mean, 2.41 mm) as compared to Group 2 (mean, –1.97 mm) but it had no correlation to recovery rate. Patients with younger age (mean, 57 years) and less duration of preoperative symptoms (mean, 4.86 years) had better recovery rate (75%).
Conclusions
Clinical outcome in CSM is not related to preoperative cervical spine alignment. Thus, lordosis is not mandatory for planning laminectomy in CSM. Good outcome is expected in younger patients operated earliest after onset of symptoms.
Introduction
Surgical treatment of multisegmental cervical spondylotic myelopathy (CSM) with segmental kyphosis is controversial. Laminectomy is an established procedure for decompression of the spinal cord in patients with CSM having a lordotic cervical curvature. The proposed mechanism of action is indirect decompression due to a posterior shift of the spinal cord, which may be lessened in patients with segmental kyphosis. Although anterior surgery is a direct mode of decompression that preserves posterior column stability, it is associated with complications and poor fusion rates in multisegmental cervical disease [123]. In addition, it is a high-risk surgery in elderly patients. Thus, the optimal treatment of multisegmental cervical myelopathy with segmental sagittal kyphotic alignment remains controversial. A postoperative backward cord shift is associated with a favorable functional outcome in CSM [45]. It is debatable whether this cord shift is reduced in patients with segmental apical kyphosis. There are many studies both in favor of and against this theory [456789]. The objective of this study was to compare the results of laminectomy in patients with lordotic curvature to those in patients with apical or segmental kyphosis.
Materials and Methods
A total of 170 patients with cervical myelopathy underwent surgery between January 1998 and August 2009 at our center. For surgical planning, supine magnetic resonance sagittal images were examined to determine the cord status, levels involved, and cervical sagittal alignment (Fig. 1). Laminectomy was performed in 90 patients, and 68 patients with a minimum follow-up of two years were included. These patients belonged to type C2 and C3 based on our classification (Fig. 1). Patients classified as type A, B, or C1 who underwent decompression through the anterior approach were excluded as there is sufficient evidence in the literature to support this management protocol. Our study population of 68 patients was divided into two groups: 36 patients with preoperative lordotic cervical curvature (Group 1) (Fig. 2A) and 32 patients with segmental apical kyphosis and an overall lordotic curvature (Group 2) (Fig. 2B). The study population comprised 60 males and 8 females. C3–C7 laminectomy was performed in 61 patients, C3–D1 in 6 patients, and C3–D2 in 1 patient. Twenty-nine patients had simultaneously undergone an additional thoracic or lumbar decompression.
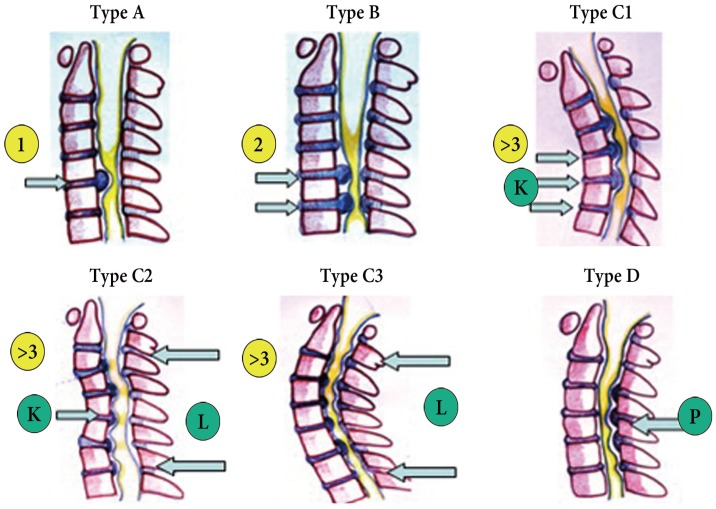
Colored hand drawing. Classification of cervical myelopathy based on levels of compression and sagittal cervical alignment in supine magnetic resonance images. Type A, one level of anterior compression; Type B, two levels of anterior compression; and Type C, three or more levels (multisegmental) of anterior compression. Type C is divided into three subtypes based on sagittal alignment: C1, complete kyphotic curve; C2, segmental kyphosis with overall lordosis; C3, complete lordosis; Type D, posterior compression. K, apical kyphosis; L, lordosis; P, posterior.

Grayscale image. (A) Group 1, patients with complete lordosis. (B) Group 2, patients with segmental apical kyphosis with overall lordosis.
All patients had undergone conventional laminectomy in the prone position with a standard midline incision. The laminectomy extended laterally to the junction of the lamina and the lateral mass. The C2 spinous process and its muscle attachments were preserved in most patients, with undercutting performed in only seven patients. All patients were mobilized on postoperative day two or three with the mandatory use of a soft cervical collar for a minimum of three months. At three months postoperatively, a magnetic resonance scan was performed to assess the adequacy of decompression. Subsequently, plain radiographs were performed yearly to assess potential changes in cervical alignment and stability.
1. Clinical evaluation
Japanese Orthopaedic Association (JOA) scores [3] were assessed preoperatively and at the last follow-up appointment, and recovery rates were calculated using Hirabayashi's formula [10]. Demographic parameters such as age, sex, and the duration of preoperative symptoms were obtained from the patients' records.
2. Radiographic evaluation
Using the Surgimap software, the minimal distance between the posterior margin of the C5 vertebral body and the anterior margin of the spinal cord (body-to-cord distance) was measured in T2-weighted mid-sagittal magnetic resonance images. The extent of posterior cord shift was calculated (millimeters) as the difference between the postoperative and preoperative body-to-cord distance [7]. Cervical alignment (Cobb's angle) was calculated from preoperative and last follow-up radiographs, obtained in the neutral position, by measuring the angle between lines from the inferior end plate of C2 to the superior end plate of C7 [8].
3. Statistical analysis
Pearson's correlation coefficient test was used for statistical analysis of the data, and significance levels of 95% or better were considered acceptable.
Results
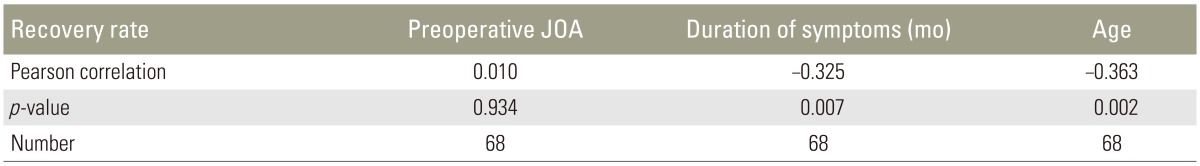
The mean follow-up period was 5.05 years (range, 2–13 years), and the mean age of the patients at the time of surgery was 61.88 years (range, 41–81 years). The overall mean recovery rate was 61.92%. There were no statistical differences in recovery rates between groups 1 and 2 (p=0.21, one-tailed analysis of variance). The mean duration of preoperative symptoms was 5.73 months (range, 1–12 months). Younger patients (age <57 years, n=48) and patients with a short duration of preoperative symptoms (<4 months) had an improved mean recovery rate (75%). The mean preoperative JOA scores in groups 1 and 2 were 10 and 10.21, respectively (p=0.934), and the mean postoperative JOA scores in the two groups were 14.9 and 14.4, respectively (p=0.86). Patients with preoperative JOA scores of >10 (36 patients) had a significantly better mean recovery rate than those with JOA scores of <10 (28 patients) (68.8% vs. 54.8%; p=0.023). Long duration of symptoms before surgery and an age of <57 years negatively correlated with the recovery rate, whereas there was a positive correlation between a high preoperative JOA score and the recovery rate (Tables 1, 2) (Fig. 3).

Masterchart showing gender distribution, operated levels, clinical and radiological results of Group 1 and Group 2
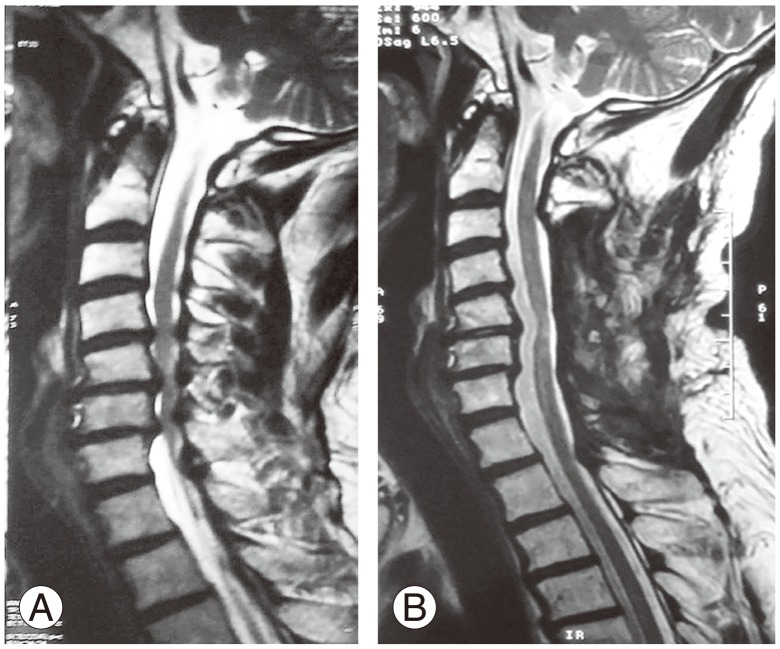
Grayscale image. (A) Preoperative T2-weighted sagittal magnetic resonance image of a 58-year-old male, showing spinal cord compressions at C4–C7. Sagittal alignment shows segmental apical kyphosis with overall lordosis. (B) Postoperative magnetic resonance image of the same patient taken four months after laminectomy, demonstrating successful decompression of the spinal cord. The magnitude of postoperative backward shifting of the spinal cord was 1.5 mm. The Japanese Orthopaedic Association score was 15.5 and the recovery rate was 75%.
In Group 1, two patients (5.5%) had a reduction in cervical lordosis by 5° and none developed kyphosis. In Group 2, seven patients had progression to cervical kyphosis with a change in alignment of 5°–10° and two patients had progression to kyphosis with a change of more than 10° (nine patients, 28.1%) (Fig. 4). Overall, 11 patients (16.1%) had a change in alignment of ≥5°. The extent of postoperative cord shift appeared to be higher in Group 1 than in Group 2; however, this correlation was not statistically significant (p=0.158).
Discussion
The selection of a surgical approach in multisegmental cervical myelopathy is still controversial. Preoperative cervical alignment plays a key role in surgical planning. Although laminectomy is an established procedure for patients with a lordotic cervical curvature, its role in patients with segmental kyphosis has been debated. Laminectomy results in the indirect decompression of the spinal cord through a posterior cord shift. Postoperative backward shifting of the cord is considered to be one of the most important indicators of adequate decompression, and its relation to preoperative cervical alignment has been reported in the literature [57911]. The impact of preoperative cervical lordosis on cord shift is a matter of discussion [458]. Similarly, it is controversial whether the extent of the postoperative cord shift affects the clinical outcome [45678911]. However, no study has compared cord shift in patients with differential preoperative cervical alignments (apical kyphosis vs. lordosis). Apical kyphosis refers to the presence of kyphosis between the C2 and C7 end plates in the middle of an overall lordotic alignment. Thus, there is a bowstring-like effect allowing sufficient posterior cord shift. Although Group 2 patients have segmental kyphosis, there were no statistical differences in cord shift measurements between the two groups. This may be because both groups have an overall lordotic curvature, which likely determines the cord shift. Postoperative magnetic resonance images showed a good posterior cord shift and the presence of adequate anterior CSF sleeve in all patients in our study. This is supported by a study by Chiba et al. [12], which suggested that the cervical cord, even in an apical kyphotic spine, has a “slack,” allowing for decompression and neurological recovery. On the contrary, Breig and el-Nadi [13] suggested that there is a deficit in spondylotic myelopathy due to the draping of the cord over the vertebral body, leading to decreased blood supply to the cord. We believe that the radiological evidence of cord shift and reappearance of the anterior CSF sleeve contradict those findings.
Laminectomy is considered to be associated with the loss of cervical alignment and progression of kyphosis. This progression is considered to be more common severe in patients with preoperative kyphotic cervical alignment [14]. It is debatable whether this is associated with poor functional outcome. Based on a literature review, Ryken et al. [15] concluded that although there is a greater risk of the loss of lordosis in patients with a preoperative straight or kyphotic cervical alignment, its association with the functional outcome could not be established. Uchida et al. [14] found no difference in the functional outcome between anterior surgery and laminectomy for patients with CSM having a preoperative kyphotic alignment. They reported a mean recovery rate of 61.5%, which is comparable to our data. Kaptain et al. [16] studied the outcome of laminectomy in patients with cervical myelopathy having lordotic, straight, or kyphotic cervical curvatures. They found that 14% of their patients with lordosis and 30% of their patients with a straight cervical alignment had a loss of alignment and progressed toward kyphosis; however, this did not have any impact on the functional outcome. Similar results have been reported by Kato et al. [17].
While Group 2 patients had a significant loss of cervical alignment in our study, only 16.1% of the total patients had a loss of cervical alignment of ≥5°. This supports the notion that degenerated spines in elderly patients are inherently stable due to anterior osteophytes, ossified ligaments, and degenerated discs [18]. In recent years, laminoplasty with cervical alignment restoration has been preferred over laminectomy due to the risk of developing post-laminectomy kyphosis [3192021]. However, its effectiveness in achieving better functional outcomes has not been reported [3141619222324].
The association of functional outcome with preoperative JOA scores, age, and duration of preoperative symptoms has been extensively established in the literature [252627], and our study demonstrated similar results.
Although a lot of work has been done on evaluating various factors affecting the outcome of surgery in CSM, strategies for deciding a surgical approach have not been studied, and the surgical approach is highly dependent on the surgeon's experience. Although plain radiographs help guide the surgical approach based on alignment, the aim of surgery is to decompress the spinal cord. Therefore, the sagittal morphology of the cord seen on the magnetic resonance image (apical kyphosis vs lordosis) is more useful in decision-making.
The practical classification used for CSM is based on the sagittal morphology of the spinal cord and helps guide the approach to CSM management.
Conclusions
Cervical laminectomy for CSM provides good radiological and functional outcomes in the presence of apical kyphosis with overall lordosis. Functional outcomes in CSM do not necessarily correlate with sagittal plane alignment. Young age (less than 57 years), preoperative JOA scores of >10, and shorter duration of symptoms are the most important predictors of good neurological recovery.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.