|
 |
- Search
| Asian Spine J > Volume 11(6); 2017 > Article |
|
Abstract
Purpose
To assess the surgical outcomes of posterior decompression and fusion for cervical myelopathy in patients with athetoid cerebral palsy.
Overview of Literature
Patients with athetoid cerebral palsy demonstrate involuntary movements and develop severe cervical spondylosis with kyphosis. In these patients, surgery is often performed at an early age because of myelopathy. A few studies have reported about the long-term outcomes of surgical treatment; however, they contain insufficient information.
Methods
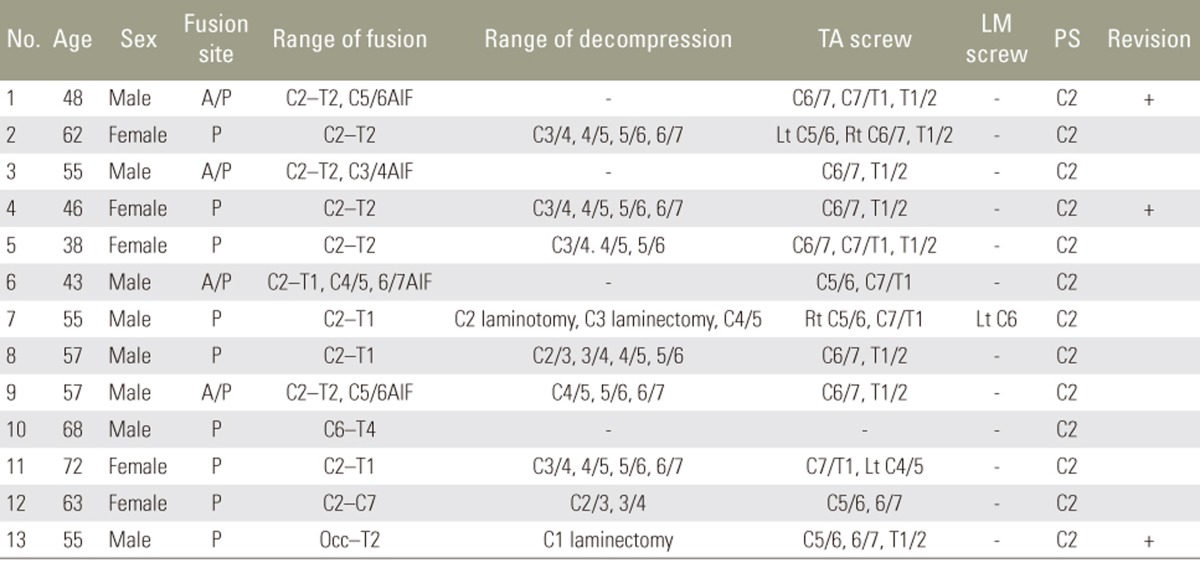
From 2003 to 2008, 13 patients with cervical myelopathy due to athetoid cerebral palsy underwent posterior fusion surgery and were included in this study. The Japanese Orthopaedic Association (JOA) score, neck disability index (NDI), C2–7 angle on radiography, and need for additional surgical treatment were examined at 1 and 5 years postoperatively.
Results
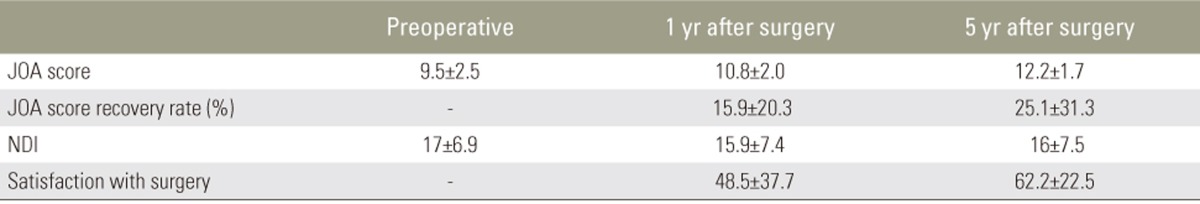
The mean C2–7 angle was −10.5°±21.1° preoperatively and was corrected to −2.9°±13.5° immediately postoperatively. This improvement was maintained for 5 years. The JOA score was 9.5±2.5 preoperatively and 12.2±1.7 at the 5-year follow-up. NDI was 17±6.9 preoperatively and 16±7.5 at the 5-year follow-up. Patient satisfaction with surgery on a 100-point scale was 62.2±22.5 at the 5-year follow-up. Three patients needed additional surgery for loosening of screws. These results demonstrate good surgical outcomes for posterior fusion at 5 years.
Patients with athetoid cerebral palsy demonstrate involuntary movements and develop severe cervical spondylosis with kyphosis [123456]. Because cervical spondylosis progresses at a young age in patients with athetoid cerebral palsy, they suffer from cervical myelopathy in their 30s or 40s. Decompression surgery, such as laminectomy or laminoplasty, is required to treat cervical myelopathy. However, it is difficult to treat cervical myelopathy with a kyphotic deformity of the cervical spine by decompression alone. Furthermore, if decompression alone is performed in patients with athetoid cerebral palsy, postoperative kyphosis of the cervical spine can occur. Therefore, anterior or posterior fixation with instrumentation has been used for patients with cervical myelopathy with athetoid cerebral palsy [7891011]. Once fixation with instrumentation is performed, careful observation is needed for implant failure and adjacent segment disease because of involuntary neck movement [12]. It is also possible for activities of daily living to deteriorate because of the decreased range of motion of the cervical spine after long instrumentation. A long-term follow-up study showed a high incidence of the progression of deformity and neurological deterioration [12]. Another report of long-term follow-up over 10 years showed that surgical results at the most improved period were good or excellent with any type of surgery, including anterior decompression and fusion, laminectomy, and laminoplasty with or without fusion [13]. However, most patients showed late neurological deterioration from 8 to 13 years postoperatively, largely because of progressive deformity [13]. In these patients, surgery is often performed at an early age. Therefore, long-term follow-up is very important. A few studies have reported about the long-term outcomes of surgical treatment; however, they contain insufficient information. There are many problems that need to be clarified for the treatment for this patient group. Various surgical procedures have been described in the literature, but which procedure is appropriate for this patient group, including the type and range of instrumentation, is still unknown. It is necessary to evaluate the long-term results of surgical treatment for this patient group. The purpose of this study was to report the surgical outcomes of cervical myelopathy with athetoid cerebral palsy.
This study protocol was approved by the Ethics Committee of Fukushima Medical University (approval no. 2592). Before surgery, informed consent was obtained from each patient. In the Department of Orthopaedic Surgery, Fukushima Medical University, instrumented fusion was performed for cervical myelopathy with athetoid cerebral palsy since 2003, following a period of performing decompression alone. The subjects were 13 consecutive patients (eight males and five females) with cervical myelopathy and athetoid cerebral palsy who underwent decompression and instrumented fusion from 2003 to 2008 (Table 1). Their mean age was 55.3 years (range, 38–72 years). The magnitude of involuntary neck movements was moderate; physicians could control their neck movement by hands for all patients. All patients were independently performing activities of daily living. Surgical procedures were performed in four patients with anterior-posterior fusion and in nine patients with posterior fusion alone. Anterior decompression and fusion with posterior fixation were performed for the initial four cases to obtain rigid fixation. After the initial period, only posterior procedures were performed for the last nine cases. The range of fusion was C2–Th2 (seven cases), C2–Th1 (three cases), C2–7 (one case), C6–Th4 (one case), and occiput–Th2 (one case). We usually select C2 for caudal level. For costal level, if there is degenerative change or instability between C7 and T1, we select T1 or T2. Posterior segmental partial laminectomy [14] was performed for decompression of the cord at neurologically symptomatic levels. In all cases, instrumentation was inserted only for posterior fusion using the Olerud cervical fixation system (Anatomica AB, Askim, Sweden). For external fixation, a sternal-occipital-mandibular immobilization (SOMI) brace and a cervical collar were used for 2 months and 1 month, respectively, in the initial four cases. No orthosis or cervical collar was used for the last nine cases. The Japanese Orthopaedic Association (JOA) scoring system [15] was used to evaluate patient neurological status, and the Hirabayashi's method [16] was used to calculate the recovery rate. The neck disability index (NDI) [171819] was used to evaluate neck symptoms. The patients' satisfaction with the surgical results was noted at follow-up (ranging from 0 [not satisfied] to 100 [completely satisfied]). Sagittal alignment of the cervical spine was evaluated by the C2–7 sagittal Cobb angle on lateral X-ray examination. Evaluations were performed preoperatively and 1 and 5 years postoperatively.
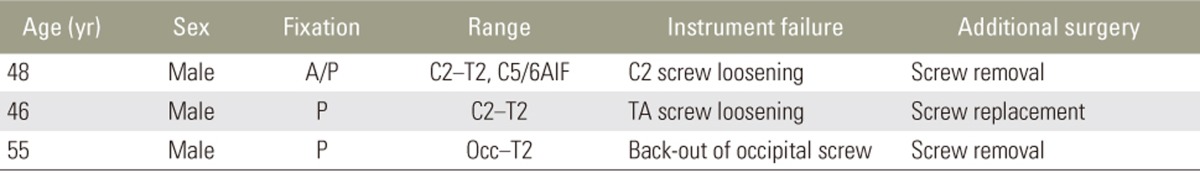
The mean operative time was 304±52 minutes (356±24 minutes with the combined anterior and posterior procedure and 246±23 minutes with the posterior procedure alone), and the mean intraoperative blood loss was 661±200 g (751±246 g with the combined anterior and posterior procedure and 417±110 g with the posterior procedure alone). Preoperatively, the mean C2–7 sagittal Cobb angle was −10.5°±21.1° on X-ray, indicating kyphosis. The C2–7 angle was corrected to −2.9°±13.5° immediately postoperatively, and it was −3.6°±12.3° at the 1-year follow-up. The correction was maintained for 5 years (Fig. 1). There was no adjacent segment disease during the 5-year follow-up period. The mean JOA score was 9.5±2.5 points preoperatively, 10.8±2.0 points at the 1-year follow-up, and 12.2±1.7 points at the 5-year follow-up (Table 2). The recovery rate of the JOA score was 15.9% at the 1-year follow-up and 25.1% at the 5-year follow-up. The JOA score was slightly improved postoperatively and was maintained for 5 years. The mean NDI score was 17±6.9 preoperatively, 15.9±7.4 at the 1-year follow-up, and 16±7.5 at the 5-year follow-up (Table 2). NDI showed no remarkable changes postoperatively. The NDI results indicate that fixation of the cervical spine resulted in little deterioration of the neck symptoms. Patient satisfaction with surgery on a 100-point scale was 48.5±37.7 at the 1-year follow-up and 62.2±22.5 at the 5-year follow-up (Table 2). Additional surgeries were needed for three patients (Table 3). In one patient, loosening of a Th1/2 transarticular screw was observed on postoperative day 26, and this screw was then replaced by a Th2/3 transarticular screw. In another patient, loosening of an occipital screw was observed, and this screw was then replaced on postoperative day 51. However, the screw backed out again and was removed 6 days after the second surgery. In another patient, loosening of the C2 pars screw was observed, and this screw was then removed 2 years after the initial surgery. All patients recovered after the additional surgery for loosened screw removal or screw replacement. Finally, bony fusion was observed in all patients based on reconstructed computed tomography findings 1 year postoperatively, except for the patient with C2 screw loosening. In patients with C2 screw loosening, bony union was also observed 2 years after the C2 screw removal.
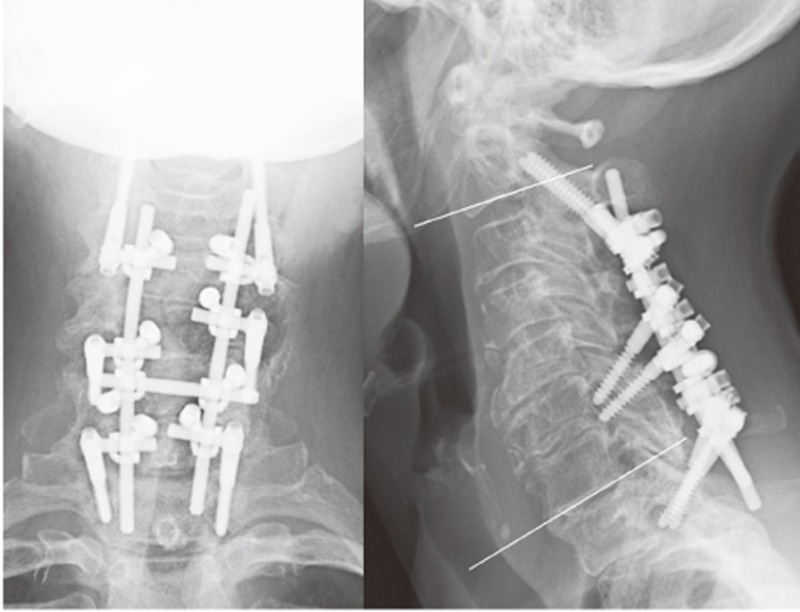
A 62-year-old woman with athetoid cerebral palsy experienced numbness in both hands and disturbance in walking, with worsening symptoms. She was diagnosed with cervical myelopathy based on neurological findings and imaging studies. On X-ray examination, the preoperative C2–7 angle was −4.6°, indicating slight kyphosis (Fig. 2). The preoperative JOA score was 9 points, and the NDI score was 10 points. Posterior fusion from C2 to T2 using a C2 pars screw and rt C5/6, lt C6/7, and bil T1/T2 transarticular screws with segmental partial laminectomy [14] at C3–4, C4–5, C5–6, and C6–7 was performed (Fig. 3). Operative time was 268 minutes, and intraoperative blood loss was 410 g. Five years postoperatively, the C2–7 angle was 18.5°, indicating lordosis. The JOA score was 11 points, and the recovery rate of the JOA score was 25%. The NDI score was 10 points, and patient satisfaction with surgery was 70/100.
In this study, the 5-year surgical outcomes of cervical myelopathy with athetoid cerebral palsy were presented based on X-ray findings and clinical evaluation. At the 5-year follow-up, X-ray findings showed that the alignment of the cervical spine was maintained without severe implant failure. The JOA score showed slight recovery postoperatively. The recovery rate of the JOA score was only 25.1% at the 5-year follow-up. This does not seem to indicate adequate improvement, but it is difficult to evaluate the condition of these patients by the JOA score alone because of the symptoms that originate from the athetoid cerebral palsy itself. This scoring system does not evaluate involuntary movements, such as athetosis, in patients with cerebral palsy. The JOA score is a reliable tool for the evaluation of functional status of compressive cervical myelopathy [15]. However, some authors have pointed out the limitations of the JOA score for the evaluation of patients with cervical myelopathy with athetoid cerebral palsy [2021]. Therefore, not only the JOA score but also other clinical evaluations are needed for the accurate evaluation of this patient group. In the present study, the neck symptoms were evaluated using NDI. The mean preoperative NDI score was 17, indicating moderate-to-severe disability. The NDI score did not change for 5 years postoperatively. This finding indicated that the patients' neck symptoms were not improved postoperatively, even though the kyphosis was slightly corrected. On the other hand, fusion surgery decreased the range of motion of the cervical spine, which was possibly followed by deterioration of neck function. As a result, NDI could not detect any changes in their neck symptoms after cervicothoracic fusion surgery. NDI does not include any items about involuntary neck movement. Therefore, NDI may have limitations when evaluating neck symptoms of patients with athetoid cerebral palsy. In addition to the JOA score and NDI, patient satisfaction with surgery was simply evaluated using a 100-point numerical rating scale, and it was over 50. This finding indicates that the patients were satisfied with their condition 5 years postoperatively, even if other tools did not show any improvement.
Pedicle screws are often used for the cervical spine as a strong anchor [22]. For patients with cervical myelopathy with athetoid cerebral palsy, posterior fixation with pedicle screw methods has been reported to be effective [2023]. On the other hand, the possibility of injury to the vertebral artery by a pedicle screw cannot be omitted. Cervical spondylosis, including that in patients with cerebral palsy, is a risk factor for perforation by a pedicle screw [24]. In the present patients, transarticular screws [2526] were inserted at the middle to lower cervical spine and the upper thoracic spine. The pullout strength of the transarticular screw is superior to that of the lateral mass screw [27]. As a result, cervical alignment was maintained for 5 years with transarticular screws, indicating that transarticular screws are one of the options for posterior fixation. For the correction of cervical deformity in patients with athetoid cerebral palsy, combined anterior and posterior fusion has been reported to be effective [7891011]. In our institute, anterior-posterior fusion was performed for the initial four patients. After that, only posterior procedures were performed for this patient group. The results of this study indicate that kyphosis was corrected by the posterior procedure alone with transarticular screws, and correction was maintained for 5 years similar to the anterior-posterior fusion. It should be noted that the present patients had relatively low-grade involuntary neck movement. It is possible that patients with more severe neck movement would need anterior fusion.
Major complications after posterior fusion surgery were loosening of the implant, pain due to the implant, and adjacent segment disease. Postoperative treatment, such as cervical orthosis or botulinum toxin injection, may reduce complications, thereby preventing instrument failure. However, it remains to be determined whether these postoperative therapies are needed. In this series, a SOMI brace was used as a postoperative external orthosis for only four patients. For other patients, no orthosis was used postoperatively because putting on the brace is difficult for patients with athetoid cerebral palsy and they find it very uncomfortable. In three patients without an orthosis, screw loosening occurred. Given this finding, a SOMI brace might reduce screw loosening postoperatively. In general, a halo vest has sometimes been reported to provide rigid external fixation. On the other hand, Furuya et al. [23] reported that pedicle screw fixation was strong enough to require a halo vest. Furthermore, the incidence of halo vest-related complications was relatively high [27]. Therefore, we do not use a halo vest as a postoperative orthosis. Involuntary neck movement is one of the causes of instrument failure. Therefore, controlling involuntary movement could help prevent these complications. Muscle release is another option for controlling involuntary movement. Ueda et al. [28] reported that laminoplasty with muscle release showed good results at the 1-year follow-up. Botulinum toxin injection is widely used to decrease spasticity and involuntary movements. Furuya et al. [23] and Jameson et al. [21] reported cases of preoperative botulinum toxin injection. Botulinum toxin injection was not administered in the present series because the patients showed relatively low-grade involuntary neck movement. It may reduce instrument failure for patients with more severe involuntary neck movement. The degree of involuntary movements is an important factor related to patient outcomes. In the present series, there were no patients with severe athetosis that could not be controlled by the patients' hands. All patients independently performed activities of daily living. Therefore, we considered that extensive postoperative immobilization with a halo vest or additional treatment, such as botulinum toxin injection or muscle release, was unnecessary for our patients. For postoperative rehabilitation in this series, we provided general postoperative rehabilitation similar to that provided for other patients with myelopathy even though they had athetoid cerebral palsy. It is possible that the results may be different for patients with much more severe involuntary movements. Some long-term follow-up studies showed instrument failure and adjacent segment instability after fusion surgery [1220]. In the present study, surgical improvement on the JOA score and alignment of the cervical spine were maintained for 5 years. Three patients needed additional surgery for screw loosening, but no patients had adjacent segment disease over the 5-year follow-up period in this series. However, Azuma et al. [13] reported that late neurological deterioration and cervical spinal deformity progressed over 10 years. Therefore, a much longer follow-up period, over 10 years, is needed in future studies.
In conclusion, posterior decompression and fusion for patients with cervical myelopathy with athetoid cerebral palsy showed results as good as those for combined anterior-posterior surgery at the 5-year follow-up. Posterior decompression and fusion using transarticular screws were found to be effective for patients with cervical myelopathy with athetoid cerebral palsy.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
1. Anderson WW, Wise BL, Itabashi HH, Jones M. Cervical spondylosis in patients with athetosis. Neurology 1962 12:410–412. PMID: 13861319.


2. McCluer S. Cervical spondylosis with myelopathy as a complication of cerebral palsy. Paraplegia 1982 20:308–312. PMID: 7177698.


3. Nishihara N, Tanabe G, Nakahara S, Imai T, Murakawa H. Surgical treatment of cervical spondylotic myelopathy complicating athetoid cerebral palsy. J Bone Joint Surg Br 1984 66:504–508. PMID: 6746682.


4. Fuji T, Yonenobu K, Fujiwara K, et al. Cervical radiculopathy or myelopathy secondary to athetoid cerebral palsy. J Bone Joint Surg Am 1987 69:815–821. PMID: 3597493.


5. Kidron D, Steiner I, Melamed E. Late-onset progressive radiculomyelopathy in patients with cervical athetoid-dystonic cerebral palsy. Eur Neurol 1987 27:164–166. PMID: 3622589.


6. Harada T, Ebara S, Anwar MM, et al. The cervical spine in athetoid cerebral palsy: a radiological study of 180 patients. J Bone Joint Surg Br 1996 78:613–619. PMID: 8682830.


7. Mikawa Y, Watanabe R, Shikata J. Cervical myelo-radiculopathy in athetoid cerebral palsy. Arch Orthop Trauma Surg 1997 116:116–118. PMID: 9006780.


8. Epstein NE. Circumferential cervical surgery for spondylostenosis with kyphosis in two patients with athetoid cerebral palsy. Surg Neurol 1999 52:339–344. PMID: 10555838.


9. Onari K. Surgical treatment for cervical spondylotic myelopathy associated with athetoid cerebral palsy. J Orthop Sci 2000 5:439–448. PMID: 11180900.


10. Onari K, Kondo S, Mihara H, Iwamura Y. Combined anterior-posterior fusion for cervical spondylotic myelopathy in patients with athetoid cerebral palsy. J Neurosurg 2002 97:13–19. PMID: 12120637.


11. Haro H, Komori H, Okawa A, Shinomiya K. Surgical treatment of cervical spondylotic myelopathy associated with athetoid cerebral palsy. J Orthop Sci 2002 7:629–636. PMID: 12486465.


12. Kim KN, Ahn PG, Ryu MJ, et al. Long-term surgical outcomes of cervical myelopathy with athetoid cerebral palsy. Eur Spine J 2014 23:1464–1471. PMID: 24337359.


13. Azuma S, Seichi A, Ohnishi I, Kawaguchi H, Kitagawa T, Nakamura K. Long-term results of operative treatment for cervical spondylotic myelopathy in patients with athetoid cerebral palsy: an over 10-year follow-up study. Spine (Phila Pa 1976) 2002 27:943–948. PMID: 11979166.


14. Otani K, Sato K, Yabuki S, Iwabuchi M, Kikuchi S. A segmental partial laminectomy for cervical spondylotic myelopathy: anatomical basis and clinical outcome in comparison with expansive open-door laminoplasty. Spine (Phila Pa 1976) 2009 34:268–273. PMID: 19179921.


15. Yonenobu K, Abumi K, Nagata K, Taketomi E, Ueyama K. Interobserver and intraobserver reliability of the Japanese Orthopaedic Association scoring system for evaluation of cervical compression myelopathy. Spine (Phila Pa 1976) 2001 26:1890–1894. PMID: 11568701.


16. Hirabayashi K, Miyakawa J, Satomi K, Maruyama T, Wakano K. Operative results and postoperative progression of ossification among patients with ossification of cervical posterior longitudinal ligament. Spine (Phila Pa 1976) 1981 6:354–364. PMID: 6792717.


17. Vernon H. The Neck Disability Index: state-of-the-art, 1991-2008. J Manipulative Physiol Ther 2008 31:491–502. PMID: 18803999.


18. Nakamaru K, Vernon H, Aizawa J, Koyama T, Nitta O. Crosscultural adaptation, reliability, and validity of the Japanese version of the neck disability index. Spine (Phila Pa 1976) 2012 37:E1343–E1347. PMID: 22789978.


19. Takeshita K, Hosono N, Kawaguchi Y, et al. Validity, reliability and responsiveness of the Japanese version of the Neck Disability Index. J Orthop Sci 2013 18:14–21. PMID: 22945912.


20. Demura S, Murakami H, Kawahara N, Kato S, Yoshioka K, Tsuchiya H. Laminoplasty and pedicle screw fixation for cervical myelopathy associated with athetoid cerebral palsy: minimum 5-year follow-up. Spine (Phila Pa 1976) 2013 38:1764–1769. PMID: 23759815.


21. Jameson R, Rech C, Garreau de. Cervical myelopathy in athetoid and dystonic cerebral palsy: retrospective study and literature review. Eur Spine J 2010 19:706–712. PMID: 20066444.



22. Abumi K, Shono Y, Taneichi H, Ito M, Kaneda K. Correction of cervical kyphosis using pedicle screw fixation systems. Spine (Phila Pa 1976) 1999 24:2389–2396. PMID: 10586466.


23. Furuya T, Yamazaki M, Okawa A, et al. Cervical myelopathy in patients with athetoid cerebral palsy. Spine (Phila Pa 1976) 2013 38:E151–E157. PMID: 23132539.


24. Uehara M, Takahashi J, Hirabayashi H, et al. Perforation rates of cervical pedicle screw insertion by disease and vertebral level. Open Orthop J 2010 4:142–146. PMID: 20448816.



25. Xu R, Zhao L, Chai B, et al. Lateral radiological evaluation of transarticular screw placement in the lower cervical spine. Eur Spine J 2009 18:392–397. PMID: 19130097.



26. Liu G, Xu R, Ma W, Sun S, Feng J. Anatomical considerations for the placement of cervical transarticular screws. J Neurosurg Spine 2011 14:114–121. PMID: 21166487.


27. Klekamp JW, Ugbo JL, Heller JG, Hutton WC. Cervical transfacet versus lateral mass screws: a biomechanical comparison. J Spinal Disord 2000 13:515–518. PMID: 11132983.


28. Lee YJ, Chung DS, Kim JT, Bong HJ, Han YM, Park YS. Surgical treatments for cervical spondylotic myelopathy associated with athetoid cerebral palsy. J Korean Neurosurg Soc 2008 43:294–299. PMID: 19096635.



29. Ueda Y, Yoshikawa T, Koizumi M, et al. Cervical laminoplasty combined with muscle release in patients with athetoid cerebral palsy. Spine (Phila Pa 1976) 2005 30:2420–2423. PMID: 16261119.


Fig. 1
A graph showing the mean C2–7 angle from preoperatively to 5 years postoperatively. The C2–7 sagittal Cobb angle is −10.5°±21.1° preoperatively. It is −2.9°±13.5° on X-ray 1 week postoperatively, −3.6°±12.3° at the 1-year follow-up, and −3.5°±10.2° at the 5-year follow-up. post op, postoperative.
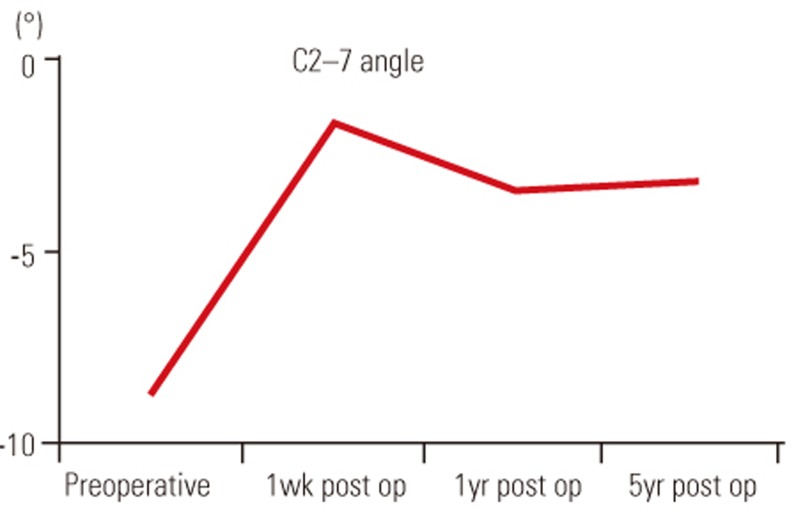
Fig. 2
Preoperative X-ray findings of the cervical spine. The white lines indicate the C2 and C7 endplates. The C2–7 angle is −4.6°, indicating slight kyphosis.

Fig. 3
X-ray findings at the 5-year follow-up. Posterior fixation was performed from C2 to T2, with a C2 pars screw and right C5/6, left C6/7 and both side of T1/T2 transarticular screws, in addition to C3–4, C4–5, C5–6, and C6–7 segmental partial laminectomy. The white lines indicate C2 and C7 endplates. The C2–7 angle is 18.5°, indicating that lordosis was postoperatively achieved.