Analysis of Revision Surgery of Microsurgical Lumbar Discectomy
Article information
Abstract
Study Design
A retrospective study.
Purpose
Our objectives were to determine the association between the pathological changes of disc herniation and the interval between primary and revision surgeries and to investigate the frequency and site of the dural laceration in the primary and revision surgeries.
Overview of Literature
Among 382 patients who underwent microsurgical lumbar discectomy, we investigated 29 who underwent revision surgery to analyze recurrent herniation pathologies and complications to determine the manner in which lumbar disc herniation can be more efficiently managed.
Methods
Of 29 patients, 22 had recurrent disc herniation at the same level and site. The pathological changes associated with compression factors were classified into the following two types depending on intraoperative findings: (1) true recurrence and (2) minor recurrence with peridural fibrosis (>4 mm thickness). The sites of dural laceration were examined using video footage and operative records.
Results
The pathological findings and days between the primary and revision surgeries showed no statistical difference (p=0.14). Analysis of multiple factors, revealed no significant difference between the primary and revision surgery groups with regard to hospital days (p=0.23), blood loss (p=0.99), and operative time (p=0.67). Dural lacerations obviously increased in the revision surgery group (1.3% vs. 16.7%, p<0.01) and were mainly located near the herniated disc in the primary surgery group and near the root shoulder in the revision surgery group, where severe fibrosis and adhesion were confirmed. To avoid dural laceration during revision surgery, meticulous decompressive manipulation must be performed around the root sleeve.
Conclusions
We recommend that meticulous epidural dissection around the scar formation must be performed during revision surgery to avoid complications.
Introduction
Conservative management is the currently the main treatment approach for lumbar disc herniation. However, certain patients do not achieve symptom relief with such conservative therapies, and surgical procedures are subsequently required. For such cases, posterior lumbar discectomy is the most common surgical procedure and has been performed for >50 years. With the recent emergence of many new technologies, the outcomes of posterior lumbar discectomy have improved and the use of the procedure has increased [1234]. Nevertheless, certain problems associated with this procedure remain to be addressed. One unresolved problem is recurrent leg pain, which presents either at an early stage after the initial surgery or relatively late. Thus, pathological findings associated with the time of recurrence should be investigated. The other unresolved problem is the rate of dural laceration. Several studies have indicated that the rate of dural laceration is higher during revision surgery than during initial discectomy [45678]. Hence, we investigated the location of dural laceration during the initial and revision surgeries to clarify the causes of dural laceration. Here, we retrospectively investigated patients undergoing revision surgery after microsurgical lumbar discectomy (MSD) to analyze recurrent herniation pathologies and complications to determine the manner in which lumbar disc herniation can be more efficiently managed.
Materials and Methods
At Department of Spinal Disorders Center, all operations were performed according to a standard procedure. The level to be explored was confirmed using radiographs during surgery. Lumbar discectomy was performed using via a posterior approach with unilateral partial hemilaminectomy. In most cases, we performed medial foraminotomy to decompress the affected root. After removing the prolapsed disc components, the annulus fibrosus was incised to remove the nucleus pulposus as much as possible. These procedures were performed using a surgical microscope. In the present series, 63.1% of the initial 382 lumbar discectomies were performed by one senior surgeon (JH) who had >30 years of experience with MSD, whereas approximately 20% were perforated by other spinal surgeons (TT, 14.7%; MM, 7.6%) with approximately 10 years of experience with MSD.
Between April 2003 and December 2012, 476 patients with lumbar disc herniation underwent MSDat Fujieda Heisei Memorial Hospital. At Department of Spinal Disorders Center, the surgical indications included a failed conservative therapy that last for >3 months, repeated pain attacks (remission and exacerbation lasting several weeks or months), severe leg pain, and remarkable motor weakness. Exclusion criteria were multiple level disc herniations, previous lumbar operations, and far-lateral disc herniation, in which a fixation procedure was adopted during the primary surgery. We diagnosed recurrent herniation on the basis of the presence of recurrent symptoms and the results of magnetic resonance imaging (MRI). Of 476 eligible patients, 382 were enrolled in this study.
Of 382 patients, 29 underwent surgery after posterior lumbar discectomy. We analyzed the following three issues in the revision surgery group: (1) pathological findings during the revision surgery, (2) rate and site of dural laceration, and (3) surgical outcomes and revision surgery rate. We retrospectively assessed multiple factors, such as sex, age, and complications. In the revision surgery group, we evaluated the site of revision interval between the first and second surgeries, site of intraoperative dural laceration, pathological findings of the revision surgery, and incidence of dural laceration. Among 168 patients in the primary surgery group and 11 in the revision surgery group, we evaluated hospital day, blood loss, and operative time (Table 1). Before the revision surgery, pain killers and root block were used for controlling neuropathic pain for several months (mean, 1.8 months). The affected disc levels were mainly L4/5 and L5/S1 (193 and 149 patients, respectively) in the primary surgery group, and L3/4, L4/5, and L5/S1 (four, 17, and eight patients, respectively) in the revision surgery group.
Results
Among 29 patients enrolled, 22 underwent revision surgery at the same level and site (recurrent cases in the narrow sense, 6.3%), three underwent revision surgery at the same level but at a different site, and three at a different level (Fig. 1). Regarding the treatment, the same MSD procedure was adopted; here the previously placed partial hemilaminectomy was meticulously enlarged. In the revision surgery group, two patients required pedicle screw fixation because of enlarged facetectomies, whereas one patient required fixation because of adjacent-level postoperative instability. One patient with supramuscular infection underwent wound lavage.
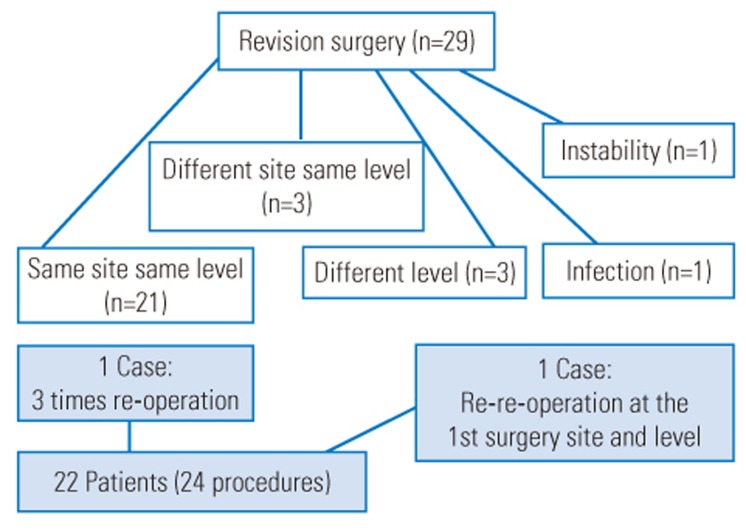
Details of revision surgery. A total of 22 patients (24 procedures) underwent revision surgery for true recurrent herniation.
The average duration from the primary surgery to the revision surgery was 436 days (range, 21–2,322 days) in patients who underwent revision surgery at the same level and 1,223 days (range, 762–1,971 days) in those who underwent revision surgery at a different level. Among 22 patients (24 procedures) who underwent revision surgery at the same site and level, 11 procedures were performed within 180 days and 13 were performed 180 days after the primary surgery. Of the 24 procedures, the pathological changes associated with compression factors were classified into two types depending on intraoperative findings: (1) true recurrence (16 cases) and (2) minor recurrence with peridural fibrosis (>4 mm thickness; eight cases). Among the 16 procedures with type 1 and eight with type 2 changes, we performed seven and two, respectively, within 180 days after the primary surgery (Fig. 2). χ2 test revealed no significant difference in the type of changes or revision surgery timing (p=0.14).
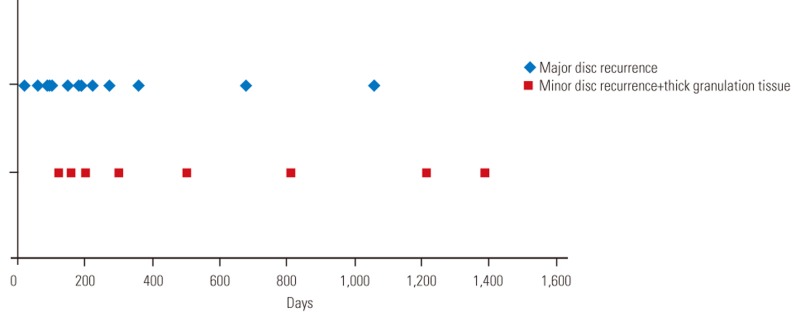
The association of timing from primary surgery to the revision surgery with pathologies of the revision surgery.
Regarding the surgical complications, dural lacerations occurred in five of 382 patients (1.3%) and in 4 of the 24 patients (16.7%) in the primary and revision surgery groups, respectively. This difference was significant (χ2 test, p<0.01). The dural lacerations occurred near the root canal region at the intervertebral disc in the primary surgery group and near the root shoulder region where severe granulation was formed and remarkable adhesive change occurred in the revision surgery group (Fig. 3). Injury because of the drilling procedure occurred in two and one patient, respectively. Other dural lacerations were caused by the forceps during the detaching procedure. These dural lacerations were repaired using dural suture and fibrin glue sealant, resulting in neither continuous liquorrhea nor meningocele formation. No nerve root injuries, epidural hematoma formation, or pulmonary embolism occurred in both the groups. One patient had a local infection in the subcutaneous suprafascial area.
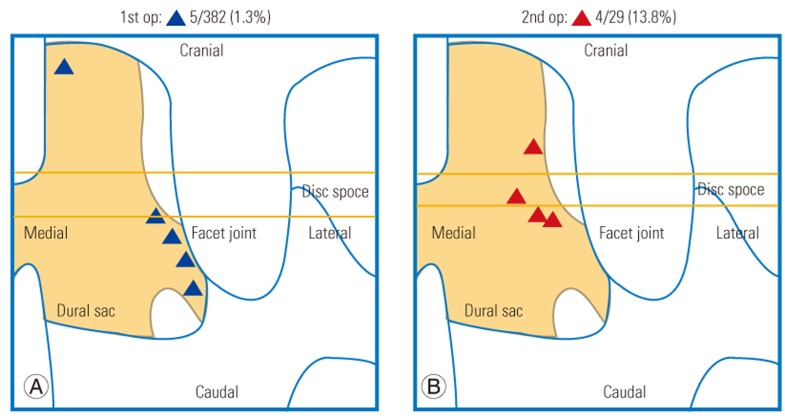
Locations of dural lacerations. Laceration occurred near the root canal region at the intervertebral disc (A) and mainly near the root shoulder, where scars usually formed (B), in the primary and revision surgery groups, respectively. OP, operation.
We were able to evaluate hospital days, blood loss, and operative time in 168 and 11 patients in the primary and revision surgery groups. Student t-test was used to evaluate these multiple factors, and the results are reported in Table 1. There were no significant differences between the primary and revision surgery groups in terms of the mean length of hospital stay (16.8 days [range, 5–61 days] versus 21.6 years [range, 9–50 years]; p=0.23), mean blood loss (24.5 [range, 5–130] versus 24.5 [range, 10–50]; p=0.99), or mean operative time (121.5 [range, 47–313] versus 130.3 [range, 85–311]; p=0.67).
Discussion
Using a surgical microscope, the operative field can be clearly visualized as a bright, three-dimensional surgical field. The entire operative process can be recorded, which is very useful for training purposes. A surgeon who plans to perform a different operative procedure should know the anatomy well. In our study, we analyzed the following three issues in the revision surgery group: (1) pathological findings during the revision surgery, (2) rate and site of dural lacerations, and (3) surgical outcomes and revision surgery rate.
1. Pathological findings at the revision surgery site
Ebeling et al. [9] examined 92 patients who underwent revision surgery after primary lumbar discectomy and reported that disc herniation recurred at the same level and site in 43% of patients, whereas it recurred at a different level in 15% of patients. A combination of small disc herniation and epidural granulation formation was observed in 23% of patients, whereas epidural granulation tissue had an important role in the development of symptomatic radicular pain in only 5% of patients [9]. Furthermore, Nakajima et al. [10] reported that 92 patients underwent revision surgery because of recurrent herniation (57%), stenosis owing to granulation (13%), osseous stenosis (16%), postoperative spinal instability (11%), and adhesive arachnoiditis (3%). In addition, Hanakita and Suwa [11] reported regarding 15 patients who underwent revision surgery at the same level and site and noted recurrent herniation in 33%, compression by epidural granulation tissue in only 13%, and a combination of small recurrent herniation and epidural granulation in 47%. Several studies have reported regarding the significance and role of postoperative epidural granulation. According to Sen et al. [12], epidural scar tissue is formed at 6 weeks to 6 months postoperatively. After 12 months, further scar formation is not observed. Ross et al. [13] reported that patients with a marked amount of epidural scar formation tend to experience a 3.2-fold greater radicular pain compared with those with less extensive scar formation. In contrast, Annertz et al. [14] reported no difference in the presence and extent of epidural fibrosis between symptomatic and asymptomatic patients. In summary, the actual significance and role of epidural postoperative scar formation remain controversial.
We analyzed the intraoperative status of the affected root, and investigated the association between revision surgery time and associated pathological findings (Fig. 2). As mentioned, epidural granulation was observed after several months. Therefore, we suggest that pathological findings and reoperation timing have some association, but there was no statistical difference.
2. Rate and site of dural laceration in the revision surgery group
The occurrence of dural lacerations with or without root injury is one of the most frequent complications of lumbar discectomy. The frequency of dural lacerations during lumbar discectomy has been reported to be 1.1%–3.7% among patients who undergo initial discectomy and 8.1%–21% among those who undergo revision surgery [45678]. The sites of dural laceration were examined using intraoperative video footage and operative records. As mentioned in the Results section, dural lacerations in the revision surgery group mainly occurred at the nerve root shoulder, where marked epidural scar formation and adhesion were observed. We assessed and drew the location of dural lacerations using the operative records and surgical video footage (Fig. 3). A meticulous detachment procedure must be performed at this site to avoid dural lacerations. Furthermore, at our department, foraminotomy is performed first by following the nerve root sleeve proximally to identify the intact nerve root sleeve. Takahashi et al. [15] assessed the locations of dural laceration and noted that in patients with lumbar disc herniation, tears mainly occurred near the herniated disc, similar to that observed in our study. In the revision surgery group, dural lacerations were observed adjacent to the root-shoulder region, where severe granulation formation and marked adhesive changes occurred [1617].
3. Surgical outcomes and reoperations rate of lumbar discectomy.
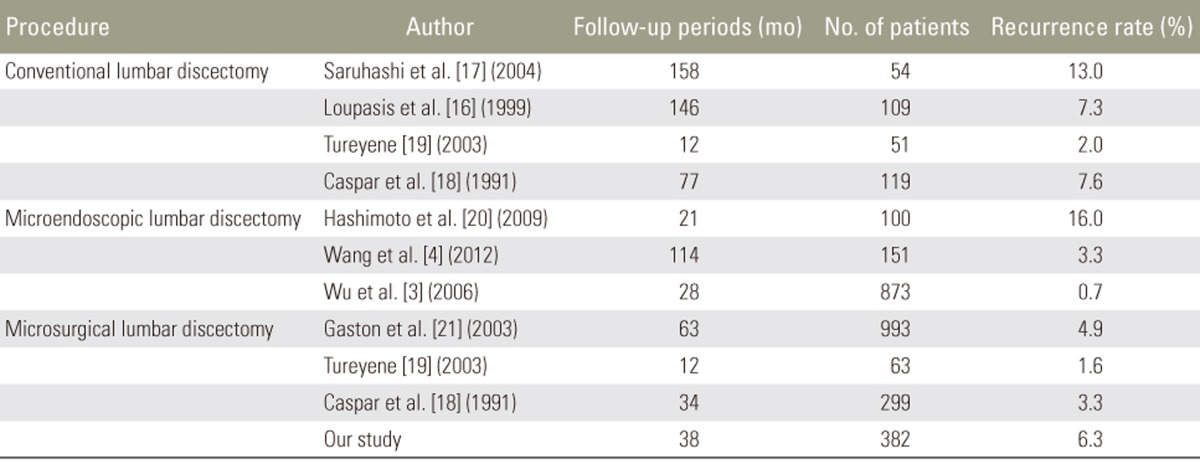
Several studies have reported the results and reoperation rates of lumbar discectomy [3491618]. Caspar et al. [18] compared MSD and conventional lumbar discectomy (CD) in 418 patients. According to their study, the complication rate was lower and the length of hospitalization was shorter in the MSD group than in the CD group; thus, patients returned to work faster in the MSD group than in the CD group. The reoperation rates in the MSD and CD groups were 3.4% and 7.6%, respectively [18]. In a randomized controlled study, Tureyen [19] compared 114 patients and reported that surgical outcomes were equal in the MSD and CD groups, and there was no significant difference regarding hospitalization length in both the groups. However, the MSD procedure allowed patients to return to their work and normal lives earlier, without excessive reliance on postoperative narcotic analgesics. Righesso et al. [1] compared CD and microendoscopic discectomy (MED) in 40 patients. Although the outcomes were the same in both the groups, the size of the skin incision, hospitalization length, and operative time were significantly less in the MED group. Several findings have been reported regarding the recurrence rate of MED. Hashimoto et al. [20] and Wu et al. [3] reported recurrence rates of 16% and 0.7%, respectively. Table 2 shows previously reported recurrence rates and follow-up periods for several surgical procedures [34916171819202122].
The operative time and length of hospital stay were longer, but blood loss was lesser in our study than in other studies [2324]. In our study, primary and revision surgeries were thoroughly performed; therefore, no significant differences were noted between the two groups. It appears that patients have a longer hospital stay in Japan compared with other countries. Although the length of hospital stay for such patients is usually shorter at present, the length of hospital stay for such patients approximately 10 years ago would extend to a month, as mentioned in a previous study [22].
The inherent limitation of this study was its retrospective design. Therefore, we could not assess all patients who underwent a primary surgery. Moreover, some patients may have undergone revision surgery at another hospital, and hence, the recurrence rate may be slightly higher. Gadolinium-enhanced MRI should be used to evaluate epidural scar formation. By evaluating MRI and the intraoperative status of patients, the accuracy of imaging findings can be determined.
Conclusions
In our study, of the 382 patients, 29 underwent revision surgery. We evaluated the following three problems; (1) revision surgery pathology, (2) rate and site of dural laceration after revision surgery, and (3) surgical outcomes and revision surgery rate. The pathological findings and revision surgery timing demonstrated no statistical difference (p=0.14). In the revision surgery group, dural lacerations mainly occurred at the nerve root shoulder. We recommend that meticulous epidural dissection around scar formation must be performed during revision surgery to avoid such a troublesome complication.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.