Minimally Invasive Lumbar Spinal Decompression in Elderly Patients with Magnetic Resonance Imaging Morphological Analysis
Article information
Abstract
Study Design
Case-control study.
Purpose
In this study, we aimed to investigate clinical outcomes and morphological features in elderly patients with lumbar spinal stenosis (LSS) who were treated by minimally invasive surgery (MIS) unilateral laminectomy for bilateral decompression (ULBD) using a tubular retractor.
Overview of Literature
Numerous methods using imaging have been attempted to describe the severity of spinal stenosis. But the relationship between clinical symptoms and radiological features remains debatable.
Objective
In this study, we aimed to investigate clinical outcomes and morphological features in elderly patients with LSS who were treated by MIS-ULBD.
Methods
We methodically assessed 85 consecutive patients aged >65 years who were treated for LSS. The patients were retrospectively analyzed in two age groups: 66–75 years (group 1) and >75 years (group 2). Clinical outcomes were assessed using the Visual Analog Scale (VAS), Oswestry Disability Index (ODI), and the modified MacNab criteria. Outcome parameters were compared between the groups at the 1-year follow-up. Core radiologic parameters for central and lateral stenosis were analyzed and clinical findings of the groups were compared.
Results
At the 1-year follow-up, patients in both groups 1 and 2 demonstrated significant improvement in their VAS and ODI scores. All clinical outcomes, except postoperative ODI, were not significantly difference between the groups. In addition, no significant difference was noted in the preoperative radiological parameters between the groups. There was no statistically significant correlation between radiological parameters and clinical symptoms or their outcomes. Moreover, no differences were noted in perioperative adverse events and in the need for repeat surgery at follow-ups between the groups.
Conclusions
MIS-ULBD by tubular approach is a safe and effective treatment option for elderly patients with LSS. Clinical outcomes in patients with LSS and aged >75 years were comparable with those in patients with LSS and aged 66–75 years. Moreover, we did not find any correlation between radiological parameters and clinical outcomes in either of the two patient groups.
Introduction
In an aging society, an increase in the occurrence of lumbar degenerative diseases, including lumbar spinal stenosis (LSS), is unavoidable [1]. LSS is one of the most common cause of lumbar spine surgery in patients aged >65 years. LSS decreases the quality of life and in severe cases, presents with problems in activities of daily living among elderly patients with radiculopathy and neurogenic intermittent claudication. In addition, the use of drug-based and non-operative treatments may fail to result in improvement and satisfaction in some patients. Decompression surgery, with or without fusion or devices, is more effective than continued conservative treatment, when the latter is not successful in patients with symptomatic LSS [2]. A recent randomized controlled trial demonstrated that a combination of decompression and fusion surgery does not result in better clinical outcomes at 2- and 5-year follow-up than decompression surgery alone [3].
Deyo et al. [4] reported that age is positively correlated with complication rates in patients treated by standard open laminectomy. However, minimally invasive surgery (MIS), which decreases the physiological burden of a surgery, can particularly benefit the elderly population by reducing the surgical risk associated with preoperative morbidity and postoperative immobility [5]. MIS techniques such as unilateral laminectomy for bilateral decompression (ULBD) for LSS have shown better clinical outcomes and have been widely used in comparison to conventional open laminectomy [56].
Although magnetic resonance imaging (MRI) is broadly used in establishing the diagnosis of LSS, the relationship between clinical symptoms and radiological features remains debatable [7]. Numerous methods using imaging have been attempted to describe the severity of spinal stenosis [89]. However, to the best of our knowledge, there is no published literature thus far that deals with the discussed characteristics in the elderly using recent core parameters chosen in the consensus conference [10].
The purpose of this study was to report clinical results of MIS-ULBD in a single institution to contribute to the evidence base of the effectiveness of ULBD in elderly patients with LSS. We have also described morphological characteristics according to age and the relationship between magnetic resonance (MR) parameters and symptom or outcomes.
Materials and Methods
1. Patient selection
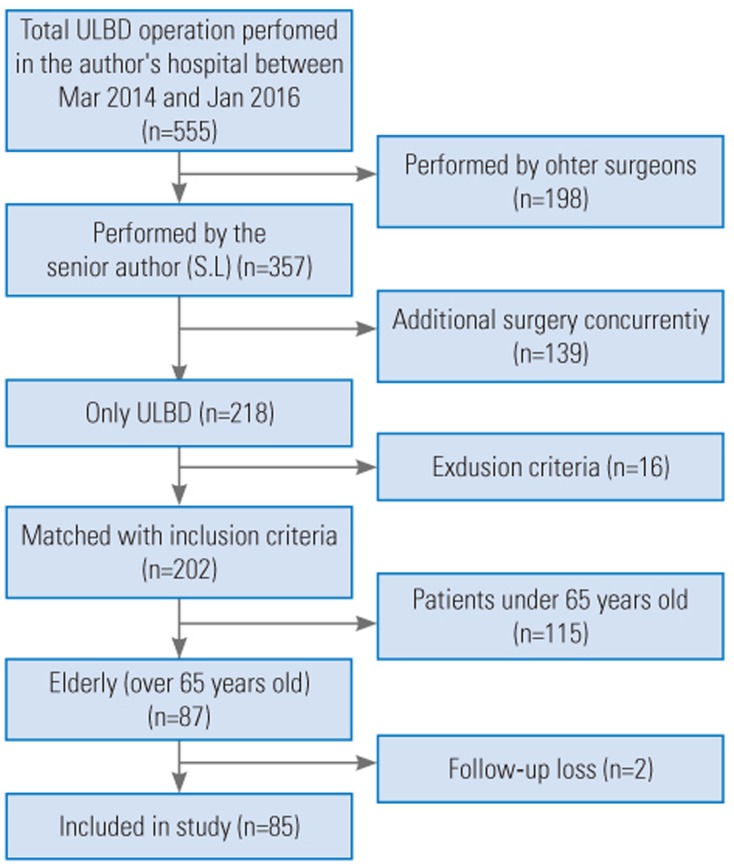
A total of 555 subjects were treated with ULBD at Barunsesang Hospital from April 2014 to January 2016. To avoid surgeon bias, we included 357 patients who were operated by the senior author (SL) for analysis in this study. We excluded 139 patients who concurrently underwent additional surgeries, such as discectomy, foraminal decompression, screw removal, or fusion. We also excluded 115 patients aged <65 years. Finally, 85 patients who successfully completed the 1-year follow-up were included in the study. Patients were divided based on their age (group 1: <65 years, n=52 and group 2: >65 years, n=33). Informed consent was provided by all patients or their family members under an approved Institutional Review Board protocol.
Our sample included patients who were unresponsive to non-operative conservative treatment for at least 12 weeks and who showed progressive symptoms despite continued non-operative treatment. The exclusion criteria included patients with marked neuroforaminal stenosis (treated by fusion or foraminal decompression at our institution, described elsewhere) [11], over three levels of stenosis (treated by spinous process splitting laminectomy at our institution, described elsewhere) [12], any prior spine surgery at any operative level in consideration of morphological changes, any prior lumbar fusion at any level to avoid adjacent disc disease, or requiring additional concurrent treatments. Patients with segmental instability, lytic spondylolisthesis, and degenerative spondylolisthesis over grade 2, with predominant lower-back pain were also excluded from the study. Only selected patients with lumbar spinal central or lateral stenosis treated by ULBD were included in the present study (Fig. 1).
2. Clinical assessment
Demographic, preoperative, and postoperative data were collected from patients' medical records. Preoperative and postoperative patient-reported outcome parameters included Visual Analog Scale (VAS) scores, Oswestry Disability Index (ODI), and MacNab grade. VAS scores for leg pain and ODI scores were collected preoperatively and on the day of the 1-year follow-up. The MacNab grade for functional improvement was noted for all patients at the time of their 1-year follow-up. Global outcomes and patient satisfaction were assessed by using modified MacNab criteria (excellent, good, fair, and poor).
3. Imaging analysis
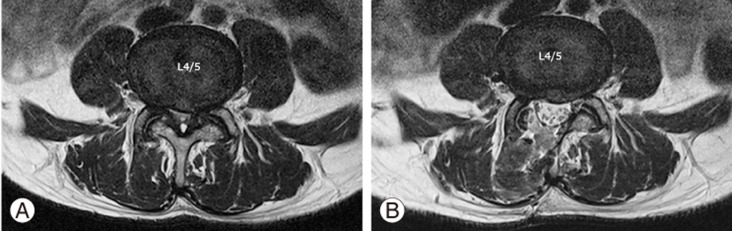
Two observers independently measured the diagnostic parameters. For each parameter, we used the average of the two observers' measurements. A difference in grading was observed in two cases and was solved in consensus. Preoperative and postoperative imaging studies (anterior-posterior and lateral flexion-extension radiographs, sagittal and axial computed tomography, and sagittal and axial T1W and T2W MRI) were methodically assessed for the degree of spondylolisthesis and presence or absence of segmental instability and scoliosis based on the exclusion criteria. The dural sac anteroposterior diameter, dural sac cross-sectional area (DSCSA), lateral recess height, compromise of the central zone [13], and nerve root compression in the lateral recess [14] were included in the analysis according to the consensus conference on core radiological parameters to describe lumbar stenosis [10] (Fig. 2). The most constricted level was selected for analysis in patients affected at a double level. These parameters were measured using a measuring program with a builtin picture archiving communication system (PiView; INFINITT Co. Ltd., Seoul, Korea).
4. Surgical techniques
In the present study, the surgery was performed under epidural anesthesia in 95% cases (81/85). Four patients underwent surgery under general or spinal anesthesia based on the decision of the anesthesiologist. During surgery, the patients were placed in a prone position on a Wilson frame. After identification of the operation level under fluoroscopic guidance, the incision site was marked on the inferior part of the lamina immediately above the index disc level, which was approximately 1 cm away from the midline. Surgery was performed in a mini-open fashion with 16-mm working tubes (MetRx; Medtronic Sofamor Danek, Memphis, TN, USA) using a skin incision of approximately 1.8 cm. After introducing a tubular retractor over the index lamina perpendicular, laminectomy was performed using a high-speed diamond drill and Kerrison rongeurs for decompression of the ipsilateral exiting roots. Decompression was usually performed clockwise and was followed by continued decompression of the ipsilateral lateral recess for identifying the traversing root. Then, the roof of the spinal canal was undercut. Hence, contralateral traversing nerve roots were also visualized and decompressed after drilling of the contralateral lateral recess. Subsequently, the contralateral exiting roots were identified and decompressed. After massive irrigation, an antiadhesive agent was applied over the thecal sac. Finally, the surgical wound was closed layer by layer (Fig. 3, Video 1).
5. Statistical analysis
For statistical analysis, the paired sample t-test, independent sample t-test for group comparisons, Fisher's exact test for categorical comparison, and Pearson's correlation coefficient for assessing the relationship between radiological parameters and clinical outcomes were conducted using IBM SPSS ver. 21.0 (IBM Corp., Armonk, NY, USA). All p<0.05 were considered to be statistically significant.
Results
A total of 85 patients were included in the study whose characteristics are described in Table 1. Mean ages at the time of surgery were 73.80, 70.40, and 79.15 years for group 1+group 2, group 1, and group 2, respectively. The most common level of spinal stenosis was the L4–L5 segment. Although sex distribution and body mass index (BMI) were significantly different between the groups, preoperative risk factors were similar.

Clinical outcomes of minimally invasive unilateral laminectomy for bilateral decompression by tubular retractor
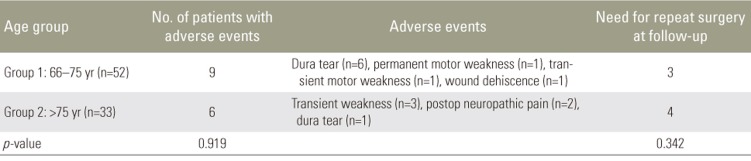
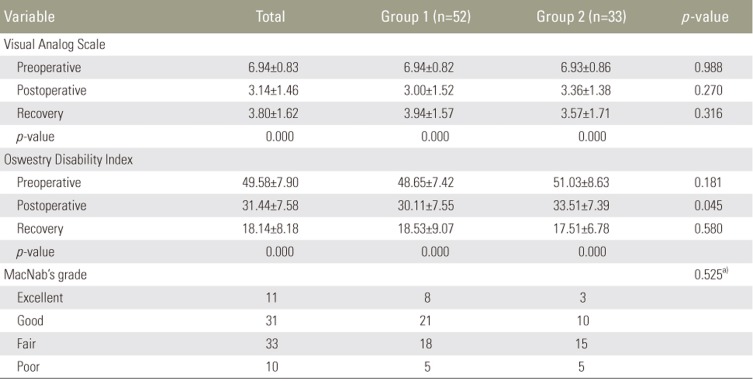
VAS and ODI scores showed significant improvement at the 1-year postoperative follow-up in both groups (p<0.05 and p<0.05, respectively); no significant differences were noted in VAS and ODI scores between the groups, except the postoperative ODI which was greater in group 1 than in group 2. The MacNab's grade was not significantly different between the two groups (p=0.525) (Table 2).
Clinical outcomes of minimally invasive unilateral laminectomy for bilateral decompression by tubular retractor
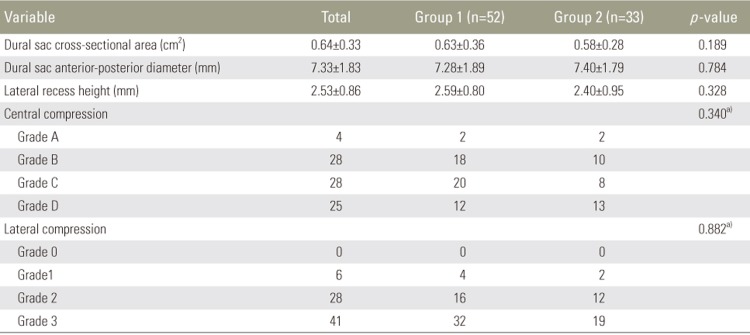
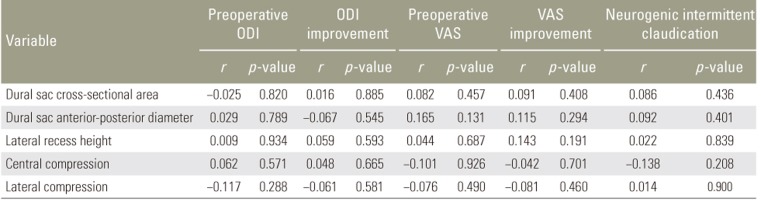
The radiological parameters are presented in Table 3. The preoperative parameters were not significantly different on group comparisons. In addition, the degree of both central and lateral stenosis did not show any difference with respect to the age group. Moreover, radiological parameters were not correlated to symptoms (Table 4).
The preoperative results, including the surgical time, hospital stay duration, blood loss, and hospital charges were not significantly different between the groups (Table 5). In addition, no differences were noted in the preoperative adverse events between the groups. Finally, no major complications, deaths, or infections occurred in the study (Table 6).

Perioperative results of minimally invasive unilateral laminectomy for bilateral decompression by tubular retractor
Discussion
Shamji et al. [15] retrospectively reviewed the efficiency and safety of LSS in elderly and recommended that surgical intervention should be considered even in elderly patients. Other studies reported favorable clinical outcomes in octogenarians [16] and multilevel-affected patients [17], although patients with diabetes mellitus [18] or high BMI (>30 kg/m2) [17] were reported to show negative prognostic factors after surgical intervention. In our study, patients aged >75 years presented with clinical outcomes that were comparable with that of younger patients with similar risk factors of the underlying disease, as measured by the modified frailty index. In general, the operating surgeon should be considerate of the life expectancy at a given age, but advanced age per se is not a contraindication for decompressive surgery.
Although the usage of the MIS technique for spinal stenosis has increased, it is relatively scarcely used in elderly patients [5]. Rosen et al. [19] prospectively investigated 57 patients aged >75 years and reported improvements in VAS and ODI scores without any major complications. Aleem and Rampersaud [20] found similar outcomes on comparing these scores between elderly patients (age >70 years) and younger patients (age <70 years). Various procedures, including foraminotomy, performed by Rosen et al. [19] and Aleem and Rampersaud [20], resulted in decompression-only or in decompression and fusion. We performed minimally invasive decompression-only in elderly patients with focal (1–2 level) LSS using a tubular retractor microscopy-assisted surgery for ULBD.
Among the various MIS techniques known for LSS, such as percutaneous biportal endoscopic decompression, or full endoscopic procedures, we selected MIS-ULBD using a tubular retractor (first described by Spetzger et al. [21]) and through the tubular approach suggested by Parmer [22]. ULBD for LSS showed better outcomes than conventional laminectomy [2324]. Cavusoglu et al. [25] also reported favorable mid-term outcomes after ULBD for LSS in their 5-year prospective study. Although asymmetric decompression may be worrisome according to the unilateral approach, Alimi et al. [26] affirms that ipsilateral and contralateral symptoms can be effectively treated by this method.
We performed volumetric access to discover the relationship between MR parameters and the severity of symptoms and their outcomes. In few previous studies, several MRI parameters were measured for evaluating the severity of spinal stenosis. However, the relationship between MRI findings and symptoms remained unclear [8]. Recently, Burgstaller et al. [7] conducted a systematic literature review and analyzed the relationship between MRI parameters and pain in 150 patients with LSS and found no correlation. In addition, no significant correlations were noted between preoperative DSCSA and clinical symptoms in patients treated by ULBD [27]. Similar results were also demonstrated in the present study.
We hypothesized that at least central stenosis would be severe in the older groups because it is a degenerative change. However, in our study, central or lateral stenosis was not frequent or severe in any specific age group. In addition, no statistically significant correlation existed with respect to any parameters for clinical symptoms or outcomes. In the literature, patients with degenerative LSS rarely manifested cauda equina syndrome. In the present study, no patient complained of saddle anesthesia, bladder and bowel dysfunction, or definite motor weakness, despite manifesting severe stenosis on MRI. Thus, we believe that the use of MR parameters is inadequate for evaluating the severity of spinal stenosis.
Various factors associated with the limitations of MR or the characteristics of LSS per se could have influenced these results. First, cross-sectional imaging is insufficient for evaluating spinal stenosis. Bartynski and Lin [14] reported inferiority of MRI compared with CT with myelography owing to the difficulty in measuring uniformly depending on the situation. Compared with high intraobserver reliability, the inter-observer reliability is low [13]. Second, most patients with spinal stenosis show some degree of accompanying disc protrusion. The sudden expansion of disc protrusion may trigger symptoms in some patients through compression delivered at a rapid onset rate [28]. In these cases, nerve entrapment may induce sudden onset of pain rather than chronic shifting and late compression. Third, congenital morphological feasibility is also a feasible reason. The trefoil configuration showed high incidence and vulnerability for LSS in some studies [14]. Fourth, the spinal canal is a dynamic structure, and the diameters vary due to changing postures and body activities. Consequently, a static image of the lumbar canal in the supine position may not represent dimensions of the spinal canal during activity [9]. Fifth, hemodynamics in the spinal region assumes a certain role in the symptoms. Some evidence supports the thesis that obstruction of the blood circulation is causal for the intermittent character of pain [29]. Finally, conventional MR cannot evaluate the nerve function that may be assessed by new imaging modalities, such as high-resolution MR neurography or diffusion tensor imaging [30].
There are some limitations of the present study. This was a retrospective, uncontrolled review of clinical outcomes in a single institution. Our study included a rather short follow-up. With respect to patient demographics, the younger group showed significantly higher BMI than the older group; this was believed to be associated with senile sarcopenia and the fact that sex distribution was significantly different.
Conclusions
MIS-ULBD by a tubular approach is a safe and effective treatment option for elderly patients with LSS. Clinical outcomes of patients aged >75 years were comparable to those of 66–75-year-old patients with LSS. We could not find any correlation between radiological parameters and clinical findings.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.
References
Supplementary Materials
Supplementary materials can be found via https://www.youtube.com/watch?v=2kpJRAe2H2U.
Video 1
Unilateral laminectomy for bilateral decompression using a tubular retractor for lumbar spinal stenosis.