Percutaneous Endoscopic Cervical Discectomy: Surgical Approaches and Postoperative Imaging Changes
Article information
Abstract
Study Design
Retrospective clinical study.
Purpose
This study investigated the relationship between surgical approaches and surgical outcomes in patients undergoing percutaneous endoscopic cervical discectomy (PECD), including the reduction in intervertebral disc height and the incidence of Modic changes.
Overview of Literature
The anterior approach involves partial invasion of the intervertebral disc, with a reported reduction in intervertebral disc height after PECD.
Methods
Forty-two patients with cervical disk hernia who underwent PECD and magnetic resonance imaging at least 3 months postoperatively were divided into four groups according to the hernia sites and the surgical approach used: unilateral hernia treated using the contralateral approach (group C, n=18), unilateral hernia treated using the ipsilateral approach (group I, n=15), midline hernia (group M, n=4), and broad and bilateral hernia (group B, n=5). Modic changes and intervertebral disc height were evaluated.
Results
The overall incidence of Modic changes was 52.4%: 72.2% in group C, 26.7% in group I, 25.0% in group M, and 80.0% in group B. The reduction in intervertebral disc height was 21.8% across all the patients: 24.5% in group C, 11.0% in group I, 22.8% in group M, and 23.9% in group B.
Conclusions
The incidence of Modic changes and the reduction in intervertebral disc height were lower in the patients treated using the ipsilateral approach than in those treated using the contralateral approach. Traditionally, a contralateral approach has been used for PECD; however, the ipsilateral approach is more appropriate and is therefore recommended.
Introduction
Anterior cervical discectomy and fusion (ACDF) is the standard treatment for cervical disk hernia [1]. However, there is a concern that cervical fusion may accelerate adjacent segment degeneration by increasing mechanical stress [2345]. Conversely, percutaneous endoscopic cervical discectomy (PECD) can preserve the intervertebral disc, thereby avoiding adverse effects on the adjacent segments. PECD uses a small outer tube and an endoscope with a percutaneous full-endoscopic system comprising a light source, an endoscope, a working channel, and an irrigation channel. However, the anterior approach involves partial invasion of the intervertebral disc, and a reduction in intervertebral disc height after PECD has been reported [67]. Intervertebral disc height is an index of intervertebral disc degeneration, although it is not always associated with clinical symptoms. The incidence of Modic changes, which are considered to be associated with clinical symptoms [89], is unknown [10].
Traditionally, a contralateral approach has been used in PECD because it offers better access than the ipsilateral approach [67]. However, we consider the ipsilateral approach to be more appropriate. To the best of our knowledge, no study has assessed the difference between the two surgical approaches in the invasion of the intervertebral disc. This study examined the reduction in intervertebral disc height and the incidence of Modic changes in patients undergoing PECD and investigated whether these indices differed between the ipsilateral and contralateral approaches.
Materials and Methods
1. General information
The study included patients who underwent PECD between August 2011 and December 2015 followed by magnetic resonance imaging (MRI) examination at least three months after the surgery. All patients had been diagnosed with cervical disk hernia on MRI and had not responded to conservative treatment. Patients with giant hernia and marked myelopathy were excluded. Overall, 42 patients (33 men and 9 women) with a mean age of 46.0 years, with surgical levels C3/4 (n=2), C4/5 (n=7), C5/6 (n=21), and C6/7 (n=12) were included.
2. Surgical method and follow-up
The surgery was performed under general anesthesia with the patient in a supine position. The head was fixed and pulled cranially with a Mayfield clamp. The upper extremities were placed along the body and pulled caudally. X-ray fluoroscopy was used to visualize the process. With the trachea or larynx pushed toward the contralateral side with the fingers, an 18G spinal needle was inserted via the skin of the frontal neck, passing between the airway and the internal carotid artery, and advanced to the intervertebral disc. After making a 5-mm skin incision, a dilator was inserted over the guide wire. An outer tube (height 4.1 mm, width 6.7 mm, square-tubular) and endoscope (VERTEBRIS cervical anterior system; Richard Wolf Co. Ltd., Knittlingen, Germany) was inserted (Fig. 1). Under endoscopic observation using the continuous irrigation method, the intervertebral disc hernia was dissected and removed using forceps and a sharp curette. If required, an electric drill was used to dissect bone spurs. When the hernia was extra ligamentous, it was removed with a hook probe and forceps following partial resection of the posterior longitudinal ligament. The patient was allowed to walk 3 hours after surgery and was discharged the next day, with the instruction to wear soft collars for one week. During follow-up, the patients were scheduled to visit the outpatient clinic at 1, 6, 12, and 24 months postoperatively and to undergo MRI at 6, 12, and 24 months.

The endoscopic system used for percutaneous endoscopic cervical discectomy. This comprised a small outer tube (4.1 mm×6.7 mm, square-tubular) and an endoscope with a percutaneous full-endoscopic system with a light source, an endoscope, and an irrigation channel.
The selection of surgical approach (contralateral or ipsilateral) for patients with unilateral hernia was unrelated to their individual characteristics. The contralateral approach was used for patients during the first half of the study period, whereas the ipsilateral approach was used for patients during the second half of the study period.
3. Evaluation
The subjects were retrospectively divided into four groups according to the sites of hernia and the surgical approaches used: unilateral hernia treated using the contralateral approach (group C), unilateral hernia treated using the ipsilateral approach (group I), median localized hernia resected locally (group M), and broad and bilateral hernia resected widely (group B). The main focus of the investigation was the differences between group C and group I (i.e., the contralateral and ipsilateral approaches) with regard to the intervertebral disc height, Modic changes, and neck and shoulder pain.
Imaging measurements were made by a blinded orthopedic surgeon using a DICOM viewer with the POP-net web server (Image ONE Co., Tokyo, Japan) on MRI images obtained 3–12 months after surgery. The intervertebral disc height at the center of the surgically treated intervertebral disc was measured on a midline sagittal plane image. A T2-weighted fat suppression sequence was carefully examined for Modic changes in the vertebral bodies. If a patient had Modic changes before surgery, he or she was considered in the analysis to have Modic changes if these were exacerbated after surgery but not if they showed a reduction. Pain in the neck and shoulder was reported subjectively by the patient on a scale of 0–10, using a Visual Analog Scale (VAS).
Group C and group I were compared using a 2×2 chi-square test or unpaired Student t-test. Statistical significance was set at p<0.05.
Results
There were 18 subjects in group C, 15 subjects in group I, four subjects in group M, and five subjects in group B. The mean time after surgery when the MRI was obtained was 7.6 months (range, 3–12 months). Comparisons between group C and group I showed no significant differences in the mean age of the subjects (43.7±9.5 versus 47.9±14.2, p=0.1590), the mean resected disk volume (0.55±0.23 g versus 0.51±0.24 g, p=0.3426), the male-to-female ratio (15:3 versus 11:4, p=0.4133), or the mean period between surgery and MRI (8.8±3.3 months versus 7.0±3.3 months, p=0.0629). No subject in either group experienced intraoperative complications.
The overall incidence of Modic changes was 52.4% (22/42). In the groups, the incidence of Modic changes was 72.2% (13/18) in group C, 26.7% (4/15) in group I, 25.0% (1/4) in group M, and 80.0% (4/5) in group B. The incidence was significantly lower in group I than in group C (chi-square test, p=0.0091). At the time of the last imaging follow-up, type 1 Modic changes were observed in 14 patients and type 2 changes in 8 patients. In some patients, the Modic changes changed from type 1 to 2 during the clinical course. Two patients showed Modic changes before surgery, and the Modic changes in one patient (in group I) disappeared after surgery. There was no significant difference in the incidence of Modic changes between subjects where an electric drill was used for bone resection and those where a drill was not used (50.0% (12/24) versus 55.6% (10/18); chi-square test, p=0.9644).
The mean reduction in intervertebral disc height across all the subject was 21.8%±16.3%. The mean reduction for each group was 24.5%±10.6% in group C, 11.0%±8.8% in group I, 22.8% in group M, and 23.9% in group B. The reduction was significantly lower in group I than in group C (unpaired Student t-test, p=0.0002) (Table 1).
The mean VAS score for neck and shoulder pain was somewhat higher in the subjects with Modic changes than in those without Modic changes, but this was not statistically significant (4.4±3.4 versus 3.2±2.1; unpaired Student t-test, p=0.0913). The general symptom remnant rate (calculated as current general symptom VAS/preoperative general symptom VAS×100) was 21.7%±17.9% in group C, 20.0%±15.1% in group I, 17.5% in group M, and 24.0% in group B. There was no significant difference between group C and group I (unpaired Student t-test, p=0.3886). The mean observation period was 13.8 months.
Discussion
PECD is not widely used in clinical practice. Currently, ACDF is a standard treatment for patients with cervical disk hernia. However, there is a concern that cervical fusion may accelerate adjacent segment degeneration, although there is no consensus in this regard yet [2345]. PECD can preserve the intervertebral disc, and it does not result in the acceleration of adjunct segment degeneration because it does not induce mechanical stress. However, the anterior approach involves partial invasion of the intervertebral disc, with a reported reduction in intervertebral disc height after PECD of 11.2%–23.0% [67]. To the best of our knowledge, no previous studies have investigated Modic changes after PECD without our preliminary study [10]. Although there is no consensus on their clinical significance, we consider Modic changes to be important in clinical practice, along with the reduction in intervertebral disc height, because they are associated with local pain [89]. In the present study, the incidence of Modic changes was higher than that expected. Although there was a tendency for neck and shoulder pain among patients with Modic changes, the association was not statistically significant; this is possibly because several factors can affect neck and shoulder pain.
There was no significant difference between the clinical outcomes of group C and group I, perhaps because there can be a substantial time lag between the appearance of changes in imaging studies and the onset of clinical symptoms of degenerative diseases. Nevertheless, we believe that postoperative degeneration of the intervertebral disc should be minimized.
Several factors affecting the reduction in intervertebral disc height and causing Modic changes have been discussed here. In our clinical experience, it is rare for patients to develop Modic changes after percutaneous endoscopic lumbar discectomy (PELD). This suggests that factors common to both PELD and PECD, including the force on the vertebral body when driving the dilator into the intervertebral disc, irrigation, and radiofrequency ablation, are unlikely to be the causes of Modic changes. Furthermore, we used a Mayfield clump during PECD surgery to increase the intervertebral space and reduce the influence of any direct external force. There were no differences in the incidence of Modic changes between patients for whom an electric drill was used and those where an electric drill was not used. We speculate that use of an electric drill resulted in no significant effects because it caused limited bone resection, and its heating effect was reduced by irrigation water. The reduction in intervertebral disc height and incidence of Modic changes was lower in group I than in group C or group B. This may be attributable to the less prominent invasion of the intervertebral disc, in particular, the central and nucleus pulposus region, in group I (Fig. 2). We believe that it is important to avoid injury to the central nucleus pulposus region because this region has a shock-absorbing function, and because nutrients are barely supplied to the central part of the intervertebral disc by diffusion [11] and it is susceptible to injury [1213].

The ipsilateral approach (group I) was less invasive on the central and nucleus pulposus region of the intervertebral disc than the contralateral approach (group C). b, bronchial airway; e, esophagus; p, uncinate process; C, area passed by the contralateral approach; I, area passed by the ipsilateral approach.
Cervical disc herniation is often a lateral protrusion of the disc close to the uncinate process, resulting from the effect of the posterior longitudinal ligament. The trachea, esophagus, and thyroid cartilage are located in front of the vertebral bodies and the right and left uncinate processes of the vertebral bodies in the deeper part. This anatomical structure prevents an outer tube tip from turning toward the ipsilateral direction, resulting in the contralateral approach being less difficult than the ipsilateral approach. The contralateral approach has therefore been the approach usually used for patients with unilateral hernia [67] (Fig. 3). However, the ipsilateral approach is also feasible, in our experience, no patients who underwent PECD using the ipsilateral approach developed complications such as airway obstruction or esophageal disorder. Therefore, we recommend the ipsilateral approach for patients with unilateral cervical disc hernia.
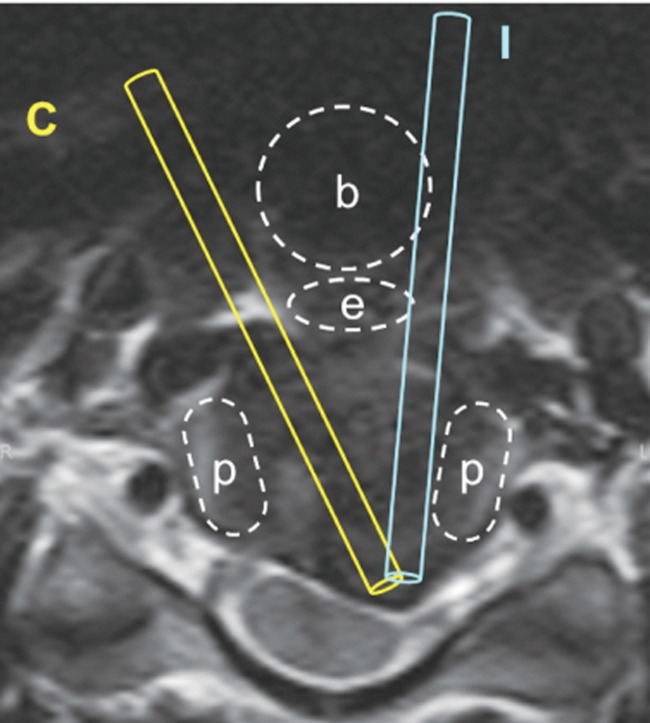
There are airways and thyroid cartilage located in front of the vertebral bodies and the right and left uncinate processes of the vertebral bodies in the deeper part. This anatomical structure prevents the outer tube tip from turning toward the ipsilateral direction, making the contralateral approach less difficult than the ipsilateral approach. Therefore, the contralateral approach is usually used for patients with unilateral hernia; however, the ipsilateral approach is also secure. b, bronchial airway; e, esophagus; p, uncinate process; C, contralateral approach; I, ipsilateral approach.
This study has some limitations. It was retrospective and the number of cases was not large. In addition, the follow-up period was not long; however, our aim was to investigate how results were related to the surgical approaches, so we believe that it was reasonable to use mid-term results (at 3–12 months) rather than long-term results, which may be greatly affected by the natural course. In MRI T2 fat suppression imaging, the influence of degeneration and edema is delicately visualized. Therefore, we used MRI obtained at least 3 months postoperatively, when there is no longer any influence on MRI of the direct external force during surgery, in order to strictly evaluate Modic changes.
Conclusions
In patients with unilateral hernia who underwent PECD, the incidence of Modic changes and the reduction in intervertebral disc height were lower for those treated using the ipsilateral approach than for those treated using the contralateral approach. Although the contralateral approach is widely used for patients with unilateral cervical disc hernias, we believe that the ipsilateral approach is sufficiently secure and more appropriate to perform.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.

