Multiple Pyogenic Spondylodiscitis with Bilateral Psoas Abscesses Accompanying Osteomyelitis of Lateral Malleolus - A Case Report -
Article information
Abstract
A psoas abscess is a potentially life-threatening infection. Multiple pyogenic spondylodiscitis with bilateral psoas abscesses accompanying an osteomyelitis of the lateral malleolus is an extremely rare event. We present our experience with needle aspiration for the treatment of osteomyelitis of the lateral malleolus and CT-guided percutaneous catheter drainage for a psoas abscess in an elderly patient. Both infections were completely resolved without recurrence. A psoas abscess should be included in the differential diagnosis of a patient with low back pain during musculoskeletal infection. Percutaneous needle aspiration or CT-guided percutaneous catheter drainage is an effective method for treating certain musculoskeletal infections.
Introduction
Psoas abscesses represent a diagnostic and therapeutic challenge because of insidious signs and symptoms, difficult differential diagnosis, and variable treatment methods. A primary abscess has no obvious source of infection, whereas secondary abscesses have clear underlying causes such as gastrointestinal tract disease, including Crohn's disease, trauma, genito-urinary tract infection, and tuberculous or pyogenic spondylitis1-5. To the best of our knowledge, there is no report of psoas abscess occurring with osteomyelitis of the lateral malleolus. Thus, a psoas abscess might have other concomitant musculoskeletal infections and can be treated with minimally invasive drainage procedures in the elderly6-10.
Case Report
A 75-year-old male was transferred from a secondary hospital, complaining of right ankle joint pain for one week, and severe lower back pain for two days developing after a slip. The patient had a twenty-year history of dull back pain, hypertension, and alcoholic liver disease. Physical examination revealed multiple tender points on the back, both inguinal areas, and the right ankle joint. The body temperature was 38℃, and he had limited range of motion in his spine and right ankle joint. Flexion contractures were noted on both hip joints. Muscle spasm was noted on the paravertebral muscles and hip flexors.
The previous diagnosis was an acute staphylococcal osteomyelitis of the lateral malleolus and an acute lumbar sprain with underlying degenerative spondylosis. He was treated with a first-generation intravenous cephalosporin after an aspiration of scanty pus from the lateral malleolus.
The white blood cell count, erythrocyte sedimentation rate, and C-reactive protein level were 17,800/ml, 57 mm/hr, and 14.1 mg/dl, respectively. Serum GOT/GPT/GGTP levels were 67/14/73 IU/L. Microscopic hematuria and proteinuria was also noted. Anteroposterior radiography showed a cortical destruction of the lateral malleolar tip and swelling of the surrounding soft tissues (Fig. 1). A Technetium-99m bone scan revealed a hot uptake on the right distal fibula (Fig. 2A), focal hot uptakes on L3 and L5, and subtle hot uptakes on T12 and L2 (Fig. 2B). A CT scan showed a suspected lesions of abscess with gas in the bilateral psoas muscles. MRI revealed a left psoas abscess at the L3 level, a right psoas abscess at the L5 level, and spondylodiscitis of L2-3 and L4-5 (Fig. 3A and B).

Anteroposterior radiograph shows cortical destruction of the lateral malleolar tip (arrow) and swelling of the surrounding soft tissue.
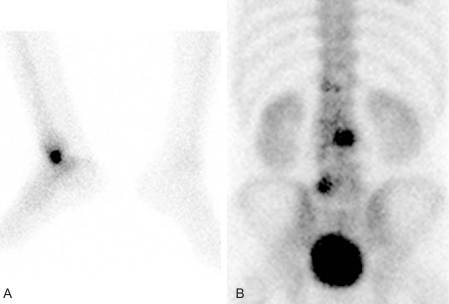
(A) Technetium-99m bone scan reveals a hot uptake on the right distal fibula, (B) focal hot uptakes on L3 & L5, and subtle hot uptakes on T12 & L2.

(A) T2-weighted coronal MRI reveals high signal intensities suggesting bilateral psoas abscesses (arrows) and destruction of L2-3 & L4-5 end plates, suggesting spondylodiscitis. (B) T2-weighted sagittal MRI shows multiple high signal intensities in vertebral bodies of T12 and the lumbar spine, however disc space narrowing and end plate destruction are noted on L2-3 & L4-5 levels only.
Due to the imbalance of electrolytes, azotemia, and hypoalbuminemia, we chose conservative methods as a first-line treatment. A second-generation cephalosporin and aminoglycoside were administered intravenously. On the 4th day of admission, the ankle swelling and redness were reduced but fever and back pain remained. We therefore performed CT-guided percutaneous catheter (12F) drainage of the left psoas muscle to drain pus and identify bacteria. The 20 cc of pus was yellowish-brown. We changed to vancomycin because of sustained intermittent fever and back pain. On the 7th day of admission, back pain and the flexion contractures of both hip joints were markedly improved, and the drained pus cultures demonstrated methicillin-sensitive Staphylococcus aureus.
Wheel chair ambulation with bracing of thoracolumbosacral orthosis was possible on the 7th day of admission, and partial weight bearing with brace and walking aids was started on the 2nd week of admission. Vancomycin was administered intravenously for 4 weeks. After 4 weeks of admission, we removed the short leg splint and recommend full weight bearing with braces. Four weeks of follow-up MRI revealed the complete resolution of abscesses. However, irregular disc space narrowing of L2-3 and L4-5 were observed (Fig. 4), and a radiograph showed no additional bony destruction of the lateral malleolus. Oral ciprofloxacin was then prescribed for 8 weeks until the C-reactive protein (CRP) normalized. The total duration of medical treatment was 3 months. We performed a physical examination, laboratory examinations, including complete blood cell count, erythrocyte sedimentation rate, CRP, and radiographic examinations during the follow-up period. At two years follow-up, there was no recurrence of symptoms and no complications, and he is performing physical activity as he was prior to the disease.
Discussion
Psoas abscesses can be classified into primary and secondary in nature2. The source of a primary psoas abscess it is unknown, but may be associated either with trauma or with a distant source of infection. The source of a secondary psoas abscess can be clearly defined by the extension of an infectious process into the psoas compartment. For example, mycobacterium tuberculosis can invade from a tuberculous spondylitis infection, as can infections of the gastrointestinal tract, including Crohn's disease, genito-urinary tract infection, and vertebral osteomyelitis1-5.
Primary psoas abscesses are more common in Asia and Africa, whereas secondary abscesses are more common in Europe2. Primary psoas abscesses are also prevalent in intravenous drug abusers and immunodeficient patients4. Primary abscesses are typically caused by Staphylococcus aureus, and secondary abscesses by enteric bacteria. In our case, the pathogen was methicillin-sensitive Staphylococcus aureus. Additionally our case included multiple musculoskeletal infections involving the long bone, axial skeleton, and deep muscles. Because the suspected pathogenesis in our case was pyogenic spondylodiscitis, our case is a secondary psoas abscess. However, it is unclear whether the bacterial origin is the infection of the lateral malleolus or septicemia starting from another unknown focus.
Modern imaging techniques, such as CT or MRI, provide better understanding of the anatomic magnitude of the infection and may suggest an underlying cause. CT can often assess the extent of the abscess, which is not always possible on ultrasound due to interference from overlying bowel gas6-8.
Traditionally, psoas abscesses have been treated with retroperitoneal surgical drainage along with appropriate antimicrobial therapy. In recent years, percutaneous drainage under image guidance has become a generally accepted method of intra-abdominal and retroperitoneal abscesses, including psoas abscess5,7-10. The success rate of percutaneous drainage was 99.5% to 76.5%8,9, with variable outcomes reported. Catheter dislocations and obstructions lead to the majority of complications8, but overall low mortality and morbidity rates are major advantages of CT-guided percutaneous catheter drainage10. CT-guided percutaneous catheter drainage is a safe and effective treatment in psoas abscess8. We followed the same principles for the treatment of our patient, with an excellent outcome.
In conclusion, psoas abscess may be an important differential diagnosis in patients with low back pain after a musculoskeletal infection, and MRI or CT scans can confirm the diagnosis and define the extent of a psoas abscess. Treatment of psoas abscess with percutaneous catheter drainage and appropriate antibiotic therapy can effectively treat selected cases, such as patients without extensive bone lesions or neurological deficits.
