Comparison of Apical Axial Derotation between Adolescent Idiopathic and Neuromuscular Scoliosis with Pedicle Screw Instrumentation
Article information
Abstract
Study Design
A retrospective study.
Purpose
To compare outcomes of apical derotation with pedicle screws in idiopathic and neuromuscular scoliosis (NMS).
Overview of Literature
No information about apical derotation in NMS with pedicle screws is available.
Methods
We performed deformity correcting surgery using pedicle screw constructs on 12 adolescent idiopathic scoliosis (AIS) patients (mean age 14.1 years) and 16 NMS patients (mean age 16.5 years). Preoperative, postoperative, and final follow-up radiographs were analyzed for Cobb's angle and pelvic obliquity, while apical rotation was measured on CT scans using the Aaro-Dahlborn method.
Results
For AIS, the mean preoperative Cobb's angle, pelvic obliquity, and apical rotation values were 57.3°, 2.8°, and 20.4°, respectively, and postoperatively they were 16.8°, 1.1° and 14.7°, respectively, showing significant correction. For NMS, the mean preoperative Cobb's angle, pelvic obliquity, and apical rotation values were 75.6°, 13.7°, and 42.9°, respectively, and postoperatively they were 27.1°, 5.8°, and 34.1°, respectively, also showing significant correction. There were no significant differences between AIS and NMS patients Cobb's angle p=0.306, pelvic obliquity p=0.887 and apical derotation p=0.113°. There were no differences in curve severity in the three groups (AIS, NMS >80°and NMS <80°); or the correction of apical rotation (p=0.25), although less correction was achieved in the Cobb's angle in the >80 NMS group (p=0.04).
Conclusions
Apical axial derotation can be achieved with posterior only pedicle screw fixation in NMS without anterior release, with comparable results in idiopathic scoliosis.
Introduction
Scoliosis is a three dimensional deformity1 with coronal angulations and axial rotation that need to be corrected simultaneously. Harrington rods produce poor control over rotational deformity2,3, and other instrumentation can better correct rotational deformity with coronal angulations. In scoliosis, the most profound rotation is observed in apical vertebrae4, although other vertebrae are also rotated, with treatment generally improving all vertebrae. Pedicle screws can best correct both deformities simultaneously and were chosen for this study.
Idiopathic scoliosis can be treated with different types of instrumentation for correcting vertebral rotation and the correction of Cobb's angle. In contrast, neuromuscular scoliosis (NMS), a rigid deformity, is not generally treated surgically to correct axial rotation. Here, we compared postoperative apical axial derotation in adolescent idiopathic and NMS treated with posterior pedicle screw fixation using CT scans.
Materials and Methods
Twelve patients with adolescent idiopathic scoliosis (AIS) and 16 patients with NMS were chosen for our study. All patients received surgery at our hospital in 2005 or 2006 with posterior only pedicle screw fixation followed by correction and fusion.
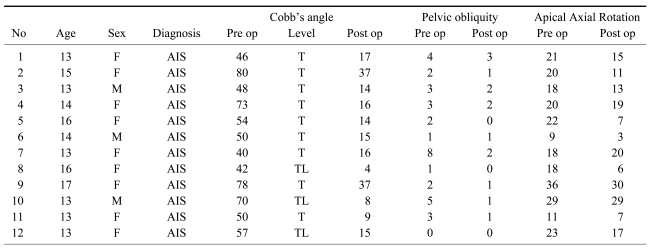
For AIS group (group A), the mean patient age (9 females and 3 males) at the time of operation was 14.1 years (Table 1). Nine patients had a major thoracic curve while 3 had major thoracolumbar curves. We excluded the patients who had double curves to maintain uniformity of the study. The average preoperative Cobb's angle was 57.3°, with flexibility of 38%.
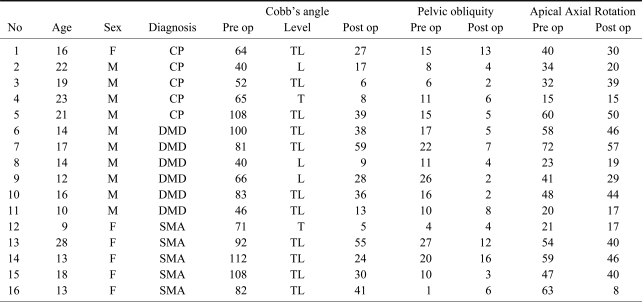
For the NMS group, the mean age of all the patients (5 cerebral palsy [CP], 6 Duchenne muscular dystrophy [DMD] and 5 spinal muscular atrophy [SMA]) was 16.5 years. Only patients with a single curve were considered for this study to reduce errors, because derotation of double curves improves one rotation angle and worsens the other. Out of 16 patients included in this group, there were 11 thoracolumbar curves, 3 lumbar curves, and 2 thoracic curves. We have divided neuromuscular patients into two groups according to curve severity; group B (curve <80°, 8 patients) with average Cobb angle of 55.5 (and group C (curve >80°, 8 patients) with an average Cobb angle of 95.7°(Table 2). Results were analyzed by idiopathic and NMS, as well as curve severity. Preoperatively, all the patients received a radiogram, CT scan, and pulmonary function test per our standard protocol.
All patients received surgery from a single spine surgeon with posterior only pedicle screw fixation, followed by correction and fusion with or without rib hump excision depending upon post-fixation appearance. During the operation, after full exposure using the standard posterior approach, pedicle screws were inserted bilaterally with freehand technique at all the levels and facet joints were thoroughly destroyed, including the apical and the adjacent levels to facilitate maximum rotational correction. Pre-contoured rods were then inserted over the pedicle screws bilaterally, followed by a standard derotation maneuver5,6 with or without in situ contouring of rods on both sides simultaneously. The rods were fixed by tightening the screw caps. Decortications of posterior laminae and posterior fusion were accomplished with bone grafts mixed with allografts. Multiple-layer wound closure was then performed and two drainage tubes inserted. All the patients underwent radiograms and CT scans, which were stored in our computerized PACS system with preoperative data, once they were hemodynamically stable and their drains were removed.
We calculated the coronal angulations by Cobb's angle7 and pelvic obliquity along a horizontal line on radiograms, while apical vertebral rotation was calculated on a CT scan with the Aaro-Dahlborn method4,8 from the mid-sagittal plane (Fig. 1). A well-trained, experienced spine fellow, familiar with all the techniques, performed all the calculations. We analyzed the preoperative and immediate postoperative Cobb's angle and apical axial derotation as average correction and percentages of correction according to curve severity and disease groups (group A, B, and C) using analysis of variance (ANOVA) tests.
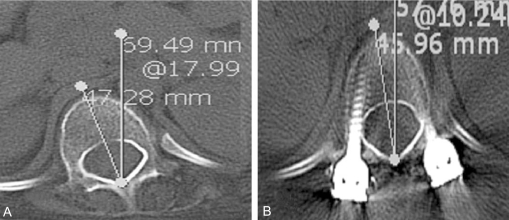
Measurement of axial rotation in the mid-sagittal plane CT scan (A) preoperative and (B) postoperative.
The correction in Cobb's angle, pelvic obliquity, and apical axial derotation were compared with a paired t-test for all groups. A p value of less than 0.05 was considered significant.
Results
The average follow-up was 26 months, ranging from 15 to 35 months. For the idiopathic scoliosis group, the average preoperative Cobb's angle, pelvic obliquity, and apical axial rotation were 57.3° (range, 46 to 80°), 2.8° (range, 0 to 8°) and 20.4° (range, 9 to 36°), respectively. Postoperatively, the average Cobb's angle, pelvic obliquity, and apical axial rotation were 16.8°, 1.1°, and 14.7° respectively. After surgery, the average correction was 71.4% (p<0.0001, paired t-test) for postoperative Cobb's angle, 51.1% (p=0.006, paired t-test) for pelvic obliquity, and 31.3% (p=0.002, paired t-test) for apical axial rotation (Table 1).
Similarly for the NMS group, the average preoperative Cobb's angle, pelvic obliquity, and apical axial rotation were 75.6° (range, 40 to 112°), 13.7° (range, 1 to 27°) and 42.9° (range, 15 to 72°), respectively. Postoperatively, the average Cobb's angle, pelvic obliquity, and apical axial rotation were 27.1°, 5.8°, and 34.1°, respectively. After surgery, the average correction was 65.1% (p<0.0001, paired t-test) for Cobb's angle, 49.3% (p=0.0008, paired t-test) for pelvic obliquity, and 18.3% (p=0.0003, paired t-test) for apical axial rotation (Table 2).
The correction rates were not different in the idiopathic and neuromuscular groups (Cobb's angle p=0.306, pelvic obliquity p=0.887 and apical derotation p=0.113; unpaired t-test), despite less correction in apical rotation overall in NMS. Clinically, all patients exhibited postoperative improvement in walking ability, cosmetic appearance, and/or sitting balance, which improved quality of life.
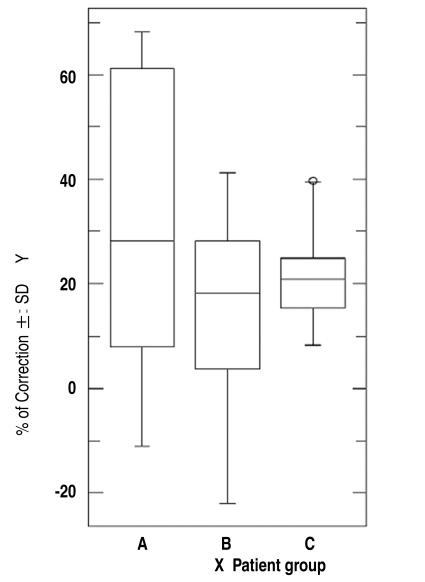
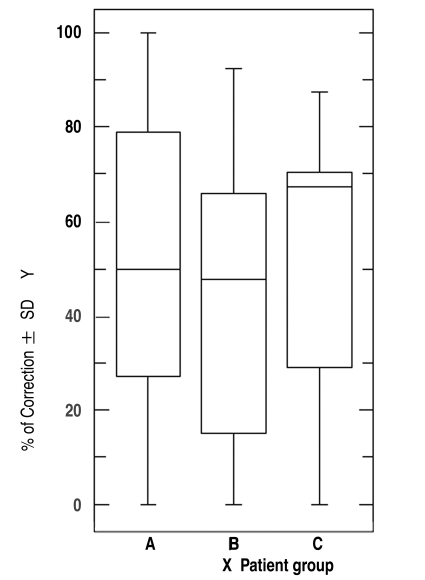
The correction in Cobb's angle was significantly different in the three groups (p=0.04, ANOVA test) (Fig. 2) while correction in pelvic obliquity (p=0.79, ANOVA test) (Fig. 3) and apical derotation (p=0.25, ANOVA test) (Fig. 4) were not. Additionally we also compared the effect of correction in three diseases of NMS group: CP, DMD and SMA. The three different disease types, CP, DMD, and SMA, did not show differences in Cobb's angle (p=0.54), pelvic obliquity (p=0.10) or apical derotation (p=0.46) by ANOVA.

Graph for analysis for Cobb's angle. The X-axis denotes scoliosis groups: A: AIS group, B: NMS <80°, and C; NMS >80°. The Y-axis denotes % of correction in Cobb's angle with SD.
Graph for analysis for pelvic obliquity. The X-axis denotes scoliosis groups: A: AIS group, B: NMS <80°, and C; NMS >80°. The Y-axis denotes % of correction in pelvic obliquity with SD.
Discussion
Although, the apical vertebra shows maximum rotation9, the upper and lower end vertebrae also exhibit rotational components in scoliosis. The vertebral and inter-vertebral axial rotation10 indicates the severity and rigidity of the scoliosis curve. Surgical success depends on the correction of the Cobb's angle, rotational angle, and translation of the vertebrae. Apical rotation outcomes are typically investigated in idiopathic scoliosis11,12 in the literature, with no reported outcomes in the neuromuscular group, probably because of the relatively small number of cases.
Here we have compared apical axial derotation in neuromuscular and AIS groups. Although different methods can measure the axial rotation of vertebrae12-15, computerized tomography is the most accurate. Since the pioneering work of Aaro-Dahlborn4,8 in 1980 to measure axial rotation on CT scans, several other methods have been developed to measure axial rotation. Gocen et al.16 in 1999 used a new technique to measure axial rotation by CT scan. Krismer et al.10 studied 11 cadavers and found that the Aaro-Dahlborn method was superior to other techniques. We used the same method here.
Moreover, surgical correction with modern techniques is three-dimensional17. Aaro-Dahlborn3 evaluated 33 patients treated with Harrington instrumentation and found no axial derotation. Marchesi et al.18 used CT scans to measure derotation in four idiopathic scoliosis patients treated with Harrington instrumentation, plus seven with Luque instrumentation, and found an average derotation of 16% and 12%, respectively, in the apical vertebrae. Using the same instrumentation, Ecker et al.19 found only 14% corrections with increase in rotation in some vertebrae. Bipedicular instrumentation can achieve maximum correction in Cobb's angle as well as axial rotation. In 1996, Jarvis and Greene20 studied Wisconsin segmental spinal instrumentation, a hybrid system with Harrington distraction rods, Luque rods, and button-wire constructs, in 24 idiopathic scoliosis patients and found 23% derotation in 22 curves and 12% deterioration in seven curves. They included double-curve patterns, which we excluded. Cundy et al.21 used the Aaro-Dahlborn method to study the effect of Cotrel-Dubosset instrumentation on rotation in 34 idiopathic scoliosis patients and reported 24% derotation in relation to the mid-sagittal plane. Suk et al.22 in 1995 first proposed the use of thoracic pedicle screws as a fixation option for treatment of AIS. Lonstein et al.23 in 1999, while studying coronal and sagittal plane correction in AIS using pedicle screw constructs or hybrid thoracic hook lumbar constructs noted a trend towards better correction of the main thoracic curve with pedicle screws, as was subsequently seen for lumbar curves as well24,25. Here we found a 71.4% correction in the coronal plane and a 31.3% derotation in the axial plane for AIS and a 65.1% correction in the coronal plane and a 18.3% derotation in the axial plane for NMS, which were not different (p=0.30 for Cobb's angle and p=0.11 for apical derotation; unpaired t-test).
No published data exists on apical derotation in NMS. Schufflebarger et al.26 used CT scan to measure rotation in relation to the mid sagittal plane in 18 patients with NMS using Cotrel-Dubosset instrumentation with fixation up to the pelvis. His findings reveal an average correction in the frontal plane of 36°, a 42% correction, but did not measure axial rotation. Steib et al.24 studied derotation by in situ contouring of rods with pedicle screws in thoracic and lumbar curves in 10 idiopathic and 10 degenerative scoliosis patients and noted derotation ranging from 8° to 10° (62% to 67%). Although we used in situ contouring in a few cases, our main purpose was to prevent screw loosening from the pedicle. In 2003 Aubin et al.27 studied biomechanical modeling of posterior instrumentation of the scoliotic spine with Cotrel-Dubosset instrumentation using a three step procedure, and noted 18° derotation in apical vertebrae, reflecting the kinematics of the rod-implant-vertebrae joint. Our all-pedicle screw construct with a posterior only approach produced comparable results with a similar derotation maneuver. In 2003, Basobas et al.28 demonstrated excellent results for selective anterior fusion for the treatment of NMS in 20 patients (most with meningomyelocele) in their retrospective study, but they did not comment on rotation. In 2002, Rhee et al.29 did not find a difference in their sagittal plane comparison of AIS after anterior versus posterior instrumentation in 110 patients. Laohachroensombat et al.30 found a significant difference in apical derotation (45%) in three dimensions after inserting pedicular screw plate constructs in 25 idiopathic scoliosis patients.
We achieved nearly the same derotation in the CP, DMD, and SMA groups (p=0.46, ANOVA test), although we had small sample sizes and the results may depend on scoliosis severity. However, we found a 31% correction in apical rotation in the AIS group, but only an 18% change in the neuromuscular group.
Conclusions
In our retrospective study, we attained comparable changes in apical axial derotation in both groups, as well as in comparison of the AIS group with two severities of NMS. Although correction in the coronal plane was different among the groups A, B and C (p=0.04, ANOVA test), we noted similar derotations in the apical vertebrae. There is no other apical derotation data for NMS in the literature. However, the pedicle screw construct produces satisfactory outcomes in idiopathic scoliosis, prompting interest in future comparison studies of these two types of scoliosis.