Kyphotic Angle Progression of Thoracic and Thoracolumbar Tuberculous Spondylitis after Surgical Treatment: Comparison with Predicted Kyphosis Outcome after Conservative Treatment
Article information
Abstract
Study Design
Retrospective comparative study.
Purpose
To compare the progression of the kyphotic angle (KA) in a surgically treated group with the predicted outcome of a conservatively treated group.
Overview of Literature
Late onset kyphosis is a complication of tuberculous spondylitis making its prevention a major goal of surgery.
Methods
Twenty six consecutive patients underwent an anterior reconstruction and posterior instrumented fusion in conjunction with antituberculous chemotherapy. The mean follow up was 56 months (range, 28 to 112 months). The patients were divided into subgroups based on the involved region of the thoracic and the thoracolumbar spine, initial KA, and the initial vertebral body loss (VBL(x)). The predicted KA (KAPd) was calculated using the formula, KAPd=5.5+30.5 VBL(x), to predict the final gibbus deformity. Kyphotic angle progression (ΔKA) based on the radiographic measurements after surgery (ΔKAR), and the predicted outcome of conservative treatment (ΔKAP) with chemotherapy were compared.
Results
Among the subgroups of the regions involved and initial KA, the ΔKA was radiographically superior with a reduced amount of kyphogenesis in the surgery group than the predicted outcome of the conservatively treated patients (p<0.05). The radiographic ΔKA was similar (p>0.05) with VBL(x)≤0.5 in the VBL(x) subgroup.
Conclusions
These results showed that in the VBL(x) subgroup, an initial VBL(x)≤0.5 is an indication of conservative antituberculous chemotherapy without surgery.
Introduction
Kyphosis and paralysis are the major outcomes of spinal tuberculosis (TB). Spinal TB can stabilize spontaneously without progression of the deformity. However, the development of a kyphotic deformity is a serious complication. It is not only cosmetically unpleasant but also impairs the cardiopulmonary function, causes pain from nerve impingement between the ribs and pelvis, and/or causes late-onset paraplegia. A severely deformed kyphosis can be treated only by corrective surgery. However, this is a challenging option with a high complication rate1. A kyphotic deformity can be prevented if spinal TB is diagnosed early and antituberculosis chemotherapy is administered promptly. However, some kyphotic deformity may still develop even with adequate medical treatment. The sequela of a kyphotic deformity has been a subject of research into the treatment of patients with spinal TB.
The fifth report of the Medical Research Council Working Party on Tuberculosis of the Spine (MRC)2 stated the following: 1) a kyphotic deformity develops most severely in the thoracic spine region, which is followed in order by the thoracolumbar, lumbar and lumbosacral spine after treatment with standard TB medications; 2) the greater the pretreatment kyphotic deformity, the less likely the kyphosis will progress further after initiating treatment; and 3) further collapse is appreciable when the initial vertebral body loss upon admission was small (< 2 vertebrae), while the initial vertebral body loss of two or three segments showed no further collapse on average2.
Rajasekaran and Shanmugasundaram3 reported that kyphosis progresses gradually in the thoracic and thoracolumbar spine above L2 during conservative treatment with anti-tuberculous chemotherapy. Regarding the degree of kyphogenesis, the initial vertebral body loss (VBL(x)) was considered to be the determining factor, while the initial kyphotic angle (KA) was not. A predicted KA (KAPd) was formulated as 'KAPd=5.5+30.5VBL(x)' with a correlation coefficient of 0.83 and an accuracy of 90%. This formula applies to the thoracic and thoracolumbar region above L2, which forms a normal kyphotic curve. In the lumbar spine, the lordotic curvature contributes to the progression of the deformity in the thoracic spine4.
This study examined the change in the sagittal profile after surgical treatment in tuberculous (Tbc) spondylitis patients, and compared it with the predicted change of the sagittal profile after chemotherapy alone. It is believed that the indications for surgery or conservative treatment might be better determined using this information.
Materials and Methods
1. Patients
This study was approved by the institutional review board. Twenty six patients (M:F=12:14) were examined after undergoing surgery for thoracic and thoracolumbar TB between 1992 and 2001. The mean follow up period and age was 56 months (range, 28 to 112 months) and 41.7 years (range, 18 to 73 years), respectively. The regional subgroups included 12 and 14 cases in the thoracic (T: from T2 to T10) and thoracolumbar (TL: from T11 to L2), respectively.
2. Operation method
Anterior radical surgery with an autogenous iliac bone graft was performed in all cases, and posterior instrumentation (TSRH™; Texas Scotish Rite Hospital, Medtronic-Sofamor Danek, Memphis, TN, USA) and fusion were performed using an autogenous cancellous bone graft.
3. Measurement
The KA progressions (ΔKA)'s were obtained. ΔKA following surgery (ΔKAR) was measured by comparison of the difference in the kyphotic angle of the last follow up standing lateral radiograph (KAFinal) to the preoperative standing lateral radiograph (KAPre) (Table 1). The radiographic measurements were performed by two independent spine surgeons that did not participate in the surgery. Each surgeon performed the measurements twice; the mean of the measurements was used as the final value. The KAPd, or the final gibbus deformity, was calculated using the formula 'KAPd=5.5+30.5 VBL(x)' by measuring the VBL(x). The estimated KAPd was calculated presuming that only antituberculous chemotherapy was administered as conservative treatment. Predicted kyphotic angle progression (ΔKAP) was calculated by difference of KAPd and KAPre (Table 1).
(1) Measurement of the kyphotic angle
The measured KA angle was the Cobb's angle between the upper border of the upper normal vertebra and the lower border of the lower normal vertebra on a simple standing lateral radiograph of the lesion, as previously reported by the MRC2,5,6.
(2) Measurement of the preoperative VBL(x)
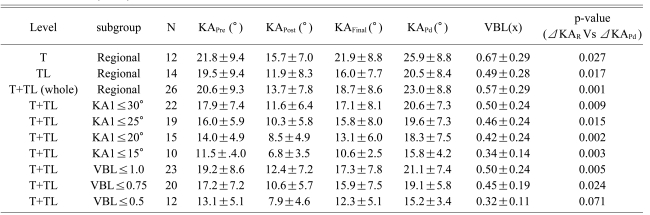
Rajasekaran and Shanmugasundaram3 assessed the loss of the vertebral body, which we regarded as VBL1, using the following method: divide the lateral height of each vertebra into 10 equal parts on a lateral radiograph; measure the loss of height in tenths from each vertebra; and add the loss of height proportions from each vertebra. The sum of the destroyed portions (ΣVBLi) from the affected vertebrae was the VBL1 (Fig. 1).
The diagram shows the method used to assess the preoperative initial vertebral body loss (VBL(x)). (A) VBL1 was defined as the fractional loss of the vertebral body area. When more than one vertebra was involved, the sum of each loss (ΣVBLi) was calculated as the VBL1. (B) VBL2 was defined as the fractional loss of the anterior vertebral body height, assuming that the original anterior vertebral height (H) was the arithmetic mean of the anterior height of the upper (a) and lower (b) normal vertebral bodies. In this study the arithmetic mean of VBL1 and VBL2 was used as the 'VBL(x)'.
Jain et al.7 proposed a different method for assessing the loss of the vertebral body, which we regarded as VBL2. Presumed normal anterior height (H) of the affected vertebral body was arithmetic mean of the anterior heights of the upper and lower normal vertebral bodies. The loss of the anterior height was calculated by subtracting the measured height from the H. The anterior height loss per affected vertebral body, was then summed to obtain the total height loss (ΣVBLi). The VBL2 was the ratio of ΣVBLi to H. In this study, the arithmetic mean of the above mentioned two calculations was used as the initial vertebral body loss: VBL(x) = (VBL1+VBL2)/2 (Fig. 1).
4. Patient assessment by subgroup
The patients were divided into three independent subgroups. The first subgroup was based on the region affected: thoracic (T) (n=12), thoracolumbar (TL) (n=14) and combined (T+TL) (n=26). The second subgroup was based on the KAPre: KAPre≤30°(n=22), KAPre≤25°(n=19), KAPre≤20°(n=15), and KAPre≤15°(n=10). The third subgroup was based on the VBL(x): VBL(x)≤1.0 (n=23), VBL(x)≤0.75 (n=20), and VBL(x)≤0.5 (n=12). The 'T+TL' group refers to all patients. The range was set by the authors to include a gradual increase in the range in an attempt to identify the threshold values to use as guidelines, assuming that that the increase in KA and VBL(x) were associated with the progression of the disease.
For each subgroup, the ΔKAR and ΔKAP were compared using a paired t-test. A p-value<0.05 was considered significant (SPSS ver. 10.0; SPSS Inc., Chicago, IL, USA).
Results
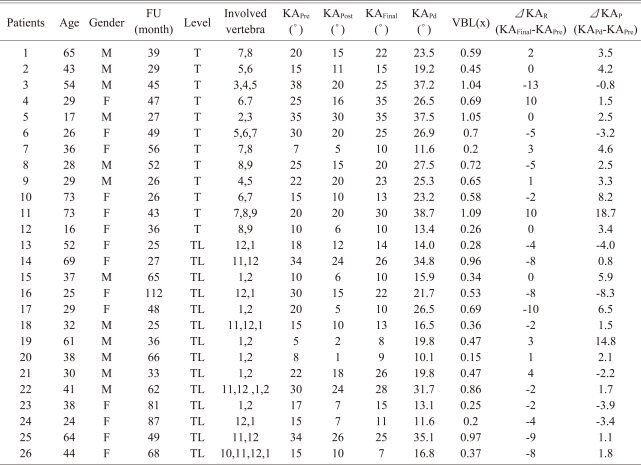
A mean of 2.4(2-4) vertebral bodies were affected by bone destruction. Preoperative Pott's paraplegia and paraparesis were observed in 8 of the 26 patients. Table 1 lists the patient demographic information.
1. Regional subgroups
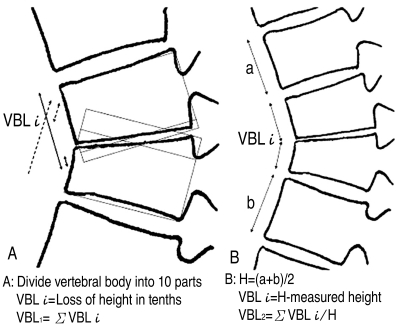
In the T group, the KAPre, KAFinal and KAPd was 21.8°±9.4°, 21.9°±8.8° and 25.9°±8.8°, respectively. The radiographically measured kyphotic angle progression (ΔKAR) and predicted kyphotic angle progression (ΔKAP) were significantly different (p=0.027) (Fig. 2, Table 2).

Comparison of the kyphotic angle (KA) progression (ΔKA) in the subgroups: thoracic (T), thoracolumbar (TL), and combined (T+TL) groups. The surgical ΔKA (ΔKAR) was significantly smaller than the predicted ΔKA (ΔKAP) which is the predicted outcome of conservative treatment: p=0.027 (T); p=0.017 (TL); and p=0.001 (T+TL).
In the TL group, the KAPre, KAFinal and KAPd was 19.5°±9.4°, 16.0°±7.7° and 20.5°±8.4°, respectively. A comparison of the kyphotic angle progression between ΔKAR and ΔKAP showed a significant difference (p=0.017) (Fig. 2, Table 2).
For the T-TL group, which represents the entire cohort, the KAPre, KAFinal and KAPd was 20.6°±9.3°, 18.7°±8.6° and 23.0°±8.8°, respectively. The ΔKAR was significantly smaller than the ΔKAP (p=0.001) (Fig.2, Table 2).
2. KA subgroup
For the KAPre≤30°group, the KAPre KAFinal and KAPd was 17.9°±7.4°, 17.1°±8.1°, and 20.6°±7.3°, respectively (Table 2). The ΔKAR was significantly smaller than the ΔKAP (p=0.001). Each subgroup of KA was analyzed to determine if the ΔKAR was significantly smaller than the predicted outcome, a kyphogenesis of ΔKAPd (Fig.3, Table 2).

Comparison of the ΔKA by the preoperative KA (KAPre) subgroups. For the subgroups of 'KAPre≤30°', 'KAPre≤25°', 'KAPre≤20°', and 'KAPre≤15°', the surgical ΔKA (ΔKAR) was significantly smaller than the predicted ΔKA (ΔKAP): p=0.009 (KAPre≤30°); p=0.015 (KAPre≤25°); p=0.002 (KAPre≤20°); and p=0.003 (KAPr≤15°), respectively.
3. VBL(x) subgroup
In the VBL(x)≤1.0 group, the KAPre KAFinal and KAPd was 19.2°±8.6°, 17.3°±7.8°, and 21.1°±7.4°, respectively. The ΔKAR was significantly smaller than the ΔKAP (p=0.005). In the VBL(x)≤ 0.75 group, the ΔKAR was significantly smaller than the ΔKAP (p=0.024) (Fig. 4, Table 2).
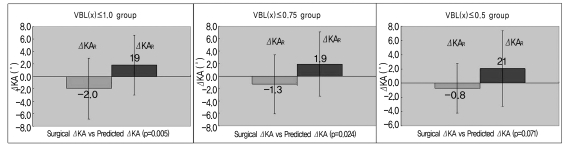
Comparison of ΔKA in the VBL(x) subgroups ('VBL(x)≤1.0', 'VBL(x)≤0.75', and 'VBL(x)≤0.5'). In the 'VBL(x)≤0.5' group, the ΔKAR was not significantly different from the ΔKAP which is the predicted KA after conservative treatment (p=0.071). In the other groups, ΔKAR was significantly smaller than ΔKAP, indicating smaller amount of kyphogenesis in the surgical group: p=0.005 (VBL(x)≤1.0); and p=0.024 (VBL(x)≤0.75).
However, in the VBL(x)≤0.5 group, the KAPre KAFinal and KAPd was 13.1°±5.1°, 12.3°±5.1° and 15.2°±3.4°, respectively (Table 2). The ΔKAR and ΔKAP were similar (p=0.071) (Fig. 4, Table 2).
Discussion
The fifth MRC report of a 5-year follow-up2 showed that ambulatory antituberculous chemotherapy was successful when compared with combined bed rest for six months, or a plaster-of-Paris jacket for nine months. Antituberculous medication was used for 18 months, and the regimen included isoniazid and para-aminosalicylic acid with or without additional streptomycin during the first three months2. Tull and Kumar8, Tuli9 reported that only 19% of patients showed progression of their kyphotic deformity>10° after rest and conservative treatment with antituberculous drugs.
The sixth MRC report of a 5-year follow-up10 showed similarly favorable results with ambulatory chemotherapy versus debridement, as well as with debridement versus radical treatment with autologous bone graft reconstruction. The favorable results included the following: return to physical activity, absence of neurological abnormalities, absence of abscess formation, absence of the development of sinus tracts, and the presence of radiographically quiescent spinal lesions10.
The eighth MRC report after a 10-year follow-up6 compared a radical anterior autologous bone reconstruction with debridement of the abnormal tissue leaving the apparently unaffected bone. The sagittal profile was superior after the radical series compared to after the debridement cases. Vertebral body loss increased by 0.05 for the radical cases, while it increased by 0.23 for the debridement cases. The KA decreased by 1.4° for the radical cases, whereas for the debridement cases, it increased by 9.8° in the thoracic and thoracolumbar lesions. The KA decreased by 0.5° in the radical cases, whereas it increased by 7.6° for the debridement cases with lumbar lesions.
The bone loss and increase in KA usually occurred within the first 18 months from the initial diagnosis and treatment. Upadhyay et al.11 reported that anterior column support resulted in less kyphotic deformity than simple anterior debridement. Rajasekaran and Shanmugasundarm12 reported less kyphogenesis with little bone loss in the single-segment lesions than in multi-segment lesions.
Firm fixation is essential for the healing of bone infections and bone fusion, and cast immobilization has been used to treat vertebral infections. The development of instruments has led to successful treatment by instrumented fusion for vertebral infections. Moon et al.13 reported that the kyphosis could be corrected and maintained effectively in adult spinal TB by adding posterior instrumented fusion. Sundararaj et al.14 reported the following advantages of adjuvant posterior instrumented fusion: prevention of graft dislodgement; correcting and maintaining the kyphosis; resulting in a superior outcome for intervertebral bone fusion. No additional risk was found for persistent infections due to the posterior instrumentation14,15. For pyogenic infections, internally fixed metal appliances facilitate the attachment and proliferation of microbes, forms a biofilm on the surface of the metal and prevents antibiotics from reaching the infection and/or inflammation and thereby healing. This occasionally necessitates removal of the metal implants16. Ha et al.17 performed an in-vitro experiment and reported much greater adherence and multiplication of biofilm formation on the metal segments with Staphylococcus epidermidis strains than in Mycobacterium tuberculosis strains. They demonstrated a more favorable environment for instrumentation in the treatment of Tbc spondylitis. Instrumentation to the posterior side, which is opposite to the initial infection, is not considered to be harmful17.
For measuring the VBL(x), Rajasekaran and Shanmugasundaram3 divided each affected vertebral body into 10 parts (Fig. 1). This calculation led to frequent ambiguity and arbitrary measurements because severely damaged vertebrae often do not have definite borders7. On the other hand, Jain et al.7 used the arithmetic mean from the anterior heights of the upper and lower vertebrae, which were normal, as the 'presumed normal anterior height' at the affected level. The 'anterior height loss' is the difference between the presumed normal height and actual height measured. In lesions at multiple levels, the anterior height losses were added to obtain the 'total height loss'. The 'initial vertebral body loss' is the ratio between the 'total height loss' to the 'presumed normal anterior height'. Jain et al.7 suggested an approximate 76% accuracy using their method for conservative treatment. However, this method may not reflect the precise vertebral body loss if the anterior cortical bone is spared selectively in the lesion distribution. In this study, the arithmetic mean of the above two calculations for the VBL (x was used) to ameliorate the shortcomings of each (Fig. 1).
The results showed significantly less thoracic KA progression after surgery than the predicted outcome after conservative treatment: (ΔKAR=0.1°±6.3° vs. ΔKAP=4.1°±5.4v; p=0.006). In addition, the thoracolumbar KA progression was significantly less after surgery than after the predicted-conservative treatment: (ΔKAR=-3.5°±4.6°vs. ΔKAP=1.0°±5.6°; p=0.000). The KA progression of the entire cohort including the thoracic and thoracolumbar spine subgroups was significantly less after surgery than after the predicted outcome with conservative treatment: (ΔKAR=-1.8°±5.6° vs. ΔKAP= 2.4°±5.6°; p=0.001). The results suggest that surgical treatment was justified based on the sagittal profile outcome because the ΔKAR, which represents the kyphotic angle progression after surgery, was significantly smaller than the ΔKAP, which represents the kyphotic angle progression in the formula for predicting the outcome.
For the KA subgroup, all subgroups with a 'KA≤30°', 'KA≤20°' and 'KA≤15°' showed a significantly smaller ΔKAR than ΔKAP, suggesting less kyphotic angle progression after surgical treatment than after the predicted outcome of conservative treatment-alone. The same conclusion in all KA subgroups confirms the efficacy of surgical treatment. However, the KA subgroup results did not suggest a range in which conservative treatment-alone might be justified.
For the VBL(x) subgroup, the ΔKAR and the ΔKAP were not significantly different in the 'VBL(x)≤0.5' subgroup (p=0.071). This suggests that the surgical treatment group did not have a significantly superior sagittal profile compared to the predicted outcome of conservative treatment. As the progression of kyphosis was the main concern for the surgical treatment of Tbc spondylitis, conservative treatment might be indicated initially in patients identified with a VBL(x)≤0.5. The other VBL(x) subgroups showed that the ΔKAR was significantly smaller than the ΔKAP, justifying surgical treatment for improved outcome on the sagittal profile. The surgical treatment used in all cases was an anterior-posterior combined surgery (anterior decompression, interbody fusion, and posterior instrumented fusion with bone graft) (Fig. 5). The KA was corrected substantially by the combined anterior column support and posterior instrumentation and the correction was maintained.

A 26-year-old female patient with T 5-7 Tbc spondylitis, with a VBL(x) of 0.7: the KAPre was 30° before surgery and final postoperative KA (KAFinal) was 25°. The predicted KA (KAPd) was 26.9°.
The limitations of this study include the following. The control group consisted of theoretical, calculated, results. The accuracy of the 'equation' requires further statistical validation to be considered a reliable control group. However, in a limited cohort with a small number of patients, different patients with the same KA and VBL(x) might include a range of factors, such as co-morbidities that reduce the homogeneity of the group, which bias the comparison. This study compared the surgical and predicted results on the same patient. The VBL(x) was calculated by taking the mean of the two methods but this value requires further validation. In addition to the sagittal profile discussed in this study, the presence of neurological complications would be an additional independent factor indicating a need for surgical treatment. Subsidence at the anterior strut graft would be likely to occur due to endplate injury either by the disease process or by the surgical procedure, even though the disc space is destroyed less aggressively compared to the pathogenesis of pyogenic spondylitis18. This endplate -associated subsidence might explain some of the variance of the subsidence observed in our data. However, the statistical analysis still leads to certain conclusions based on a comparison of the two groups. In subgroup analysis, conservative treatment appears to be warranted with an initial VBL(x) of ≤0.5. Nevertheless, the KA subgrouping did not suggest guidelines for conservative treatment. Further study with a larger cohort would enable statistical analysis to improve the categorization of patients, as well as a comparison of surgically and medically treated groups.
Conclusions
For patients with thoracic and thoracolumbar Tbc spondylitis, surgical treatment was more effective for kyphosis correction than the predicted outcome of conservative treatment. An initial VBL(x) of ≤0.5 on the sagittal profile after surgical treatment was not significantly superior to the outcome predicted by conservative treatment. The KA is not a parameter that can be used to determine whether to perform surgical treatment. These results suggest that a VBL(x) of ≤0.5 is an indication for conservative antituberculous chemotherapy.