1. Herkowitz HN, Kurz LT. Degenerative lumbar spondylolisthesis with spinal stenosis. A prospective study comparing decompression with decompression and intertransverse process arthrodesis. J Bone Joint Surg Am 1991 73:802ŌĆō808. PMID:
2071615.


2. Lee CK. Lumbar spinal instability (olisthesis) after extensive posterior spinal decompression. Spine (Phila Pa 1976) 1983 8:429ŌĆō433. PMID:
6635793.


3. Herron LD, Trippi AC. L4-5 degenerative spondylolisthesis. The results of treatment by decompressive laminectomy without fusion. Spine (Phila Pa 1976) 1989 14:534ŌĆō538. PMID:
2727798.


4. Carragee EJ. Single-level posterolateral arthrodesis, with or without posterior decompression, for the treatment of isthmic spondylolisthesis in adults. A prospective, randomized study. J Bone Joint Surg Am 1997 79:1175ŌĆō1180. PMID:
9278077.


5. Deguchi M, Rapoff AJ, Zdeblick TA. Posterolateral fusion for isthmic spondylolisthesis in adults: analysis of fusion rate and clinical results. J Spinal Disord 1998 11:459ŌĆō464. PMID:
9884288.


6. Greenough CG, Peterson MD, Hadlow S, Fraser RD. Instrumented posterolateral lumbar fusion. Results and comparison with anterior interbody fusion. Spine (Phila Pa 1976) 1998 23:479ŌĆō486. PMID:
9516705.


7. Schnee CL, Freese A, Ansell LV. Outcome analysis for adults with spondylolisthesis treated with posterolateral fusion and transpedicular screw fixation. J Neurosurg 1997 86:56ŌĆō63. PMID:
8988082.


8. Chow DH, Luk KD, Evans JH, Leong JC. Effects of short anterior lumbar interbody fusion on biomechanics of neighboring unfused segments. Spine (Phila Pa 1976) 1996 21:549ŌĆō555. PMID:
8852308.


9. Inoue S, Watanabe T, Hirose A, et al. Anterior discectomy and interbody fusion for lumbar disc herniation. A review of 350 cases. Clin Orthop Relat Res 1984 (183): 22ŌĆō31. PMID:
6697590.
10. Takahashi K, Kitahara H, Yamagata M, et al. Long-term results of anterior interbody fusion for treatment of degenerative spondylolisthesis. Spine (Phila Pa 1976) 1990 15:1211ŌĆō1215. PMID:
2267618.


11. Tsuji H,Tsuji H,Lumbar spine instability and surgical strategy. editors. Comprehensive atlas of lumbar spine surgery. 1991.St. Louis: Mosby-Year Book; p.12ŌĆō27.
12. Motosuneya T, Asazuma T, Nobuta M, Masuoka K, Ichimura S, Fujikawa K. Anterior lumbar interbody fusion: changes in area of the dural tube, disc height, and prevalence of cauda equina adhesion in magnetic resonance images. J Spinal Disord Tech 2005 18:18ŌĆō22. PMID:
15687847.


13. Chen D, Fay LA, Lok J, Yuan P, Edwards WT, Yuan HA. Increasing neuroforaminal volume by anterior interbody distraction in degenerative lumbar spine. Spine (Phila Pa 1976) 1995 20:74ŌĆō79. PMID:
7709283.


14. Christensen FB, Karlsmose B, Hansen ES, B├╝nger CE. Radiological and functional outcome after anterior lumbar interbody spinal fusion. Eur Spine J 1996 5:293ŌĆō298. PMID:
8915633.


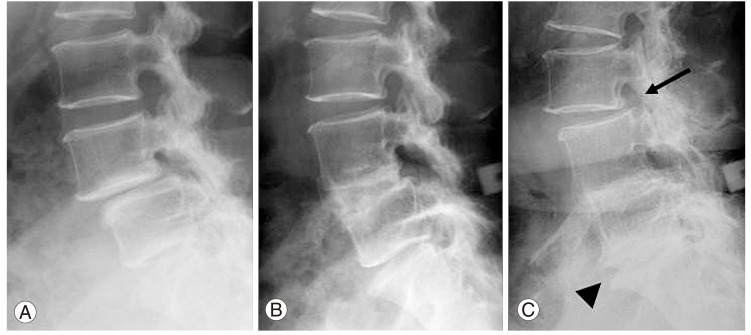
15. Tsuji H, Hirano N, Katoh Y, et al. Ceramic interspinous block (CISB) assisted anterior interbody fusion. J Spinal Disord 1990 3:77ŌĆō86. PMID:
2134415.


16. Tsuji H, Hirano N, Matsui H, et al,Tsuji H, Hirano N, Matsui H, ,Effects of ceramic interspinous block on anterior lumbar interbody fusion. editors. Lumbar fusion and stabilization. 1994.Tokyo: Springer; p.220ŌĆō226.

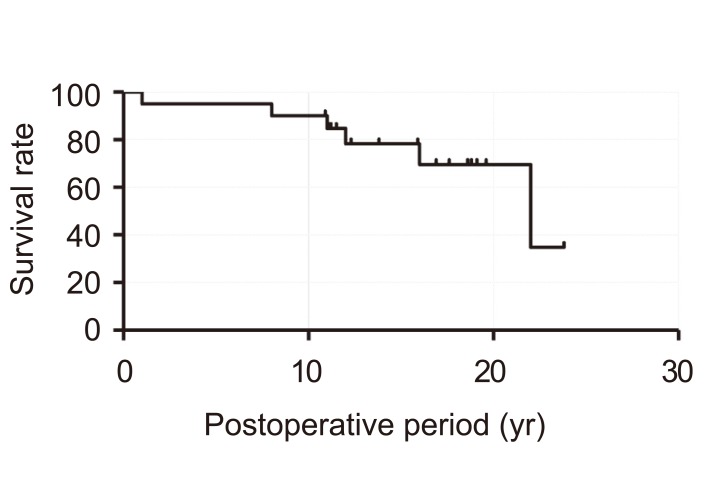
17. Ishihara H, Osada R, Kanamori M, et al. Minimum 10-year follow-up study of anterior lumbar interbody fusion for isthmic spondylolisthesis. J Spinal Disord 2001 14:91ŌĆō99. PMID:
11285419.


18. Kaplan EL, Meier P. Nonparametric estimation from incomplete observations. J Am Stat Assoc 1985 53:457ŌĆō481.

19. Taillard W. Spondylolisthesis in children and adolescents. Acta Orthop Scand 1954 24:115ŌĆō144. PMID:
13217798.


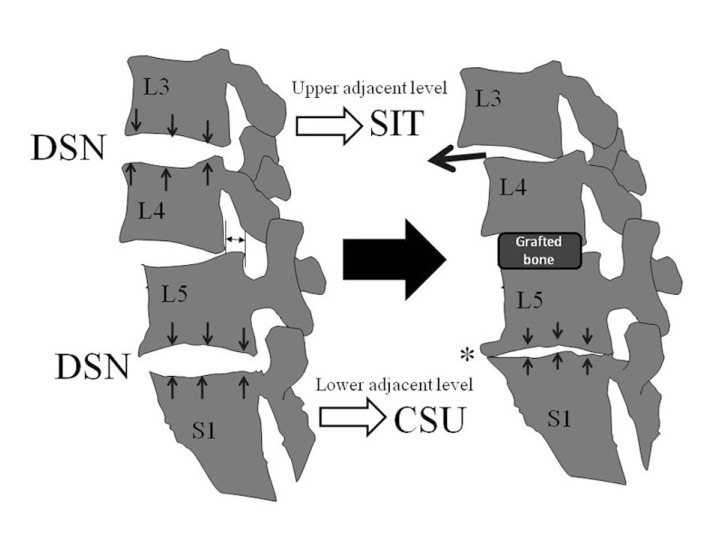
20. Kanamori M, Ishihara H, Kawaguchi Y, Yasuda T. H-shaped autologous bone graft associated with a ceramic interspinous block for the posterior lumbar fusion. J Jpn Soc Lumbar Spine Disord 2005 11:157ŌĆō163.

21. Kanamori M, Ishihara H, Kawaguchi Y, Ohmori K, Shigeta T. Posterior decompression for lumbar stenosis with spondylolisthesis. Cent Jpn J Orthop Traumatol 2002 45:717ŌĆō718.
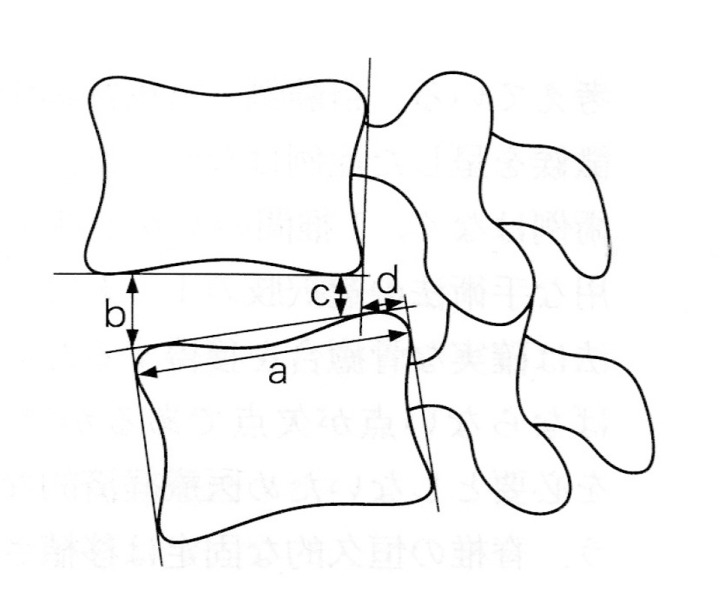
22. Motomura H, Kanamori M, Nobukiyo M. The relationship between lumbar vertebral disc height on plain radiography and disc degeneration evaluated with magnetic resonance imaging. J Jpn Soc Lumbar Spine Disord 2001 7:126ŌĆō131.

23. Dennis S, Watkins R, Landaker S, Dillin W, Springer D. Comparison of disc space heights after anterior lumbar interbody fusion. Spine (Phila Pa 1976) 1989 14:876ŌĆō878. PMID:
2781400.


24. Kumar A, Kozak JA, Doherty BJ, Dickson JH. Interspace distraction and graft subsidence after anterior lumbar fusion with femoral strut allograft. Spine (Phila Pa 1976) 1993 18:2393ŌĆō2400. PMID:
8303439.


25. Meyerding HW. Spondylolisthesis. Surg Gynec Obstet 1932 54:371ŌĆō377.
26. Panjabi MM, White AA,Panjabi MM, White AA,Kinematics of the spine. editors. Clinical biomechanics of the spine. 1978.Philadelphia: JB Lippincott; p.61ŌĆō90.
27. Johnsson KE, Redlund-Johnell I, Ud├®n A, Willner S. Preoperative and postoperative instability in lumbar spinal stenosis. Spine (Phila Pa 1976) 1989 14:591ŌĆō593. PMID:
2749373.


28. Phillips FM, Carlson GD, Bohlman HH, Hughes SS. Results of surgery for spinal stenosis adjacent to previous lumbar fusion. J Spinal Disord 2000 13:432ŌĆō437. PMID:
11052354.


29. Rahm MD, Hall BB. Adjacent-segment degeneration after lumbar fusion with instrumentation: a retrospective study. J Spinal Disord 1996 9:392ŌĆō400. PMID:
8938607.


30. Seitsalo S, Schlenzka D, Poussa M, Osterman K. Disc degeneration in young patients with isthmic spondylolisthesis treated operatively or conservatively: a long-term follow-up. Eur Spine J 1997 6:393ŌĆō397. PMID:
9455667.