Recurrent Malignant Fibrous Histiocytoma in Psoas Muscle: A Case Report
Article information
Abstract
Malignant fibrous histiocytoma is one of the most common sarcomas that occur in soft tissue, it usually develops in old age individuals and the incidence is similar between the genders. We report here on a case with invasive local recurrence after surgical resection of a malignant fibrous histiocytoma that occurred in the left psoas muscle of a 69-year-old male patient. The patient was first admitted to our hospital with a primary lesion in the left lower abdomen, as seen on magnetic resonance imaging. We report here on a rare case of a malignant fibrous histicytoma in the psoas muscle.
Introduction
Malignant fibrous histiocytoma has been regarded as one of the most common sarcoma tumors in soft tissue since the introduction of the concept of facultative fibroblasts by Ozzello et al. [1] in 1963. It is usually treated by orthopedic surgeons due to its nature and usual location. This tumor has a high likelihood of metastasis and recurrence, and as for its histologic features, the findings show spindle shaped or round cells that represent polymorphic cells, inflammatory cells and giant cells. The most common sites of occurrence are the upper and lower limbs followed by the chest and retroperitoneal cavity. The patients with occurrence in the retroperitoneal cavity sometimes do not have any symptoms and these tumors are often found in an advanced stage and especially for the rare cases where this tumor occurs in psoas muscle. Local recurrence after surgical removal of malignant fibrous histiocytoma has not yet been reported in Korea. Hence, we report here on a case of malignant fibrous histiocytoma that occurred in the left psoas and we review the relevant literature.
Case Report
We performed an examinationon a 69-year-old male patient who had left lower abdominal pain for the previous one month and we found a mass on the left psoas muscle (Fig. 1). The patient was diagnosed with malignant fibrous histiocytoma after performing radical excision and biopsy at our hospital, and the man refused postoperative chemotherapy and radiation therapy. At that time, the surgical resection marginal status was negative. After one year, a 3.0 × 3.0 × 1.6 cm size tumor at the L5-S1 level was observed in the back of the psoas muscle on an magnetic resonance imaging (MRI) examination with contrast medium, and this MRI was performed during outpatient follow-up. Under the diagnosis of recurrent malignant fibrous histiocytoma, reoperation was advised, but the patient refused surgery and he was managed without any special treatment. Sixteen months after surgery, outpatient MRI imaging showed an increase in size of the tumor to 5.0 × 6.7 × 3.7 cm (Fig. 2) along with radiating pain in the lower left leg at. Surgical treatment was again recommended, but the patient refused surgical treatment and returned home. Eighteen months after surgery, the patient was admitted to the emergency room complaining of severe pain in the left lower abdomen and radiating pain symptoms accompanied by paresthesia in the left lower leg. A physical examination showed no specific findings in the skin, and non-mobile adult fist-sized soft mass associated with tenderness was palpated. The plain radiographs did not show the findings of punctate calcification, and the chest computed tomography (CT) and brain MRI examination performed for the preoperative evaluation showed no distant metastasis to the lung or brain. MRI was performed using contrast media, and a huge mass 10.0 × 6.7 × 18.0 cm in size at the L3-S1 level was located in the left retroperitoneal cavity (Fig. 3). The findings showed the accelerated hypertrophy compared to the size of the mass at 16 months after surgery, and iliac involvement was also observed. We planned tumor resection with the anterior retroperitoneal approach with the patient in the lateral position by approaching the tumor from the left. Since the mass was located along the route of the left ureter, a ureteral double J stent was inserted into the left ureter to prepare if ureteral obstruction and damage occurred.
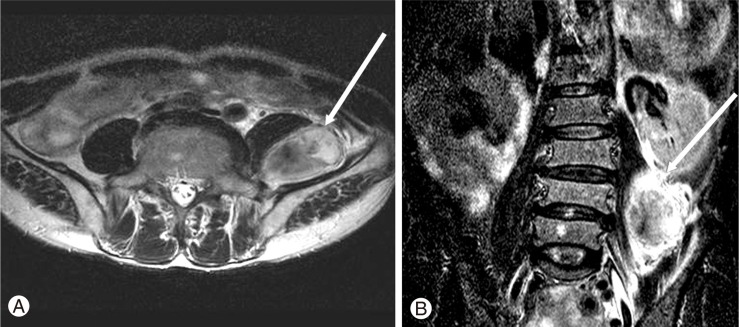
The T2-weighted magnetic resonance imaging image shows a well demarcated, heterogenous, round mass with high signal intensity. (A) T2 weighted axial image. (B) T2 weighted coronal image.
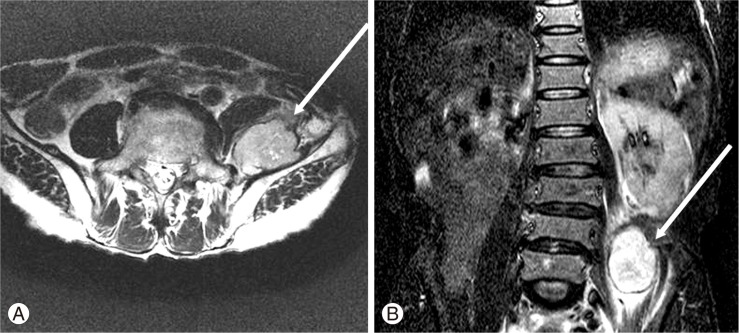
A heterogenously enhanced mass lesion (5 × 6.7 × 3.7 cm) is seen between the left psoas muscle and iliacus muscle at the L5-S1 level. (A) T2 weighted axial image. (B) T2 weighted coronal image.

A heterogenously enhanced mass lesion (10 × 6.7 × 18 cm) is seen between the left psoas muscle and iliacus muscle at the L3, 4, 5, S1 level with direct invasion of iliac bone. (A) T2 weighted axial image. (B) T2 weighted coronal image. (C) T2 weighted sagittal image.
The intraoperative findings showed severe peritoneal adhesions due to the previous surgery. It was very difficult to access the retroperitoneal cavity and the tumor was in the anterior peritoneal wall and it was pressing on the peritoneal cavity. Unlike the well-demarcated mass encapsulated with a membrane that was observed in the previous surgery, the mass showed the findings of partial septation by a thick, tough capsule. The mass had irregular margins and we confirmed the findings of iliac involvement that was visible on magnetic resonance imaging.
The gross findings showed that the resection surface appeared slightly light gray with internal hemorrhage, necrosis and mucinous degeneration (Fig. 4A).

(A) The mass is partially encapsulated by thick fibrous tissues. The largest fragment of the mass measures 14.0 × 8.0 × 6.0 cm. The cut surface of the mass is lobulated, creamy white and firm. Hemorrhage, necrosis and myxoid changes are present. (B, C) Diffuse bizarre storiform cells and spindle cells are seen. (B) H&E, ×200. (C) H&E, ×400.
On the microscopic examination, diffuse irregular round cells and spindle tumor cells, a fibrous and mucinous matrix and frequent cell divisions were observed (Fig. 4B and 4C). Based on the pathologic findings, the tumor was diagnosed as pleomorphic malignant fibrous histiocytoma. After surgery, the patient's dull left lower abdominal pain and radiating pain in the lower left leg improved and he was referred to a medical oncologist for radiation therapy.
Discussion
Malignant fibrous histiocytoma is the most common soft tissue sarcoma, and this generally occurs in 50-70-year-old people, but it can occur in a young adults [2].
The most common symptom is a painless mass, and the patients with this tumor mainly complain about fatigue, weight loss and abdominal pain and specifically in the cases of abdominal and retroperitoneal malignant fibrous histiocytoma, and this can lead to hematuria, lower extremity pain, abdominal distension, varicose veins and hernia. Another recent case report described a patient with an iliopsoas compartment tumor the patient presented with pain in the ipsilateral groin and testicular regions [3].
Our patient was managed without any symptoms for approximately 16 months after performing resection and then he complained of left lower abdominal pain as the hypertrophy of the mass accelerated at 18 months after surgery. We think the symptoms were mild when the tumor was small, but the symptoms were aggravated due to the increase in abdominal pressure as the tumor size increased.
Malignant fibrous histiocytoma generally refers to the group of tumors that originate from histiocytes, and making the specific diagnosis is difficult since these lesions have a variety of pathological types. Malignant fibrous histiocytoma usually consists of three types of cells: spindle shaped cells, round cells and giant cells. The pathologic findings greatly vary and it can be classified into five types depending on the distribution of these cells: the storiform-pleomorphic type, the myxoid type, the giant cell type, the inflammatory cell type and the angiomatoid type. Of these types, the storiform-pleomorphic type is most common and it accounts for approximately 65% of malignant fibrous histiocytomas [4].
For the cases of malignant fibrous histiocytoma, it has been reported that they show pathologic findings different from the primary tumor, or other histologically very different tumors can occur for about 10% of them [5].
For making the diagnosis, the clinical symptoms, the physical examination findings such as an abdominal mass and abdominal tenderness, and a low density mass seen on the plain abdominal tomography can indicate a suspicious mass, and the retroperitoneal tumors can be also observed by CT, MRI, and ultrasonography [6].
The main treatment is extensive surgical resection and then these tumors are often treated with concurrent chemotherapy and radiation therapy to reduce the possibility of local recurrence and metastasis. It has been reported that the average five-year survival rate of patients with malignant fibrous histiocytoma is 59% to 66.7% and the local recurrence rate is 16% to 31% [7]. The prognostic factors to predict local recurrence and distant metastasis include the patient's age, a history of recurrence, the tumor size and depth of invasion, the histological grade of the mass and the status of the resection tumor margin. The histological grade of the emass and the status of the resected tumor margin are the most reliable predictors of the prognosis [8].
However, it is often impossible to conduct the extensive resection without damaging the capsule of the mass when soft tissue sarcoma such as malignant fibrous histiocytoma occurs in the retroperitoneal cavity. For the mass of this report, we thought that the mass was radically resected (< 2 cm distance from the tumor) with a negative marginal status when the primary surgical resection of the tumor was conducted, but we think the recurrence occurred due to microscopic residual tumor and the local recurrence occurred at a more rapid rate because postoperative concurrent treatment was not conducted. Thus, we can say that it is of great importance to conduct the concurrent treatment with postoperative chemotherapy and radiation therapy when malignant fibrous histiocytoma with a higher recurrence rate occurs in the retroperitoneal cavity rather than in the limbs. The effect of these treatments are still controversial, but Feldman and Norman [9] reported that irradiation reduced the size of the mass, and Simon and Enneking [10] reported that one patient among the cases of lung metastasis of malignant soft tissue tumor completely recovered from multiple pulmonary nodules in both lungs after radiation and dactinomycin therapy.
For our current case, considering that the age of the patient was the late 60s and the size of the tumor was larger than 5 cm with iliac involvement and the histological grade was also high, we can predict that there is a great possibility of local recurrence or distant metastasis into the lung in the future. In addition, when malignant fibrous histiocytoma occurs in the retroperitoneal cavity, despite the fact that it was successfully treated with surgical resection, the histological grade is high and this type of tumor has a high likelihood of local recurrence in the case with poor prognostic factors for local recurrence. Therefore, we think that concurrent treatment with chemotherapy and radiation therapy after surgery should be conducted and periodic follow up observation should be performed for the early detection of local recurrence and metastasis after surgery. Because the tumor's growth increased over time, we can verify the need for surgical excision as soon as possible when the recurrence occurs.
We performed surgical treatment for a recurrent malignant fibrous histiocytoma that occurred in the left psoas muscle, and we report the MRI findings and the prognostic factors for local recurrence and distant metastasis, along with a review of the relevant literature.