Clinical Findings and Results of Surgical Resection of Thoracolumbar Osteoid Osteoma
Article information
Abstract
Study Design
Descriptive, cases series study.
Purpose
To evaluate clinical findings and results of treatment of patients with spinal osteoid osteoma who underwent surgery.
Overview of Literature
Osteoid osteoma is a benign tumor with spinal involvement rate of about 10%. It is manifested during adolescence with symptoms such as painful scoliosis. To treat the problem, operation on the patients and excising the nidus are suggested.
Methods
This descriptive study was conducted on 11 patients with spinal osteoid osteoma at our orthopedic educational center. All patients were treated through open surgery and nidus curettage. All samples were pathologically confirmed. Imaging methods (spiral computed tomography-scan) was used in preoperative planning. Scoliosis and other clinical findings were studied.
Results
The study was conducted on 11 patients comprising 6 females (54.5%) and 5 males (45.5%) with the mean age of 14.6 years. Mean deviation of scoliosis resulting from spinal osteoid osteoma was 22.8 degrees. There was more scoliosis in the involvement of the lumbar vertebra. In comparison with adults, scoliosis was more severe in youths. There was one case of vertebra body involvement with manifestation of painful scoliosis. Due to lack of careful preoperative examination, the surgery was repeated for this case. No sign of recurrence was observed in patients who underwent open surgery and all scoliosis in the follow-up had improved.
Conclusions
Based on our findings, surgical excision of spinal ostoeid osteoma was successful and complete recovery was achieved in spinal deformity in the course of follow-up. Scoliosis is often seen during adolescence and lumbar involvement is more severe.
Introduction
Osteoid osteoma is a less frequent benign tumor initially described by Jaffe [1] in 1935. Osteoid osteoma is often seen within the first thirty years of life and its classic complications include local pain, more pain resulting from activity, night pain, and aspirin-responding pain [2]. Early diagnosis is important, since the possibility of spinal tumor should always be taken into consideration even if the incidence is low and prevention of developed complications is induced [3]. Radiography is often used to detect the disease [2]. However, bone scan and computed tomography (CT)-scan are required to exactly determine the lesion locus. The tumor is treated through excision surgery of the nidus [2].
Spinal involvement is seen in about 10% of the cases of osteoid osteoma. Scoliosis resulting from spinal osteoid osteoma is manifested in 70% of cases as a painful scoliosis in adolescents [4]. Secondary scoliosis may be attributed to para-spinal muscles spasm and inflammatory variations in lesion-surrounding tissues. Spinal involvement is often seen at the posterior component [5,6,7]. In general, the posterior spine is involved with osteoblastomas or osteoid osteoma [6]. An osteoblastoma is a vascular, osteoid, bone-forming lesion located mostly in the long bones and posterior elements of the spine. It is noted in the differential diagnosis according to symptoms and morphology with osteoid osteoma [6].
The aim of the present study is to review unusual spinal osteoid osteomas treated at the spinal column ward of our training center within the last five years (2007-2012). The study describes clinical and radiological findings and therapeutic results of patients with thoracolumbar osteoid osteoma.
Materials and Methods
This retrospective study was conducted on 11 patients with unusual osteoid osteoma who were referred to the spinal cord surgery ward of the Shohada Orthopedic Center of the Tabriz University of Medical Sciences. All patients were evaluated by considering the patients' conditions, how the disease was started, type of pain and natural pain independent to physical activity, pain response to nonsteroidal anti-inflammatory drugs especially to ibuprofen, patients' primary complaint, diagnostic methods, treatment methods, and results of long-term follow-up.
All patients were clinically examined and the findings were recorded. Radiological films (plain X-ray films) were prepared for all patients. CT-scan was used to exactly determine the lesion locus and unusual cases. A bone scan was conducted in uncertain cases. All required documents were available for each patient. All patients underwent open spinal surgery and the nidus was surgically excised. The histopathological examination of all samples confirmed osteoid osteoma (Fig. 1). The tumors consisted of thick, irregular shape trubeculae of woven bone, and numerous osteoblast-like cells that fill the intertrabecular spaces. The patients were followed up for about two years. The present study was supervised and confirmed by the ethics committee of Tabriz University of Medical Sciences.
Results
The study was conducted on 11 patients suffering from spinal osteoid osteoma. The subjects consisted of 6 females (54.5%) and 5 males (45.5%) with the mean age of 14.6 years. The findings are separately presented in Table 1. Spinal deviation (scoliosis) seen in about 7 cases (63.6%) was regarded as the most important complaint of the patients. In 5 patients (45.5%), the scoliosis was not painful or typical and the patients had been referred to a physician due to their postural disorder. The mean duration of the disease symptoms was 15 months. Primary pain and painful scoliosis were seen in two cases (18.1%). Involvement of spinal posterior component was observed in 10 patients (90%), resulting in spinal deviation (Fig. 2). Vertebral body involvement occurred in only 1 patient, an 8-year-old boy with scoliosis, resulting from a tumor in the body of the T12 vertebra (Fig. 3). Misdiagnosis before careful detection of osteoid osteoma was seen in 6 patients (54.5%). The patients received medical or brace treatments and were referred to our center because they had not recovered. During the initial stages, the physicians were successful in accurate detection of the disease in only two cases considering the description of conditions and radiography. In addition to axial cuts, a spiral CT-scan at the sagital view was required to provide better visibility of the nidus in patients with posterior cortex involvement where the pedicels were jointed. Primary surgery to excise was unsuccessful in one case of vertebral body involvement in an 8-year-old boy. In the second surgery conducted on the T12 vertebra, the lesion was completely excised. The problem resulted from a lack of primary exact examination and the surgery was carried out relying only on axial cuts. It was not possible to find the lesion during surgery. The CT-scan was repeated, sagital cuts of the second surgery were successfully evaluated, and the tumoral lesion was excised.
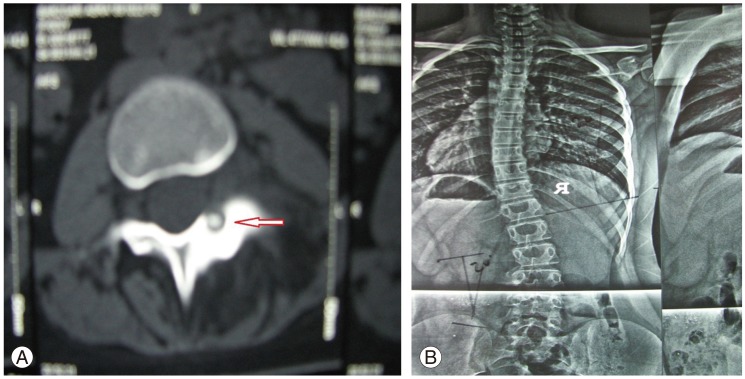
(A) Involvement of posterior part (arrow) of vertebra. (B) Twenty degrees scoliosis deviation in thoracolumbar spine.
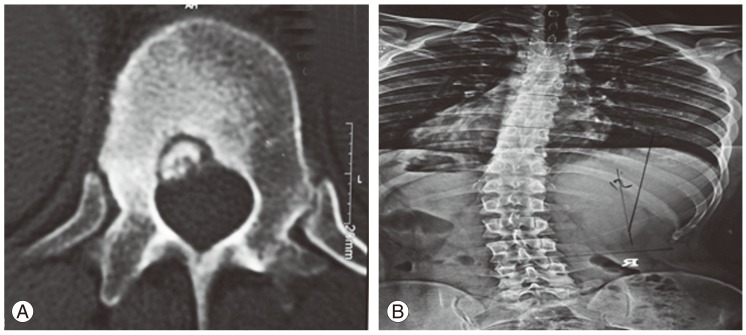
(A) Involvement of body of T12 vertebra with painful scoliosis in an 8-year-old boy. (B) Twenty-one degrees spinal deviation due to T12 osteoid osteoma.
Preoperative pain duration was reported to be 6 months in four patients describing their conditions. Neural manifestations and iatrogenic neural damage resulting from surgery were not seen in any patient.
Mean deviation of scoliosis resulting from spinal osteoid osteoma was 22.8 degrees. Scoliosis resulting from spinal osteoid osteoma was observed to be more pronounced in lumbar vertebra involvement and was more severe in youths than in adults. The highest rate of deviation (30°) was seen in a 15-year-old girl suffering from backache (Fig. 4). On follow-up, it was revealed that the patients' symptoms had completely disappeared and spinal deviation was recovered (Fig. 5). Spinal deviation was seen in tumor lesions of thoracic vertebra.
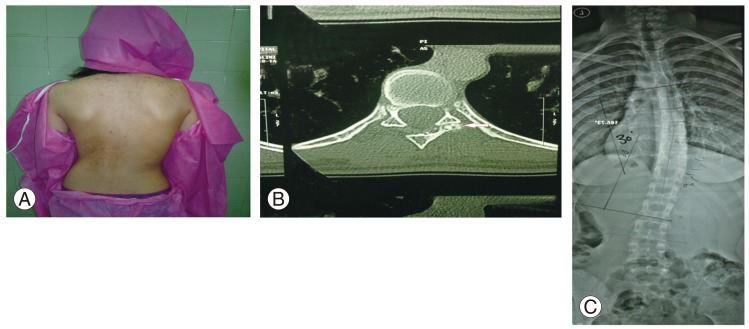
(A) Clinical photo of spinal deformity. (B) Axial computed tomography of vertebra indicating posterior lesion. (C) Radiography showed 30° scoliosis in a 15-year-old girl.
Discussion
Adolescence is regarded as the peak age for osteoid osteoma and spinal involvement has been reported as 10% to 20% in various studies [8,9]. Backache, which depends on the nidus locus, was the patients' most serious complaint. However, it seems important that backache is not common during adolescence and youth. When it occurs, it relates to muscular spasm and spinal deviation resulting in clinical suspicion of osteoid osteoma [8,9]. Considering the small size of the lesion and the complex spinal anatomy, spinal radiography is not helpful in detecting the tumor and may even result in misdiagnosis of the tumor in some cases, unless every patient with recent scoliosis undergoes further imaging examinations, especially when backache is added to the scoliosis panel with a small angle [9,10].
The incidence rate of osteoid osteoma-related scoliosis varies from 20% to 70% in various studies. Asymmetrical lesions in thoracic and lumbar vertebra increase scoliosis progress risk [11,12,13,14]. Muscular spasm and inflammatory responses are the most important factors leading to spinal deformity. In a study conducted by Assoun et al. [2], intensive inflammatory variations around lesions were observed in about 63% of cases. Aydinli et al. [15] studied 8 patients with spinal osteoid osteoma and noted that painful scoliosis was seen in 5 cases (62.5%). In similar findings in our study, scoliosis was indicated in 63% of the patients. However, 45% of the patients did not feel pain or the pain was not sufficiently severe to seek treatment. The disease was incorrectly detected by the physicians and the patients received inappropriate treatments due to underestimation of ambiguous lumbar pain with mild scoliosis. Similar to other studies, osteoid osteoma had occurred during adolescence. One of the factors involved in misdetection was the greater number of female patients compared to male. According to Sapkas et al. [16], painful adult scoliosis was treated with a brace for a long period of time and non-recovery and progress of scoliosis angle to 25° were detected after 5 years.
CT-guided percutaneus radiofrequency ablation as a minimally invasive treatment for osteoid osteoma is an acceptable method [13]. Lindner et al. [13] demonstrated that treatment with CT-guided radiofrequency ablation was successful and safe without recurrence in 58 patients with osteoid osteoma in extremities. The procedure may not be indicated for lesions of spine or small bone (hand and foot) due to thermal necrosis.
In most patients, spinal osteoid osteoma is completely treated by surgery and the lesion curettage results in disappearance of the symptoms. Therefore, lesion curettage is regarded as a definite and appropriate treatment for these patients [4,15]. At the spinal area, excision of the lesion is associated with a number of difficulties and neurological damage risk due to neural adjacency and anatomical complexity. In unusual cases, accurate preoperative planning and use of CT-scan imaging methods with three-dimensional reformation, is therefore of special importance [4,15]. In our study an 8-year-old boy presented with 21° scoliosis and it was not possible to completely excise the nidus since the osteoid osteoma was located at the body of the T12 vertebra. Thus, a second surgery was required, the need for which may be attributed to the lack of exact preoperative examination and imaging evaluations to determine the exact locus of the lesion. Vertebral CT-scan at sagital and coronal cuts made it possible to exactly determine and approach the lesion. According to Cristante et al. [17], osteoid osteoma was observed in the body of the L5 vertebra of a 44-year-old woman. The problem manifested with night pain and was treated using a minimal invasive radiofrequency method. In Cristante et al. [17]'s report, no spinal deviation was recorded. Considering the infrequency of spinal involvement, most studies were conducted as case reports and no study has evaluated the relationship between osteoid osteoma at different parts of the spinal column and the type and size of the resulting deformities. It seems that scoliosis resulting from osteoid osteoma often occurs during adolescence. According to our report, it is not limited to the posterior parts of vertebra and may lead to scoliosis at the vertebra body. Additionally, our observations suggested that spinal osteoid osteoma of the lumbar area is associated with more deformity and severe scoliosis. While this may be related to the patients' age (adolescence), we were not able to determine reasons for this. The sample size is too small for a reliable conclusion and further studies are required in this regard. Also, the most important symptoms of the disease may be manifested as spinal deviation during adolescence without any predominant pain. This is regarded as one of the important factors in misdetection.
Conclusions
Based on our findings, surgical excision of spinal ostoeid osteoma was successful and complete recovery of spinal deformity was achieved in the course of follow-up. Scoliosis is often seen during adolescence and lumbar involvement is more severe.
Notes
No potential conflict of interest relevant to this article was reported.


