Introduction
Cervical radiculopathy is one of the most frequently occurring and treated cervical spinal conditions. Radiculopathy is a disorder of the cervical nerve root, manifesting usually as a combination of neck and upper limb pain, sensory deficit or motor disturbance [1].
Anterior cervical discectomy and fusion (ACDF) is the gold standard for the surgical treatment of cervical disease, with multiple ways of performing the procedure reported in the literature since its original description by Smith and Robinson [234567]. ACDF using stand-alone cages packed with local autograft has been used with favorable results [89]. Over the last 10 years, the practice at our institute is to use stand-alone cages of trabecular metal (TM-S, Zimmer, Minneapolis, MN, USA) without an autograft. To our knowledge, there are no medium- to long-term outcome results of cervical trabecular metal cages without autograft reported in the literature.
The purpose of this study was to evaluate the clinical and radiological outcomes of our 10-year experience of ACDF using stand-alone trabecular metal cages in the treatment of cervical radiculopathy
Materials and Methods
Between July 2002 to July 2012, 90 consecutive patients between the ages of 36 and 64 years at surgery (mean, 44 years) who had been diagnosed with cervical radiculopathy and/or axial neck pain with sclerodermal distribution who underwent single or 2-level ACDF with trabecular metal cages and followed-up for a minimum of 3 years were included. Patients with a history of spine infection or tumor, cervical spine fractures, traumatic spinal cord injury, cervical myelopathy, or prior cervical spine surgery were excluded.
Two fellowship-trained spine surgeons performed the operations, with operation levels limited to the lower part of the cervical spine (C4–7). Two independent senior spine surgeons reviewed the patients and outcomes. We identified and included 90 consecutive patients who met all the inclusion and exclusion criteria with at least 3 years follow-up.
Clinical assessments of axial neck pain, radicular arm pain, upper extremity weakness, and upper extremity altered sensation were performed. As well visual analog scale (VAS) scores were determined preoperatively and postoperatively at 3 months, 1 year, 3 years, and at the latest postoperative follow-up. Radiological assessments were carried out at the same time periods. Axial neck pain and radicular arm pain were subjectively rated as improved or unchanged, upper extremity weakness and motor strength were objectively rated as normal or abnormal. Likewise, upper extremity sensory function was graded as altered to light touch, or normal. An incidence of new deficits was recorded for both motor and sensory function based on newly identified neurologic events.
Results
The mean patient age was 44 years (range, 37–62 years) with a mean follow-up of 4.5 years (range, 2–7 years). Fifty one patients underwent 2-level ACDF and 39 patients underwent 1-level ACDF. Mean operating time was 43 minutes per level (range, 35–50 minutes), and average blood loss was 120 mL per procedure (range, 83–180 mL).
There were improvements in axial neck pain of 80% at the 1-year follow-up and 75% at the 3-year follow-up, and in radicular arm pain with 95% at the 1-year follow-up, and 85% at the 3-year follow-up. VAS scores improved from a preoperative mean of 3 to a mean of 9 at 1 year and a mean of 8 at 3 years postoperatively.
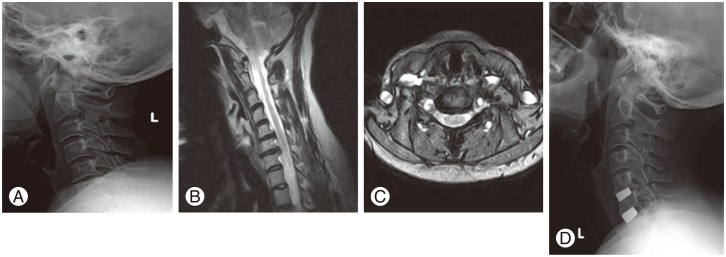
Preoperatively, 70% of patients had sensory deficit and 50% of patients had motor deficit. There was an improvement in preoperative sensory deficit at the 1-year follow-up (90%) and at final follow-up (90%). There was also an improvement in the preoperative motor weakness at the 1-year follow-up (95%) and 3-year follow-up (85%). Fifteen percent of the patients had a motor deficit at the latest follow-up, had undergone a 2-level ACDF, and had radiographic evidence of pseudoarthrosis (Fig. 1). This incidence was lower than the reported rates for anterior plating [10]. No cage extrusion or migration occurred. Subsidence occurred in 8% of levels fused with no correlation found with clinical outcomes.
Fusion was assessed using lateral radiographs and magnetic resonance imaging (MRI) scans looking for bone breaching and radiolucent lines around the device, as well as with dynamic radiographs to assess any translational movement of the device. In our series, 90% of patients did not exhibit any evidence of bone breaching or radiolucency around the device, with translational movement of less than 2 mm on dynamic radiographs at the 1-year follow-up in all patients. Furthermore, MRI scans confirmed restoration of cervical lordosis, with maintenance over the follow-up period (Fig. 2).
There was no persistent dysphagia, voice complaints, dural tear, tracheal perforations, or oesophageal perforations. One patient developed a deep methicillin resistant Staphylococcus aureus (MRSA) infectious infarction of the spinal cord, which was treated with antibiotics. Recovery was complete when reviewed at the 1-year follow-up [11].
Four patients (3.6%) had to undergo further cervical discectomy and fusion surgery planned at the final follow-up. All these patients presented with symptomatic progressive cervical spondylosis, not related to the previously operated segments, and did not respond to conservative measures for at least 6 weeks.
Discussion
Trabecular metal cages (Fig. 3) provide an excellent balance between porosity and strength. They offer a high coefficient of friction to help prevent device migration and extrusion, as well a low modulus of elasticity that may improve load-sharing, which potentially minimizes stress shielding. With their average porosity of 80% and a consistent open pore structure, they are also designed to resemble the structure and mechanical properties of cancellous bone, which provides an excellent environment for boney in-growth and vascularization.
Traditionally, autologous iliac bone graft has been used to fill the disc space during ACDF, with good fusion rates and clinical outcomes. However, autologous bone graft comes with its own set of donor site morbidities including pain, numbness, and infection [21213]. As a result, the use of stand-alone cages has become popular, with many reports describing its effectiveness with good stability, restoration of disc height, and facilitation of bone fusion.
Nonunion and subsidence have been reported as complications of ACDF using stand-alone cages [1415]. Over-distraction, damage of endplate, and osteoporosis are risk factors for subsidence and nonunion [16]. Adequate preparation of both endplates so as not to damage the bony cartilage is an important factor in decreasing subsidence after ACDF with stand-alone cage. In our series, the subsidence rate was 8% of levels fused, and the radiological finding of subsidence did not correlate with a worse clinical outcome, and we found no cage migration or extrusion at the 1- and 3-year follow-up, as an indirect measure of union and fusion.
The main presenting symptom in our series was radiating pain (83%) to either arm, similar to other studies [1718]. Seventeen percent of patients complained of axial neck pain, recurrent headaches, dizziness, and sclerodermal radiation to the shoulder. At the 1- and 3-year follow-up, the improvement of axial neck pain was 80% and 75% respectively, and of radicular arm pain was 95% and 85% of patients respectively. Patients with a preoperative upper extremity weakness and numbness tended to more frequently develop postoperative motor and sensory deficits at the final follow-up period following an ACDF procedure. It is likely that these deficits either represent a recurrence of preoperative deficits or more likely, an overlap of dermatomes and myotomes from an adjacent or remote level supporting the notion of progression of cervical spine degenerative disease, acting as a major contributor to new postoperative sensory and motor deficits [19].
In our series, there was a significant improvement in patient VAS scores at 1 year, with this improvement maintained at 3 years postoperatively. Fifty one patients underwent 2-level ACDF, and 39 patients underwent 1-level ACDF, usually at the C5/C6 (65%), consistent with the results of other studies [1820].
Recently, Mehra et al. [21] found that approaching spinal levels above C4 and exposing more than 3 spinal levels were two factors significantly related to voice and swallowing problems. As all our operative levels were below C4 and we did not expose 3 levels in our patients, we did not have any incidence of persistent dysphagia or voice complaints.
One patient developed a deep MRSA infection after C6/C7 ACDF leading to cord ischemia, with radiological changes and rapidly evolving neurological deterioration. Rapid evaluation with MRI scanning and initiation of antibiotic produced dramatic response with our patient and total recovery at the 1-year follow-up [11].
With ACDF procedures, there are risks of adjacent segments degenerating [22]. This has been observed in approximately 3% of patients in a retrospective long-term follow-up study, with a predicted prevalence at 10 years of approximately 25% [23]. Similar findings were observed in our series at the final follow-up. Recently, a meta-analysis indicated that the mid- to long-term rates of adjacent segment disease and neurological improvements were not significantly different when cervical disc arthroplasty was compared with anterior discectomy and fusion [24]. More importantly, there are no natural history studies yet available to demonstrate a difference between the likelihood of adjacent segment disease developing when ACDF, cervical disc arthroplasty, and non-operated yet symptomatic cervical spondylosis are compared.
The reoperation rate of our series was 3.6%, which is comparable to the rate of the 5-year results published by the Food and Drug Administration ProDisc-C study [25].
Conclusions
To our knowledge, this is the first publication reporting specifically on the mid-term outcomes of ACDF with stand-alone trabecular metal cages as treatment for cervical radiculopathy. Excellent and/or good outcomes were evident in ACDF with acceptable low reoperation rates, and reduced operative times and complications. This appears to be a safe and effective option in treating single and 2-level cervical disc radiculopathy and neck pain.