The Use of T1 Sagittal Angle in Predicting Cervical Disc Degeneration
Article information
Abstract
Study Design
Retrospective evaluation.
Purpose
To analyze the effect of T1 slope on degree of degeneration in patients with cervical disc degeneration.
Overview of Literature
The T1 slope is well known parameter that may be very useful in evaluating sagittal balance. There are no reports on the analysis of the relationship between T1 slope and cervical disc degeneration. We hypothesized that T1 slope has an effect on the degree of cervical degeneration.
Methods
Sixty patients who had cervical spine magnetic resonance imaging (MRI) in our orthopedic clinic were enrolled. Patients were divided into two groups according to T1 slope. Radiologic parameters obtained from radiography and cervical spine MRI were compared between low T1 slope group (≤25) and high T1 slope group (>25).
Results
Among low T1 slope group, average degeneration grade of each cervical segment was 2.65 in C2-3, 2.50 in C3-4, 2.62 in C4-5, 3.23 in C5-6, and 2.81 in C6-7. And that of high T1 group was 2.35 in C2-3, 2.32 in C3-4, 2.59 in C4-5, 2.79 in C5-6, and 2.32 in C6-7. Grade of degeneration of low T1 group was significantly higher, as compared with high T1 group in C5-6 (p=0.028) and C6-7 (p=0.009). Percentage of high grade degeneration of more than grand III was 65.4% in low T1 group and 32.4% in high T1 group (p=0.018). Risk of high grade degeneration of C6-7 was significantly higher in low T1 group (odds ratio, 5.63; 95% confidence interval, 1.665-19.057; p=0.005).
Conclusions
Patients with low T1 slope had higher grade of degeneration regardless of age and gender. Low T1 slope is a potential risk factor of cervical spondylosis especially in the C6-7 cervical segment.
Introduction
Normal lordotic alignment is one of the most important contributing factors to effective motion and function of the cervical spine. Loss of normal lordotic alignment may induce pathologic changes in the kinematics and accelerate degeneration of the functional motion unit [1].
The T1 slope is the sagittal angle between a horizontal line and the superior end plate of T1. The T1 slope is well known parameter that may be very useful in evaluating sagittal balance. Knott et al. [2] reported that patients with T1 tilt of higher than 25° need full column radiography because of the possibility of positive sagittal balance. T1 slope reportedly can be a predictor of kyphotic alignment change after laminoplasty [3]. Cervical spondylosis is an age related degenerative change of cervical segments. Park et al. [4] reported that T1 sagittal slope angle decreased in the older group, as compared with the younger counter part. Many studies have evaluated the factor of cervical disc degeneration [1567891011]. However, there are no studies on the relationship between T1 slope and cervical spondylosis.
We hypothesized that T1 slope can affect the degree of cervical degeneration because of impaired sagittal balance.
Materials and Methods
We enrolled patient of >50 years of age who had cervical spine magnetic resonance imaging (MRI) from January 2013 to December 2014 who visited our orthopedic clinic consecutively. Total 90 patients were enrolled at the beginning of study. Chart reviews indicated that neck pain, shoulder pain, and arm pain were the main symptoms. We excluded patients who taken cervical MRI due to motor vehicle accident or trauma because these traumatic event can cause change of natural cervical lordosis. Thirty patients were excluded and cervical spine MRI of 60 patients were included in the final analysis.
Patients were divided into two groups according to T1 slope. Radiologic parameters obtained from radiography and cervical spine MRI were compared between low T1 slope group (<25) and high T1 slope group (>25).
1. Inclusion criteria
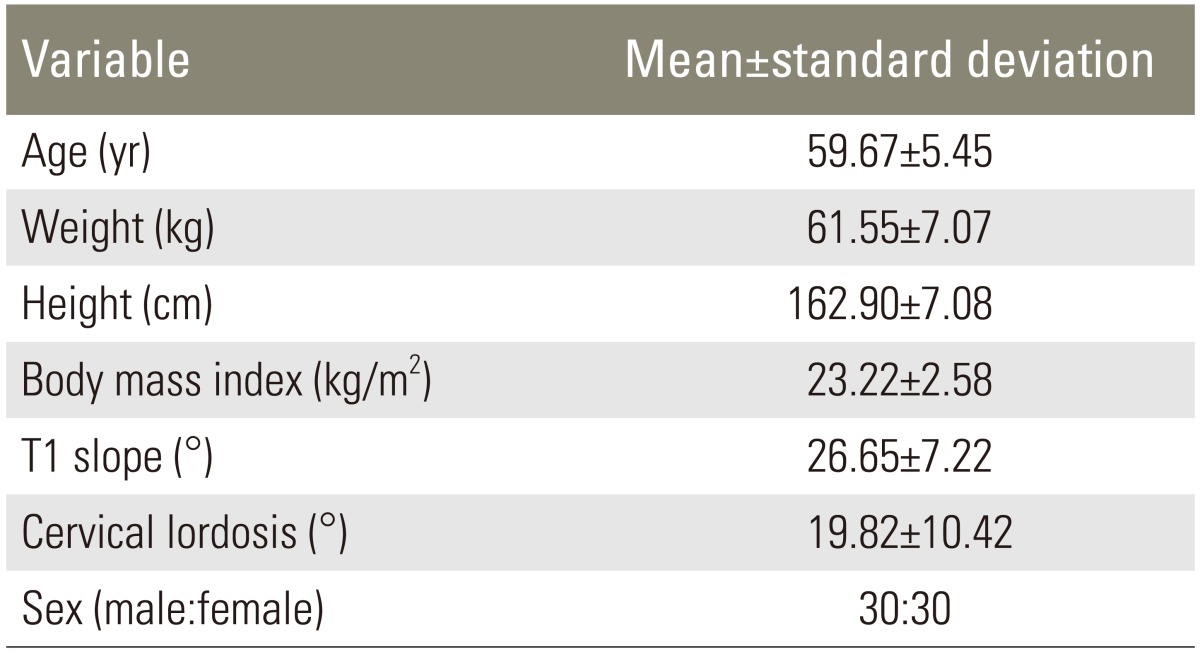
The patients who visited orthopaedic clinic of Gwang-Myeong Sung-Ae Hospital with (1) age above 50 years old, (2) no history of surgery on spine, (3) no recent history of trauma within 3 months, (4) patient with neck pain and radiculopathy of upper extremities, were included. Average age of all patients was 59.67±5.45 years old. Average T1 slope was 26.65°±7.22°and average cervical lordosis was 19.82°±10.42°. Of 60 patients, 30 were male and 30 were female (Table 1).
2. Measures analyzed
Lateral radiograph of the cervical spine was obtained in a standing position with the upper extremities attached naturally at the side of the trunk and their head facing forward for horizontal gaze.
T1 slope was measured as the angle between a horizontal line and superior endplate of T1 in standing lateral radiograph. Cervical lordosis was measured between lower end plate of C2 and inferior end plate of C7 in the same standing lateral radiograph.
Cervical intervertebral disc degeneration was measured based on the magnetic resonance imaging-based grading system [12]. Grading of disc degeneration of the 60 patients was performed by three spinal surgeons (observers) in a blinded fashion using the T2-weighted sagittal images. Five cervical levels (C2-3, C3-4, C4-5, C5-6, and C6-7) were chosen and 300 discs were assessed on T2-weighted mid sagittal images.
This classification takes into account the nucleus signal intensity, the nucleus structure, the distinction between the nucleus pulposus and the annulus fibrosus, and the disc height from grade I to V. High grade degeneration was defined as a grade higher than grade III in which case the disc height is decreased.
3. Statistical analysis
Grade of disc degeneration were compared between low T1 group and high T1 group using t-test and chi-square test. And risk of high grade degeneration was analyzed using binary logistic regression test controlling age and gender. Statistically significant difference was considered when p-value was <0.05.
Results
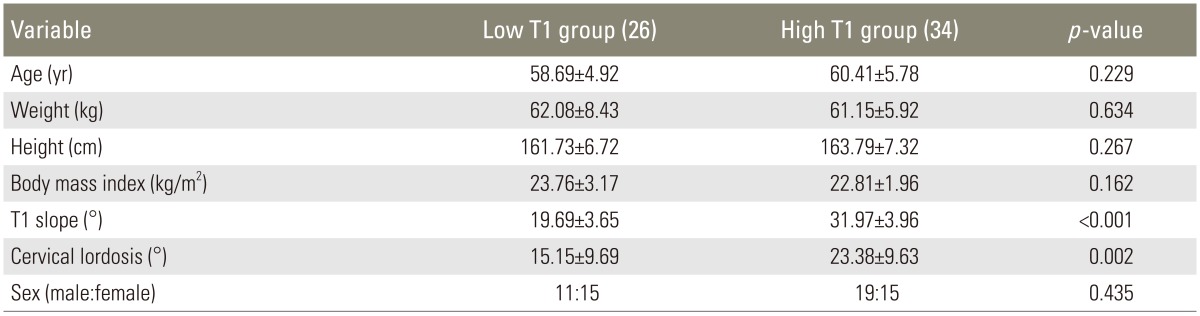
Average age of low T1 group was 58.69±4.92 and that of high T1 group was 60.41±5.78. The difference of age between low T1 group and high T1 group was not statistically significant (p=0.229). Average T1 slope of low T1 group was 19.69±3.65 and that of high T1 group was 31.97±3.96. The difference of T1 slope between both groups was statistically significant (p<0.001). Average cervical lordosis of low T1 group was 15.15±9.69 and that of high T1 group was 23.38±9.63. The cervical lordosis of both group was statistically significant (p=0.002). Among both groups, weight, height and body mass index were not significantly different (Table 2).
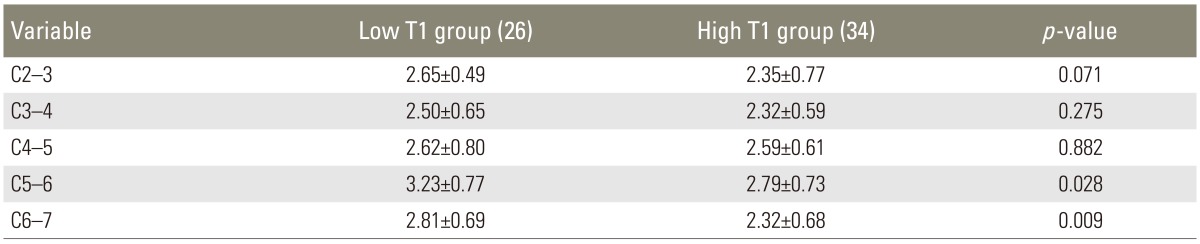
Among low T1 group, average grade of each segment was 2.65 in C2-3, 2.50 in C3-4, 2.62 in C4-5, 3.23 in C5-6, and 2.81 in C6-7; and that of high T1 group was 2.35 in C2-3, 2.32 in C3-4, 2.59 in C4-5, 2.79 in C5-6, and 2.32 in C6-7. Grade of degeneration of low T1 group was significantly higher, as compared with high T1 group in C5-6 (p=0.028) and C6-7 (p=0.009) (Table 3, Figs. 1, 2).
Comparison of radiologic parameter on magnetic resonance imaging between low T1 group and high T1 group using t-test
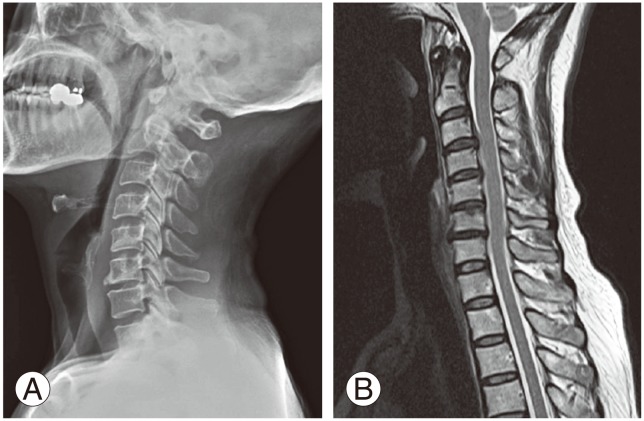
Radiographic example of a 55-year-old female with low T1 slope (A) upright lateral X-ray. (B) T2 sagittal image of cervical magnetic resonance imaging.
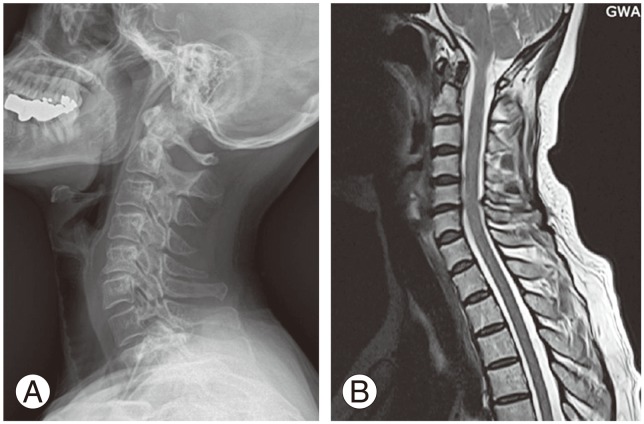
Radiographic example of a 51-year-old female with high T1 slope (A) upright lateral X-ray. (B) T2 sagittal image of cervical magnetic resonance imaging.
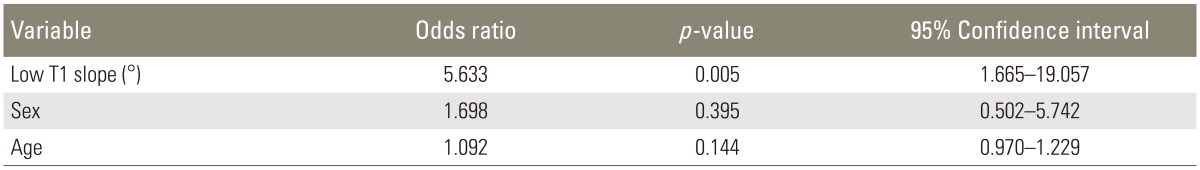
Percentage of high grade degeneration of more than grade III was 65.4% in the low T1 group and 32.4% in high T1 group (p=0.018) (Table 4). Risk of high grade degeneration of C6-7 was significantly higher in the low T1 group (odds ratio, 5.63; 95% confidence interval, 1.665-19.057; p=0.005) (Table 5).
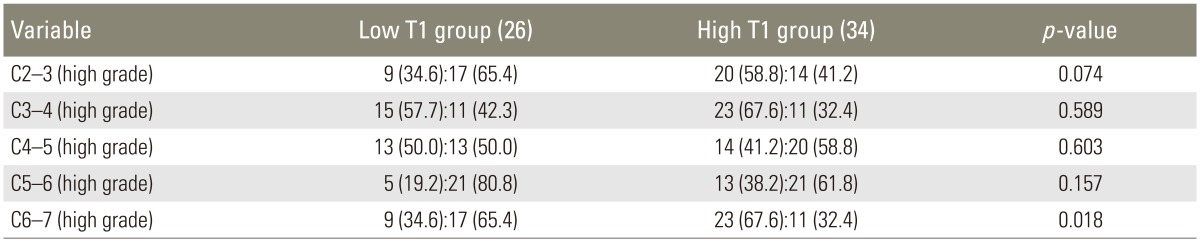
Comparison of radiologic parameter on magnetic resonance imaging between low T1 group and high T1 group using chi-square test
Discussion
Cervical disc space narrowing, osteophytes, and disc degeneration are common and increase with aging [9]. The prevalence of abnormal magnetic resonance images of the cervical spine is related to age in asymptomatic individuals. Clinical cervical aging studies have shown that 14% of asymptomatic subjects younger than 40 years have abnormal MRI scans with an increase to 50% by 50 years old [13]. Therefore, we enrolled patient aged over 50 years old to analyze disc degeneration.
Cervical lordosis in standing posture in 54 healthy volunteers was 54° (range, 36°-76°) [14]. In our study, average cervical lordosis of all patients was 19.82°. Candidates of our study were patients with neck pain and radiculopathy of upper extremities. The average age of patient was 59.67 years. Degenerative change with aging and its underlying pathology may be a contributing factor to decrease in lordosis.
Straightened cervical lordosis causes stress concentration, so cervical lordosis may have a direct impact on cervical spondylosis [15]. In our study, the low T1 group had significantly lower cervical lordosis, as compared with the high T1 group. Decreased cervical lordosis in the low T1 group may cause stress concentration on the C5-6 and C6-7 segments. This stress concentration may result in a higher degree of degeneration of these segments.
The changes in sagittal alignment of the cervical spine affects the kinematics. Consequently, it may cause changes in the segment subjected to maximum load for overall motion and accelerate its degeneration [1]. The increased strain energy density and stress in the vertebral cortex over time may induce the remodeling process according to Wolff's law, leading to the formation of osteophytes [10]. Knott et al. [2] reported that patients with high T1 slope of more than 25° can have positive sagittal balance because of the increased sacral vertical axis.
We did not evaluate whole sagittal balance of body because this study was performed retrospectively. However, high T1 slope does not contribute to a high grade of degeneration of the cervical disc. Cervical degeneration and spondylotic change may be caused by stress concentration with decreased cervical lordosis rather than impaired sagittal balance.
The limitation of our study is that the sagittal balance of patients was not evaluated because the study was performed retrospectively. Degree of disc degeneration of both groups was significantly different but we could not conclude that the sagittal balance has an effect on cervical disc degeneration. Further study is required on the relationship between sagittal balance and cervical disc degeneration.
Conclusions
Patients with low T1 slope had less cervical lordosis than patients with high T1 slope. In addition, there was a higher grade of degeneration regardless of age and gender. Low T1 slope is a potential risk factor of cervical spondylosis especially in the C6-7 cervical segment.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.