Introduction
Adult spinal deformity surgery is associated with high rates of mechanical complications, such as proximal junctional kyphosis and nonunion [1]. Nonunion at the lumbosacral junction is a classic complication of long construct, with the reported incidence of nonunion ranging from 5% to 44% when using S1 promontory screws (classical S1 screws) [2-4]. The risk of nonunion increases with fusions extending to L3 and above [5]. Therefore, experts have recommended anterior interbody support or iliac fixation to decrease the risk of nonunion [6,7]. Furthermore, addition of anterior support without pelvic fixation does not decrease the stress on the S1 screws [5]. Classical iliac fixation has been extensively studied and has demonstrated superior biomechanical proprieties and lower pseudarthrosis rates than those of the Galveston technique or sacral plate technique [4]; however, its drawbacks include separate skin incision, use of connectors, and development of implant prominence requiring screw removal (range, 22%ŌĆō34%) [4,5,8]. The use of S2 alar iliac (S2AI) screws in pediatric patients has been popularized by Paul D. Sponseller and in adult patients by Khaled M. Kebaish [9]. S2AI screws address the drawbacks of classical iliac screws while demonstrating similar biomechanical advantages [9].
To the best of our knowledge, there is no description of iliac fixation emerging from the first sacral pedicle. The S1 alar iliac (S1AI) screw has the advantage of achieving pelvic fixation without dissection to the S2 pedicle entry and may be a viable option for the salvage of a failed S1 promontory screw. The main aim of this paper was to describe the S1AI screw fixation technique and report our experience with the first few cases.
Technical Note
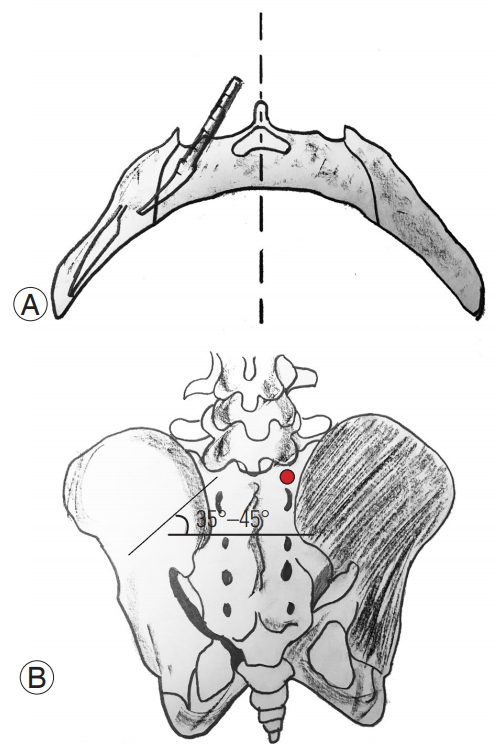
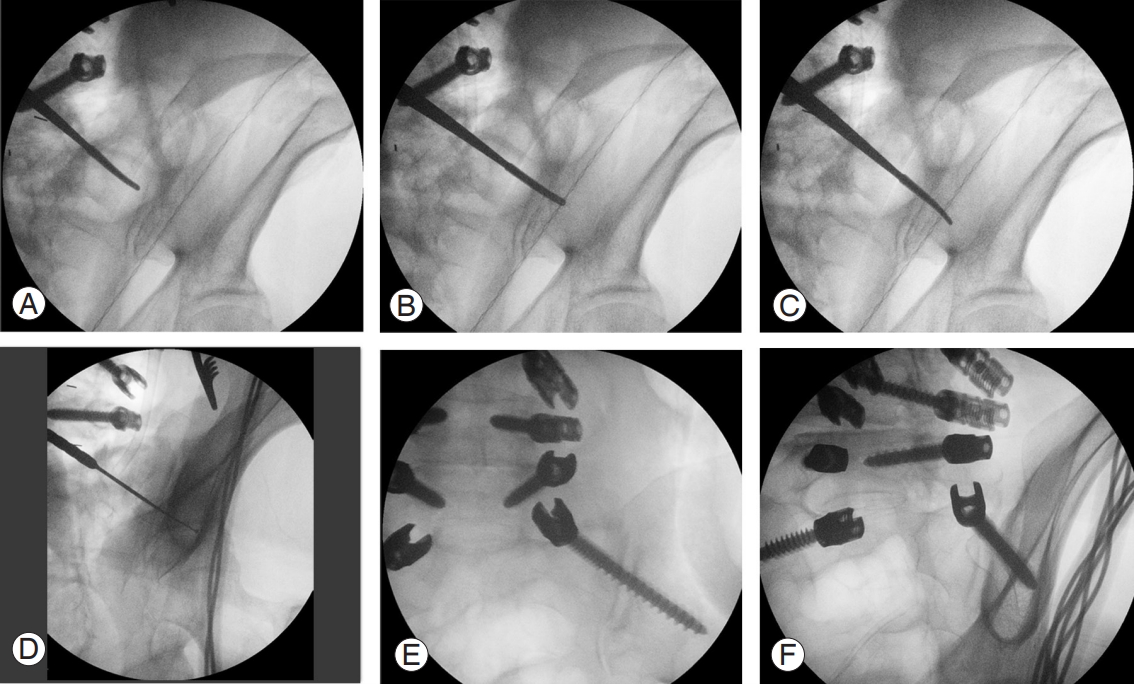
S1AI screw fixation is performed using anatomical landmarks and under fluoroscopic guidance. The entry point is located at the entry of the S1 pedicle at the foot of the superior S1 facet in the middle (Fig. 1). The entry point should not be located very laterally (to have sufficient purchase in the sacrum) or medially (to be in line with the L5 screws). A 2-mm burr is used to create a posterior breach for the entry point. The gear shift is pointed backward to avoid anterior sacral breach. The gear point is angled 35┬░ŌĆō45┬░ caudally and 20┬░ horizontally in the coronal plane. The position is checked using anteroposterior (AP) fluoroscopy such that the screw should aim at the ipsilateral greater trochanter (Fig. 2). The pedicle finder is advanced 3ŌĆō5 cm until it hits the lateral sacral cortex at the sacroiliac joint. The sacroiliac joint is penetrated by carful advancement of the pedicle finder, either manually or using a mallet hammer, after determining the correct position using AP fluoroscopy. The curved probe is turned 180┬░ to face anteriorly. The use of a long probe with a straight handle to maintain the 20┬░ horizontal coronal angle and minimize the interference of surrounding tissues is preferred. Oblique fluoroscopy with tear drop view is used to verify the intrapelvic trajectory of the tip of the gear shift after advancing 5 mm into the iliac bone until the desired depth is achieved (normally Ōēź75 mm). Next, a ball-tipped sounding device is used to palpate all bony borders, after which tapping and screw insertion is performed in the classical manner.
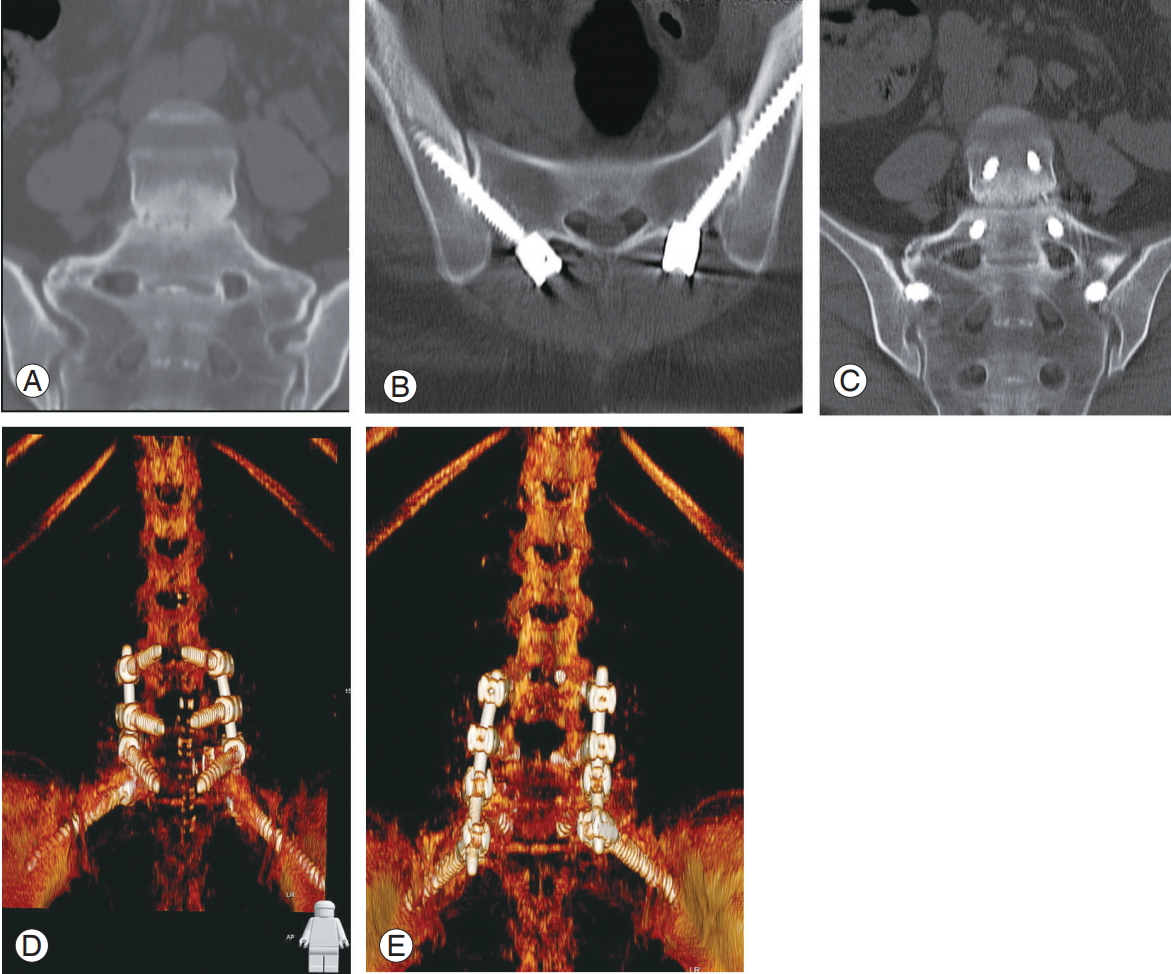
Between June 2017 and September 2017, seven patients were operated using S1AI screw fixation. The use of S1AI screw fixation was indicated by sacralization of L5 with high grade isthmic spondylolisthesis in one patient, severe S1 body osteoporosis with a history of anterior surgery on the sacral plateau in one, spinal metastasis to the L5 body requiring L5 corpectomy and pelvic fixation in two, pelvic fixation for L2ŌĆōS1 construct in two, and nonunion at the lumbosacral junction in one. Postoperative pelvic computed tomography and evaluation of the screw trajectory and ilium size were performed.
A total of 14 S1AI screws were placed and evaluated using postoperative imaging. The mean length and diameter of the S1AI screws were 78 mm and 8 mm, respectively. There were three posterior cortical breaches of the iliac bone that were observed in the first two cases in which we used a straight gear probe. The average length of the screw inside the iliac bone was 37.3 mm. There were no patients with neurological or vascular complications associated with the use of these screws. No patients presented postoperative sacroiliac pain during the short follow-up period.
Discussion
Even with the advancement of spinal instrumentation, the incidence of mechanical complications is up to 44%. Therefore, distal fixation for long posterior spinal fixation is crucial [2]. Kim et al. [10] found that the L5ŌĆōS1 space is the most common site for nonunion during scoliosis surgery, with an incidence of 24%. The use of pelvic fixation as an adjunct for sacral fixation decreased the incidence of mechanical complications at the sacroiliac junction to <5% [8]. Nonetheless, iliac screws are associated with extensive tissue dissection, connector use, and implant prominence development [3,8]. S2AI screw fixation has been described as an alternative to iliac fixation, with the biomechanical advantage of cortical fixation (both sides of the sacroiliac joint) as well as cancellous purchase in the narrow space between the two cortices of the iliac wing. We described, for the first time, S1 alar iliac direction for sacropelvic fixation. This fixation technique could be used in patients with abnormal transition at the lumbosacral area (sacralization of L5) (Fig. 3). In our opinion, the most important indication for using S1AI screw fixation was to salvage S1 screw failure (loose classical S1 screw, destruction of the anterior sacral body by a tumor, etc.). Generally, osteopenia at S1 limits the quality of fixation at the S1 promontory screw.
The advantages of the newly described S1AI screw fixation are numerous. It is in line with other screws and does not require connectors. There is less need for extensive dissection of the sacral ala because the entry point is more medial than that in classical sacral screw fixation, thereby reducing bleeding and operative time. In addition, this type of trajectory offers the advantages of pelvic fixation. Moreover, as shown by Sutterlin et al. [5], the use of pelvic fixation as an adjunct to a long construct is superior to using an anterior support alone.
The incidence of posterior breach was 21%, and a straight probe was used in all such cases. In case of S2AI screws, this breach frequently ranged between 10% and 22% [2]. Several studies have shown that the ŌĆ£four wall corticalŌĆØ purchase was superior to the ŌĆ£three wall corticalŌĆØ purchase with S2AI screws [11]. Nonetheless, the use of quad cortical purchase has been debated and lacks supportive evidence [2]. Albeit this controversy, the posterior breach was not associated with increased vascular or neurological complications.
Several studies have shown that sacroiliac pain is one of the leading causes of failed back surgery syndrome, with an estimated incidence of 22%ŌĆō40% [12]. One notable concern was that the S1AI screw crossed the sacroiliac joint. In fact, OŌĆÖBrien et al. [3] found that the S2AI screw crossed the SI joint cartilage in 60% of cases in a cadaveric study. The long-term effects of this breach are not fully known, and longer follow-ups of patients with S2AI screw fixation may elucidate this issue. Nonetheless, the incidence of SI joint pain seems to be relatively low with the use of S2AI screws [2]. This could be caused by the fixation of the SI joint by the traversing screw [13].
This technical note reported the first few experiences of the use of S1AI screws. There were several limitations in this study. First, there was no long term follow-up to evaluate the screw performance. Second, there are no biomechanical studies that proved the superiority of this screw type over S1 promontory screws. To overcome the second limitation, an ongoing biomechanical study has been designed.
In conclusion, the use of S1AI screw fixation is a viable option that may serve as a foundation for long constructs. Its main advantage is its suitability for revision surgery for failed lumbo-sacro-pelvic fixation. It can also be used in patients with weak S1 promontory fixation, especially in those with osteoporosis. However, further biomechanical testing and longer follow-ups are needed.