Introduction
There are numerous previously published papers on the spinal tuberculosis, mostly from the tuberculosis prevalent countries such as India, Northern-Africa, Hong Kong, and Korea in the past [1-14]. Good quality and informative papers are still being published from India [9,10,14,15]. However, in the previous papers pediatric spinal tuberculosis were dealt less in comparison with the adult spinal tuberculosis, and those authors rarely focused to observe the effect of the disc of the lesion on the affected vertebral growth and kyphotic changes [2,5,11-14,16].
During the past 60 years there was remarkable evolution in the management of spinal tuberculosis, particularly the surgical management of the disease-related spinal deformity, its prevention and correction. British Medical Research Council (MRC) spinal tuberculosis study group provided the standardized therapeutic protocol after the field survey in Hong Kong, Korea, and Africa [11]. However, recently the MRC-provided protocol is not well accepted as the standardized regimen. Because the MRC therapeutic protocol declined more toward the conservative ambulatory chemotherapy than the surgical regimen. Those opponent surgeons were the members of the aggressive surgical school, and they paid attention more on the spinal column cosmesis in the cases of the spinal tuberculosis of the adulthood [12,14,15].
Children are not the miniature of the adults, and they are anatomically and physiologically different from the adult in many aspect. A child has a growth potential in the growth plate, and high modeling capacity. Therefore, the kyphosis management of the pediatric spinal tuberculosis must be different from the adult. Up to now only a few conducted the surgery for the malaligned spinal column of in the pediatric spinal tuberculosis, based on the severity of the disease by ignoring the end-plate and the ring apophysis [1,12].
Rajasekaran [9,10] reported the very informative natural course of the pediatric spinal tuberculosis in the late 1980. They did not mention and discussed in detail the role of the growth cartilage on the spinal column growth, and also did not provide most desirable time in assessing the residual kyphosis.
Based on the above-mentioned information, the current authors designed this retrospective study, utilizing all the previously collected medical records, X-ray and magnetic resonance imaging (MRI) data by them. The aim of this study was to elucidate the most reliable predicting time for residual kyphosis in the medically treated children.
Materials and Methods
One hundred and one children with various stages of tuberculous disease processes, aged from 2 to 15 years, were subjected to this study. They were treated at one of those hospitals listed below: eight Catholic University affiliated hospitals, Dong-Shin General Hospital, Sun General Hospital, and Cheju Halla General Hospital during the period of 1971 to 2010, and were treated only with the combined anti-tuberculous chemotherapeutics. Surgically treated children were excluded. All children were followed for 36 months at minimum and 20 years at maximum.
Forty children (39.6%) had the lesion in cervical and cervicodorsal junction, 30 children (29.7%) in the dorsal, and 31 children (30.7%) in the lumbar and lumbosacral spine. Twenty-six children (25.7%) were under age of 5 years, 43 children (42.5%) in age range from 6 to 10 years, and 32 children (31.6%) over 10 years of age. Eighteen children (17.8%) were partially paralytic; three in Frankel B, 12 in Frankel C, and five in Frankel D.
This study was approved by the Institutional Review Board of Cheju Halla General Hospital (IRB approval no., CMC-MKIOR: 26). Informed consents were obtained from patients.
1. Diagnostic methods
Clinical diagnosis was made on basis of the patients disease history and complaints and the physical findings at the time of initial examination which was augmented later by laboratory and image data, and was reconfirmed by the physical response against chemotherapeutics. For image diagnosis, simple radiograms and MRI were used. MRI demonstrated more accurately the disc sparing. Thus, great emphasis was placed on the assessment of disc conditions including growth cartilage which was closely related with the re-growth and modeling of the bony vertebra. This issue was the key point of this study.
2. Assessment of the disease arrest and healing, and stability of the diseased segment(s)
Images were the keys in the assessment of disease states which were augmented by the clinical symptom improvement and laboratory data. Disease arrest point is the progress stop time in which no further bony vertebral damage occurs on images in conjunction with the normalized laboratory data. Disease heal (cure) point is defined when the image and laboratory data of the arrest point are maintained and additional radiographic findings such as bony reformation, modeling, and intercorporal fusion are seen. Diseased segment stability is defined when the same image findings of the arrest point is seen irrespective of corporal fusion.
3. Assessment of disc condition at the site of tuberculosis and spontaneous intercorporal fusion of the diseased segment(s)
Disc space on image becomes narrowed when any part of its component structure is destroyed. Therefore, assessment of disc space on simple radiographs and MRI is important, and more important one is the assessment of the end-plate condition whether it is irregular, and disrupted, and disappeared. Because the vertebral growth and modeling of shape are depend on the growth cartilage. In the case of complete disc disappearance including growth plate, bony vertebral re-growth, and modeling cannot be anticipated, while the re-growth is possible when the growth end-plate cartilage is preserved in spite of some disc space narrowing. Intercoporal fusion can be assessed early by image study.
4. Assessment of changes of kyphotic deformity
The change of kyphosis is measured by Cobb method, utilizing the simple radiograms at the initiation time of chemotherapy, arrest, and cure points, and thereafter the kyphotic change was measured with certain interval in the cases of the decreased and increased kyphosis. Effect of the spontaneously fused bloc vertebrae on kyphosis progress also assessed.
5. Assessment of stability of the diseased segment at the time point of arrest and cure
When the rapid progress of kyphosis at the fused and unfused arrested and healed sites was seen, those phenomenon was defined as a instability sign. For such a case careful observation was carried out.
6. Treatment protocol
1) High calorie diet
For all children high calorie protein diet was prescribed when they were hospitalized. However, it was impossible to check it after discharge from hospital. Also it was impossible in the children under ambulant chemotherapy.
2) Anti-tuberculosis chemotherapy
For all children directly observed chemotherapy was practiced under the children’s parents’ and other family members’ supervision. In all children three drug regimen was adopted: isoniazid (INH, H), streptomycin (S), and para-aminosalicylic acid (PAS, Pa) for 18 months formula ([3HSPa], 15HPa) was used between 1971 and 1975. Since 1976, three drugs, isoniazid (H), rifampin (R), ethambutol (E), or pyrazinamide (Z) for 12 month (12RHE or 12RHZ) was adopted. In none of children secondary drugs or new drugs were used. For some children pyridoxine was prescribed.
3) Supplementary immobilization
Head halter traction was routinely applied in all cervical spine tuberculosis cases for 7–10 days before definite therapeutic protocol was finalized. Before 1980, Minerva cast in 14 children was applied for 3 month because of the noted cervical instability. Thereafter, four-post cervical brace was applied in seven children, and halo-shoulder apparatus for 4 months in 12 children. Seven children were treated without any supporting apparatus.
Results
1. Laboratory data
1) Hematologic findings
Erythrocyte sedimentation rate at the time of initiation of chemotherapy was 41 mm/hr (range, 31–54 mm/hr) and 14 mm/hr (range, 9–17 mm/hr) at the post-chemotherapy 3 months.
2) C-reactive protein
Average C-reactive protein at pre-chemotherapy and post-chemotherapy 3, 6, 9, and 12 months was 3.9 mg/dL (range, 2.3–4.7 mg/dL), 0.5 mg/dL (range, 0.23–1.4 mg/dL), 0.05 mg/dL (range, 0.04–0.16 mg/dL), 0.06 mg/dL (range, 0.03–0.13 mg/dL), and 0.03 mg/dL (range, 0.01–0.09 mg/dL), respectively.
2. Intervetebral disc condition
On images complete disc destruction was noted in two (5.0%) out of 40 cervical tuberculosis, eight (26.7%) out of 30 dorsal spine tuberculosis, and six (19.4%) out of 31 lumbar and lumbosacral tuberculosis. All those 16 children (15.0%) with complete disc destruction were the advanced one at the time of initiation of chemotherapy.
3. Disease arrest and cure and stability of the diseased segment
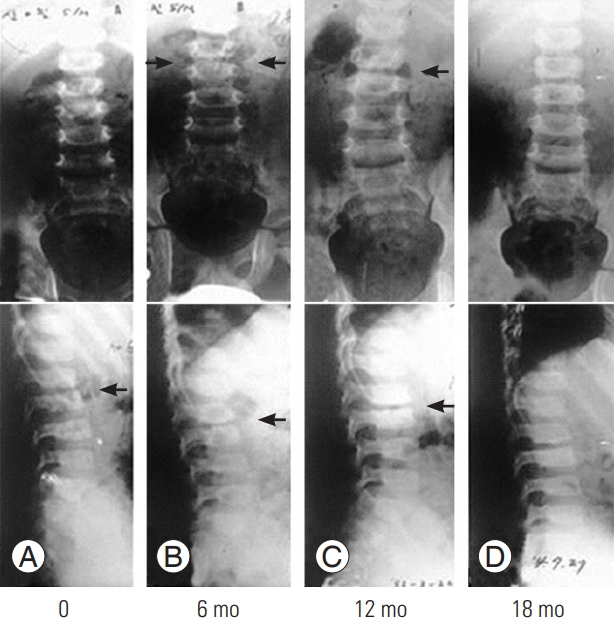
In some cases slow drug response was observed in the early stage of drug therapy, but finally it did not influence the final cure. There is no drug non-responder. Spontaneous intercorporal fusion in 40 cervical, 30 dorsal, and 31 lumbar and lumbosacral tuberculosis occurred in five cases (12.5%), seven cases (23.3%), and four cases (12.9%), respectively at the end of chemotherapy (Figs. 1, 2).
In all cases the disease arrest sign was observed at the average post-chemotherapy 3 months (range, 2.5–4.3 months), and cure was obtained at post-chemotherapy 12 months by maintaining all the radiological and laboratory findings of the arrest point without change, and additional augmented signs of reformation of destroyed bone and modeling. Stability of the diseased segment was obtained together with the disease arrest and cure irrespective of intercorporal fusion
4. Change of kyphotic curve during chemotherapy and afterward
1) Cervical tuberculosis (n=40 cases)
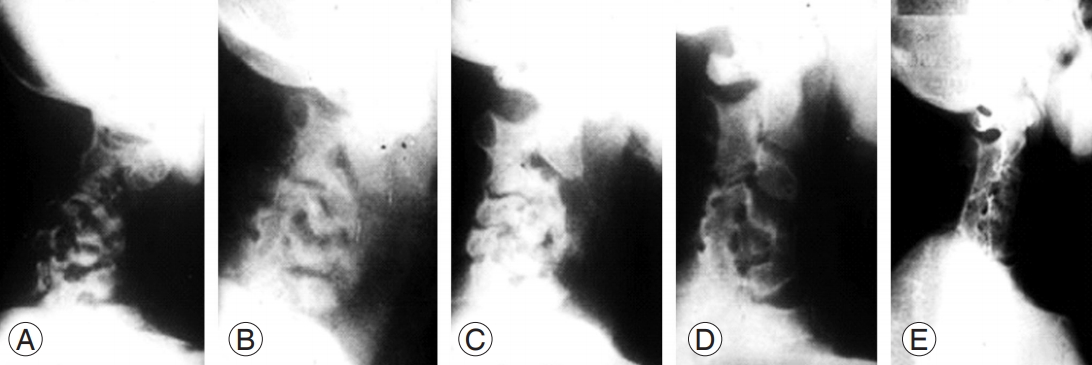
Among 40 children (36 cervical and four cervicodorsal junction cases): 10° kyphotic angle was maintained in eight children (20%) without change, and 8° kyphotic angle decreased to 3° in six children (15%) at the end of treatment. In 26 children (65%) initial 8° kyphotic angle increased to 16° at the end of chemotherapy (Table 1, Fig. 2).
2) Dorsal tuberculosis (n=30 cases)
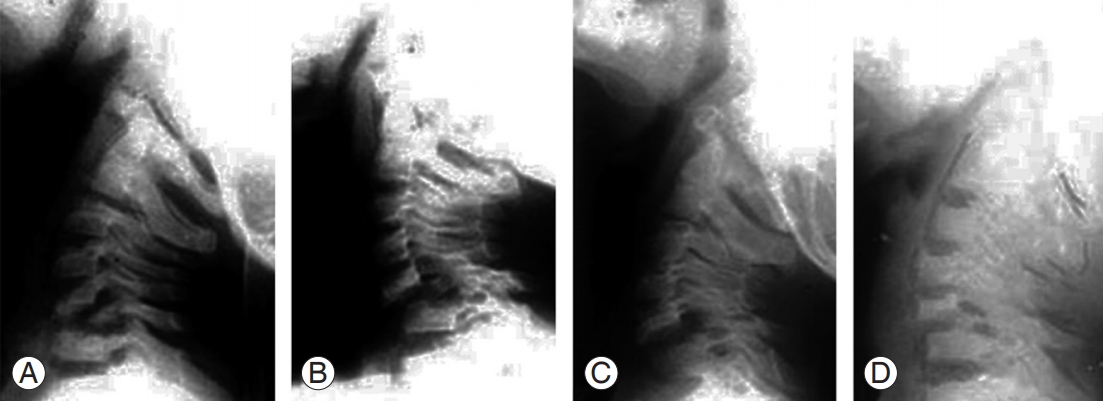
Initial 13° kyphotic angle was maintained till end of treatment in seven children (23.3%), and in four children (13.3%) average initial 15° kyphotic angle decreased to 10° at the end of treatment. In 19 children (63.3%) average initial 11° kyphotic angle increased to 23° at the end of treatment (Figs. 3, 4).
3) Lumbar and lumbosacral tuberculosis (n=31 cases)
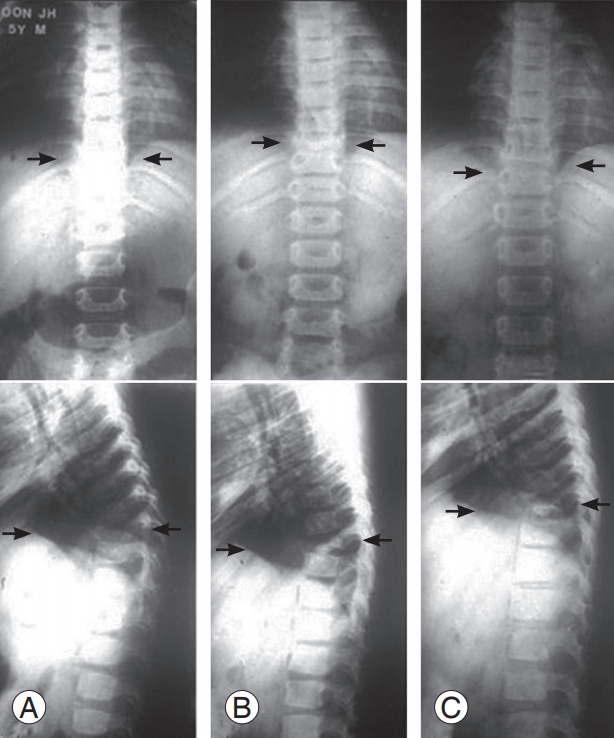
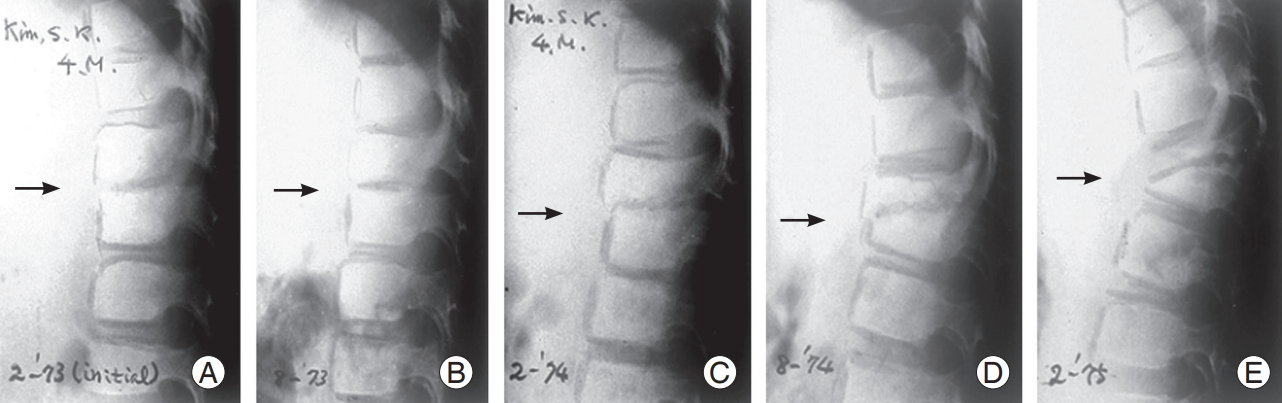
In five children (16.2%) the average initial 5° kyphotic angle was well maintained till end of chemotherapy, and in four children (12.9%) the average initial 12° kyphotic angle decreased to 4° at the end of chemotherapy. In 22 children (70.9%) the average 14° initial kyphotic angle increased to 25° at the end of chemotherapy (Figs. 5–7).
In summery among the 101 children, 20 children (19.8%) could maintain the initial angle, and initial angle decreased in 14 children (13.7%), while in 67 children (66.3%) initial angle increased. This fact evidently suggested that in the advanced pediatric spinal tuberculosis progress of kyphosis is an inevitable complication during and after treatment because of growth plate damage (Table 1). Main cause of the progressive kyphosis was the single wedged fused bloc or unfused two wedged vertebrae. Non-fusion was not the main cause of the progressive kyphosis.
Discussion
The primary objective of the management of the pediatric spinal tuberculosis was to save life through curing the disease, and secondly to minimize the disease-related complications such as spinal deformity and/or neurological deficit by early 1980. Thus, the management aimed primarily curing the disease and secondary the prevention of destruction of the infected spinal column maximally, protection of the spinal cord and nerves, and/or hastening the recovery of paralysis, and maintenance of the stability of the diseased segment [2,3,5-8,17]. By the 1980, diagnostic and assessing tools was limited, though nowadays for diagnosis and assessment of therapeutic response various imaging studies can be utilized such as simple radiograms, computed tomography, bone scan, MRI, and positron emission tomography. None of those could solely provide the definite healing points. Rajasekaran [9,10] mainly focused to observe the natural course of affected spinal spinal column curve change pediatric tuberculosis of spine, irrespective of chemotheraphy, but they did not report the results of comparison of nontreated and ambulatorily treated children.
All children in the current series presented the different disease stages at the time of initial examination. Some individualistic management modification was inevitable. Selection of the type of management is important; conservative versus surgical under the cover of the directly observed anti-tuberculous chemotherapy [17]. Disc destruction lagged far behind the bony vertebral destruction because disc destruction is rather mechanical than enzymatic. Judicious selection of the management was mandatory by the treating physicians: medical treatment versus surgical treatment. Surgery should be indicated only for the complicated tuberculosis. Surgeons should assess the growth plate condition in the lesion before surgery through the image studies. MRI was found to be the most reliable one; MRI demonstrated the severity of bony vertebral destruction, disc sparing as well as the extraosseous soft tissue extension of the disease. MRI-based observation was the best method in identifying the evidence of healing. But generally the healing status was defined on basis of clinical and radiological parameter which lagged behind the clinical improvement by 3 months by most of the studies.
Up to now there have been controversies regarding the duration of antituberculous treatment (ATT) because each individual responded differently to ATT even under the same drug formula. Thus, it was essentially needed to evaluate the spinal lesions clinically, hematologically, and radiologically and the contrast MRI to document healing of the vertebral lesion after 8 months of ATT and subsequently to decide for the continuation or stoppage of treatment [18]. The current authors did the same practice.
When anterior surgery is indicated for the lesion, radical surgery should not be practiced, because it destroys the remaining growth plate in the lesion. Gentle less aggressive debridement is the choice to preserve the remaining growth cartilage. As regard to this issue, the current authors have chosen the less aggressive debridement procedure for all the pediatric spinal tuberculosis irrespective of the disease stage [17].
Prediction of progress and non-progress of kyphotic deformity could be possible at the time of initiation of chemotherapy, but its predictive accuracy was rather low. The change of the kyphotic deformity primarily was not directly related with the drug efficacy, and was rather related with the severity of tissue destruction including the growth plate cartilage at the time of initiation of chemotherapy. Even under the same therapeutic drug formula, there were three clinical types of the curve change in the current series: (1) non-change (static) form, (2) deformity progress form, and (3) deformity decrease form.
It is acceptable to stop the continuous observation for the non-curve progress form at the end of chemotherapy. However, in the two remainders follow-up observation should be continued till fixation of residual deformity. Differentiation of the curve type could be possible at least at the post-chemotherapy one year. The diseased corporal foci healed in the two different patterns: fused and unfused (non-union). The low rate of spontaneous intercorporal fusion in children could be theoretically attributed to the local production of two bone formationrelated factors; local production of BMP antagonists (nogging and chordin) to maintain the continuous vertebral growth, while spontaneous intercorporal fusion in adult patients in roughly over 90% because of speculated local production of BMP only.
In either case of the current series the healed original foci did not show sign of instability. As regard the stability of the healed diseased focus, most treating physicians paid attention whether the stability could be obtained and being maintained permanently or not. However, as far as the current authors’ observation is concerned, stability of the healed diseased segment was maintained even in the cases of the non-fusion (fibrotic union) till the end of observation.
As regard the growth of the fused Pediatric bloc vertebrae, there are two different opinions: one by the British MRC’s tuberculosis survey teams [4] and Schulitz et al. [1], and the other by Upadhyay et al. [12] in Hong Kong. The current authors support the former one [17]. The MRC [4] and Schulitz et al. [1] reported that in the pediatric spine there may be progressive kyphosis despite a solid fusion because the continuing growth in the posterior element of the spinal column may create the further deformity, and they reported the anterior fusion alone had the worst prognosis in terms of progressive kyphosis [1,11]. Combined anterior and posterior fusion decreased the incidence of kyphosis. On the other hand, Upadhyay et al. [12] showed that a short anterior spinal arthrodesis done at an early age was not associated with progress of deformity during growth and development from the disproportionate posterior spinal growth. Therefore, they did not recommend a posterior fusion to stop posterior growth [12].
Spontaneously fused block vertebra during and after chemotherapy becomes stable, but it is not a good news. There may be a possibility of progressive kyphosis due to continuing growth in the posterior spinal element as mentioned above, and may create further deformity. Spontaneous intercorporal fusion rate during chemotherapy in children is less than 15%. Thus, it is important to observe the influence of the healed unfused segment on kyphosis. If the rapid progress of kyphosis which exceed over 50°–60° should not be allowed, because in those cases the late unrecoverable paralysis develop gradually [14,15,18]. Those cases with rapidly progressive deformity and unacceptable deformity at the end of chemotherapy, need not only the surgical deformity prevention procedure, but also corrective surgical procedures should be carried out.
However, we treating physicians should keep in mind that the undamaged growth cartilage in the disc of the pediatric spinal tuberculosis lesion participates not only in repairing of the destroyed bony vertebra, but also in modeling of the healed bony spinal lesion. The noteworthy message in this study is that most reliable predicting assessment time of residual kyphosis is the end of the disease cure.
In all children of the current authors’ series, spinal tuberculosis healed without any drug-related complications in spite of the progress of kyphosis even after cure in 67 children (66.3%). However, the high percentile incidences of residual kyphosis did not indicate the failure of the chemotherapy. Because this unacceptably high rate of residual kyphosis was primarily the end-product of the late discovery and treatment delay in the advanced disease, and secondly due to the patients poor home economy which deprived the opportunity from children to be seen earlier by the physicians. Over two-third of the victim children belonged to the charity service care group up to the end of 1980. That period was nationally the uninsured era in Korea. There was no government supported Medicare system at that time.
Based on the current study results, early discovery of the diseased children by the regional and local health care service personnel and the early management by the physicians are stressed. Those are the keys not only for the cure of the disease, but also reduction of the disease-related crippling.
In summary the successful management of the pediatric spinal tuberculosis should result not only in cure of the disease, but also prevention and/or minimization of the disease-related complications such as residual kyphosis and neurological involvement.
It is reminded to all the treating physicians that medicine is the basic curative agent, and that surgery is only the adjuvant therapeutic means for the complicated conditions. Also the continuous vigilant observation is recommended till the growth maturity in the children particularly presenting the evidence of spinal deformity progression.