Investigation of Comorbidity, Trauma History, and Osteoporotic Fractures in the Postmenopausal Population: A Nationwide, Observational, and Cross-Sectional Study of Korean Orthopedic Outpatient Clinics
Article information
Abstract
Study Design
A nationwide, observational, and cross-sectional study targeting postmenopausal patients from 62 orthopedic outpatient clinics in Korea between October 2010 and February 2011.
Purpose
This study was carried out to investigate comorbidity, trauma history, and the status of osteoporotic fracture treatment in Korean postmenopausal women.
Overview of Literature
There has been little reports on the comorbidity, family history, trauma history, and treatment status of osteoporotic fractures in patients visiting the orthopedic outpatient clinics in Korea.
Methods
A total of 1,255 postmenopausal women between the ages of 50 and 80 years were enrolled in the study and the population distribution was reflected by region. Comorbidity, familial history of osteoporosis, familial history of osteoporotic fracture, history of falls, and status of osteoporotic fracture management were evaluated using an interview and questionnaire. The relationship between family history of osteoporosis and bone mineral density was analyzed.
Results
A number of patients (23%) had a family history of osteoporosis and 16.5% had a family history of fractures. Most (64.7%) of the patients had one or more comorbidities, including 58.8% exhibiting a chronic disease and 16.4% suffering from diseases that restrict exercise or walking. The results of the questionnaire indicated that 21.8% of these fracture patients had experienced a fracture previously and that the most common type of fracture was that of the spine. Lumbar spine bone mineral density was found to be lower in the presence of family history of osteoporosis.
Conclusions
Postmenopausal women are liable to have osteoporotic fractures due to the high prevalence of osteoporosis, a history of falling, and the comorbidity with diseases that restrict ambulation. A better understanding of postmenopausal women in the orthopedic outpatient settings is important to the management of osteoporotic fractures.
Introduction
Estrogen depression makes postmenopausal women more vulnerable to osteoporosis due to decreased osteoblast function. It is well known that increasing age is associated with decreasing bone mineral density (BMD) in postmenopausal women. According to a study published in 2017 [1], the average life expectancy of South Korean women is likely to exceed 90 years in 2030 and, in these women, complications such as osteoporosis and fractures will increase rapidly. Therefore, the clinical significance of osteoporosis and osteoporotic fractures in Korean postmenopausal women is expected to escalate further. As orthopedic surgeons are the first medical practitioners to come into contact with fracture patients, epidemiologic information gathered from orthopedic outpatient clinic patients is useful to them. However, orthopedic surgeons are often not familiar with the data even though postmenopausal women as a population have many comorbidities and risk factors for osteoporotic fractures. As there have been no previous reports measuring these parameters to date, the purpose of this study was to investigate comorbidity, family and trauma history, and status of osteoporotic fracture treatment in postmenopausal women who have visited orthopedic outpatient clinics in Korea.
Materials and Methods
1. Study design
This was a nationwide, observational, and cross-sectional study targeting postmenopausal patients in 62 orthopedic outpatient clinics between October 2010 and February 2011 in Korea. The methods are as described previously [2,3]. To compensate for regional differences between areas, data provided by the National Statistical Office of Korea were used to identify the distribution of women over the age of 50. The same proportion of patients was recruited from each of four regions, namely the Seoul Metropolitan, Central, Youngnam, and Honam areas. A total of 1,281 patients was enrolled in this study.
2. Inclusion criteria
Among women 50 years of age or older who visited orthopedic clinics, patients who had undergone menopause, as confirmed by a physician, were included. Postmenopausal patients were defined as women for whom 12 months had passed since their last menstrual period at the time of enrollment [2,3].
3. Exclusion criteria
We excluded premenopausal women, subjects ≥80 years of age, women who had undergone a high-energy trauma such as a traffic accident within the past 3 months, subjects who had suffered non-vertebral fractures in the 6 months prior to the study registration, and people who did not have the cognitive ability to be involved in the research (i.e., the skill to understand the contents of the survey) based on the discretion of the investigator [2,3].
4. Demographic information and medical history
Patients were evaluated for age, height, weight, years following menopause, family history of osteoporosis in the mother and siblings, family history of osteoporotic fracture in the mother and siblings, living environment (residential area, facilitated residence, family residence, etc.), type of insurance (medical insurance or medical care), and medical record. In addition, we identified comorbidities such as hypertension, diabetes, hypercholesterolemia, osteoporosis, rheumatoid arthritis, hyperthyroidism, hyperparathyroidism, degenerative knee osteoarthritis, foot disease, spinal disease with claudication, and Parkinson’s disease. Furthermore, details about any history of falls and traumas experienced within the year prior to the study period were noted. If there was a history of fracture, we determined whether the fracture occurred before or after the onset of menopause, the site and cause of the fracture, and the treatment received [2,3].
5. Bone mineral density
The BMD of patients was measured at points in the lumbar spine, femoral neck, and total hip joint using dual energy X-ray absorptiometry. If data measured within 3 months prior to the study were available, they were used. Measurements were carried out according to the manufacturer’s instructions for each measuring instrument. BMD data were statistically analyzed for correlation with a family history of osteoporosis, exercise- and movementlimiting diseases, and a history of steroid treatment [2,3].
6. Ethics statement
The study was conducted in accordance with the Declaration of Helsinki and approved by the institutional review board (IRB approval no., 06-2010-131) of Seoul Metropolitan Government-Seoul National University Boramae Medical Center. All patients provided written informed consent [2,3].
Results
This study is a follow-up to research conducted in 2014 [2]. A total of 1,255 patients were included in this study. The mean age of the patients was 63.2±7.7 years, the age at the time of menopause was 48.8±5.2 years, and the mean postmenopausal period was 14.5±9.0 years. Among the subjects, 209 (16.8%) lived alone and 1,021 (82.3%) lived with their families. A total of 1,083 (87.3%) resided in a city or county, and 158 (12.7%) resided in a town or township. According to the details collected about medical insurance, 1,155 (95.0%) of the patients were enrolled as national health insurance subscribers and 59 (4.8%) were receiving medical care.
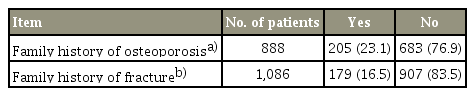
1. Family history
Of the postmenopausal women who visited the orthopedic outpatient clinic, 23% had a family history of osteoporosis and 16.5% had a family history of fractures (Table 1). The response rates to questions about a family history of osteoporosis and family history of fractures were 70.7% and 86.5%, respectively. Patients tended to remember a family history of fracture more than a family history of osteoporosis.
2. Comorbidity
The most common comorbidities among postmenopausal women who visited orthopedic outpatient clinics were hypertension (49.1%), osteoporosis (15.6%), diabetes (13.5%), hyperlipidemia (12.3%), and arthritis of the knee (11.2%). Table 2 summarizes the prevalence of other chronic illnesses or diseases. Most patients (64.7%) had one or more comorbidities. The percentage of patients with chronic diseases such as hypertension, diabetes, hyperlipidemia, osteoporosis, rheumatoid arthritis, hyperthyroidism, hyperparathyroidism, spinal diseases with claudication, and Parkinson’s disease was 58.8%. In addition, the proportion of postmenopausal women with diseases that limited exercise or walking ability, such as severe knee osteoarthritis, spine disease with claudication, foot disease, and Parkinson’s disease was 16.4%. The prevalence of rheumatoid arthritis, hyperparathyroidism, and a history of steroid injection lasting over 3 months were 1.8%, 0.1%, and 1.5%, respectively. All of these are possible causes of secondary osteoporosis.
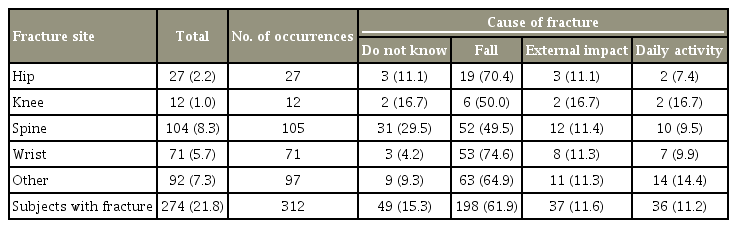
3. Causes and treatment of fractures with respect to fracture sites
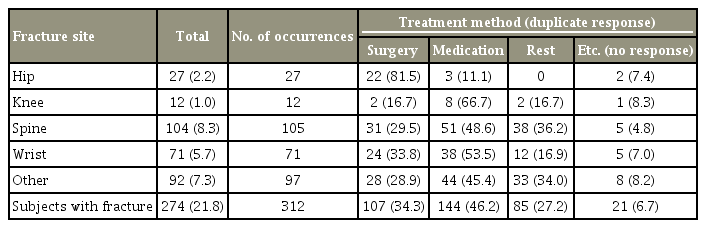
A number of patients (n=274, 21.8%) had experienced previous fractures at the same location. These included 8.3% of the patients who had spinal fractures; 5.7% who had wrist fractures; 2.2% who had hip fractures; and 1.0% who had knee fractures (Table 3). A total of 7.3% had experienced other fractures. The highest proportion of fractures were caused by falls (61.9%), then external impact (11.6%), and daily activities (11.2%).
Most patients (81.5%) with hip fractures underwent surgical treatment while patients with wrist fractures, vertebral fracture, and knee fracture were treated surgically in 33.8%, 29.5%, and 16.7% of cases, respectively. In total surgical treatment was provided in 34.3% of cases (Table 4).
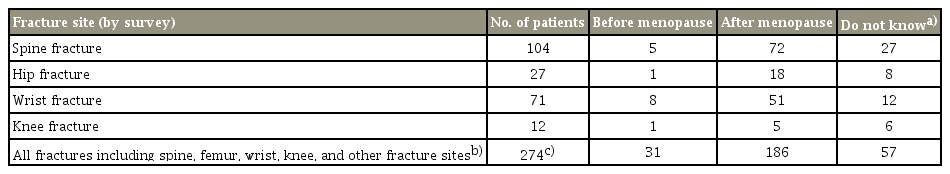
Answers to the questionnaire indicated that of the total number of fractures (n=277), 186 of these occurred after menopause and only 31 fractures occurred before menopause. Fifty-seven patients did not remember whether their fracture occurred before or after the menopause (Table 5).
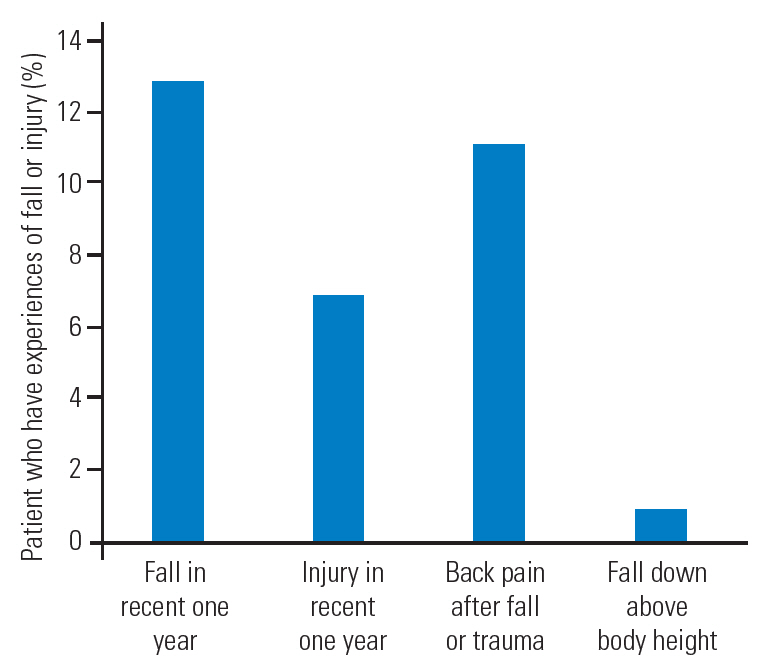
Among the subjects, 161 (12.8%) had fallen within the past year and the average number of falls was 1.4 per year. A total of 6.9% of patients had experienced a trauma or traffic accident within the past year and the average number of injuries was 1.0 per year. Of these patients, 138 (11.0%) experienced back pain following the fall or trauma. While most falls were from that was below body height, some patients (0.9%) had experienced a fall from a distance greater than body height (Fig. 1).
4. Factors associated with bone mineral density
In this study, we investigated whether a family history of osteoporosis, the presence of diseases that limit exercise and walking, and previous steroid treatment were associated with the BMD of the lumbar spine, femur, and total hip. Of these criteria, the only association identified was between family history of osteoporosis and lower BMD of the lumbar spine (p=0.0437). However, we could not confirm any association between the presence of diseases that limit exercise and walking and previous steroid treatment with a family history of osteoporosis.
Discussion
Postmenopausal women appear to have increased incidences of various comorbidities as well as decreased BMD. The prevalence of metabolic syndrome, found in 13%–45% of women of reproductive age, increases by 32%–70% after menopause [4,5]. Additionally, menopause itself has been reported to be an independent risk factor for type 2 diabetes regardless of body weight and age [6,7]. In addition, the prevalence of hypertension in postmenopausal women is 41%, which is higher than that in men [8]. Therefore, it is important to understand potential comorbidities found in postmenopausal fracture patients in orthopedic outpatient clinics; to date, there has been little research on this population [9]. In our study, 64.7% of postmenopausal women who visited orthopedic outpatient clinics had concomitant diseases and more than half had chronic diseases. The incidence of these comorbid diseases is expected to increase gradually as the population ages. Patients who have parathyroid hormone disease, undergo long-term steroid usage, and exhibit rheumatoid arthritis also accounted for some of the fracture clinic outpatients. The presence of osteoporotic fractures is of particular importance in this group of patients.
Osteoporotic fractures are a major complication in postmenopausal women and are one of the major causes of socioeconomic burden [10]. Most osteoporotic fractures occur after menopause and in this study at least 67.8% (up to 88.6%) of these fractures happened after menopause. The most common cause of osteoporotic fracture was falling, followed by minor trauma, and daily living. In this study, 12.8% of patients had experienced a fall within the year and 6.9% had experienced a trauma or traffic accident within the year. The causes of falls or trauma in elderly patients have been widely reported. In general, about half of these falls are due to jamming of the feet or slipping. Another 20% are caused by syncope, 20% are due to loss of balance, and the rest are the results of other factors [11]. When considering the risk of osteoporotic fracture, any history of falling and minor traumas should be taken into account in the outpatient setting.
The most frequent location for an osteoporotic fracture in postmenopausal women was the vertebrae. However, surgical treatment was performed in only 29% of patients with this type of fracture compared with 81.5% patients with hip fractures that were surgically treated. Kung [12] have stated that the surgical treatment of vertebral fractures is low because many patients are asymptomatic and the cause of the back pain is difficult to distinguish. Nonetheless, osteoporotic vertebral fractures should not be ignored considering that the presence of existing osteoporotic fractures in itself is a risk factor for another vertebral fracture, decreasing quality of life [13], and increasing mortality [14].
Several cohort studies have been conducted on the family history of osteoporosis and osteoporotic fractures. Fox et al. [15] reported that the risk of hip and wrist fracture increased by 50% and 64%, respectively, in the presence of parental history of osteoporotic fracture of the hip or wrist. A family history seems to increase the risk of fracture independently of BMD [15]. Other researchers found a negative correlation between a fracture history in a sister and 10-year fracture-free survival in perimenopausal women [16]. In our study, the family history of osteoporosis and fractures were reported as 23.1% and 16.5%, respectively. Few respondents knew of their family history of osteoporosis. The number of people who knew this information was lower than the number who knew about the prevalence of osteoporosis in postmenopausal women. This was likely to be underestimated in view of the low response rate.
In this study, lumbar BMD was found to be statistically lower in patients with a family history of osteoporosis than in those with no family history of the condition. According to the present study, a family history of osteoporosis may be helpful in predicting the occurrence of osteoporosis in the lumbar spine for orthopedic patients. Soroko et al. [17] reported that osteopenia occurred in more by 51% of women with a family history of osteoporosis in their cohort study of Caucasian women aged 60 to 89 years. However, there was no difference in BMD for patients with diseases that limit exercise or gait and those who had been treated with steroids for 3 months or more, which are known risk factors for osteoporosis. These results might have been limited by a failure to control other confounding factors in this study.
This study has limitations as a cross-sectional study and it is impossible to explain the causal relationship. Postmenopausal women who did not attend the outpatient clinic because of disability or other reasons could have fallen out of the study and therefore there may be a selection bias. Additionally, the collection of data on the family history of osteoporosis was memory-dependent and self-reported. Furthermore, the paternal family history was not used in this study. Nevertheless, this is the first study in which a nationwide, cross-sectional study on orthopedic outpatients was performed to examine the multifaceted approach to managing the risk factors for osteoporotic fracture in Korean postmenopausal women.
Conclusions
In conclusion, postmenopausal women visiting orthopedic outpatient clinics are a characteristic population group with a high degree of comorbidity including osteoporosis and high risk of osteoporotic fracture. Among the osteoporotic fractures exhibited by postmenopausal women, vertebral fractures may be the most frequently found, but also the most overlooked. Diagnosis of osteoporotic vertebral fractures and the evaluation of osteoporosis should not be missed for this population. A family history of osteoporosis can also be used to evaluate the risks of osteoporosis and osteoporotic fracture.
Notes
No potential conflict of interest relevant to this article was reported.