Impact on Neurological Recovery of Transforaminal Debridement and Interbody Fusion versus Transpedicular Decompression in Combination with Pedicle Screw Instrumentation for Treating Thoracic and Lumbar Spinal Tuberculosis
Article information
Abstract
Study Design
Retrospective study.
Purpose
To compare the neurological outcome of transforaminal debridement and interbody fusion with transpedicular decompression for treatment of thoracic and lumbar spinal tuberculosis.
Overview of Literature
Few articles have addressed the impact of neurological recovery in patients with tuberculosis who were treated by two different operative methods via the posterior-only approach.
Methods
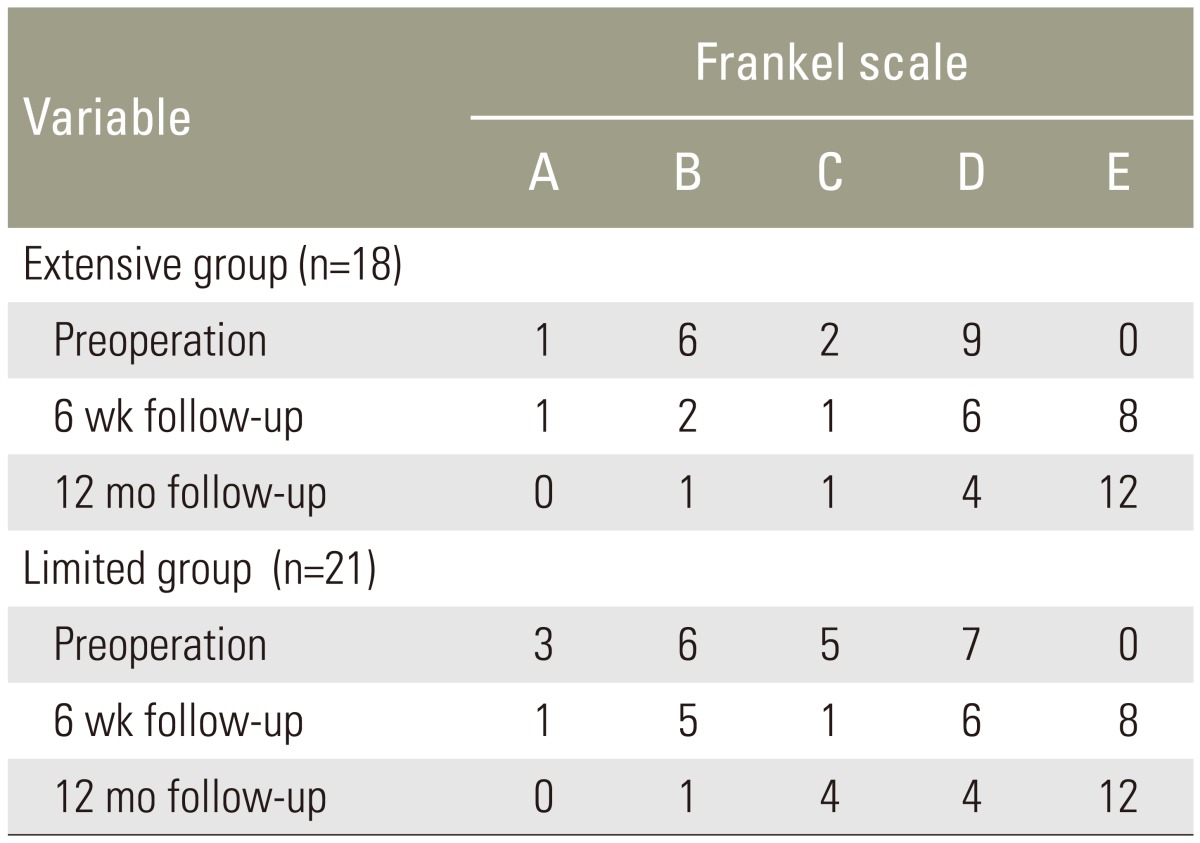
Clinical and radiographic results of one-stage posterior instrumented spinal fusion for treatment of tuberculous spondylodiscitis with neurological deficits were reviewed and analyzed from 2009 to 2013. The extensive (E) group consisted of patients who received transforaminal debridement and interbody fusion, whereas transpedicular decompression was performed on limited (L) group. Rapid recovery was improvement of at least one Frankel grade within 6 weeks after operation. Otherwise, it was slow recovery.
Results
All 39 patients had improved neurological signs. The median follow-up period was 24 months. Proportionately younger patients (under 65 years of age) received extensive surgery (15 of 18, 83.3% vs. 11 of 21, 52.4%; p=0.04). The mean operative time and blood loss in the group E were higher than in the group L (both p<0.01). With regard to type of procedure, especially at thoracic and thoracolumbar spine, patients who underwent extensive surgery had rapid neurological recovery significantly different from those of limited surgery (p=0.01; Relative Risk, 3.06; 95% Confidence Interval, 1.13 to 8.29).
Conclusions
Transforaminal debridement and interbody fusion provides more rapid neurological recovery in patients with thoracic and thoracolumbar spinal tuberculosis compared to transpedicular decompression.
Introduction
Spinal tuberculosis accounts for approximately 50% to 66% of all cases of osteoarticular tuberculosis and imaging is important for characterizing lesions, as osteolytic patterns and destructive behaviors likely to produce kyphosis and instability [12]. The response to non-operative treatment is occasionally slow and kyphotic deformity is likely to progress during the follow-up period [3]. Therefore, surgery is superior, particularly in cases when non-operative management has failed or severe kyphosis/instability has developed with or without neurological deficit [45]. Anterior radical surgery (i.e., the Hong Kong operation) for spinal tuberculosis reported by Hodgson and Stock has been considered the gold standard [67]. The most important advantage of the traditional approach is that it allows a full radical resection of the infectious focus [5]. However, a review of the recent literature shows the evidence supporting autofusion of anterior spinal segment affected by tuberculous (TB) disease can be obtained without anterior surgery [891011].
Transforaminal thoracic interbody fusion or transforaminal lumbar interbody fusion has been modified to treat spinal tuberculosis in a one-stage posterior transforaminal debridement, interbody fusion plus pedicle screw instrumentation [81011121314]. Moreover, the posterior transpedicular approach has recently become popular as an alternative method and a less invasive surgical procedure [151617].
In the present study, the difference of the two surgical procedures regarding the treatment of TB spondylodiscitis by the single-stage posterior approach and instrumented stabilization was analyzed in terms of rapidity of neurological recovery, general surgical outcomes, radiological results and postoperative complications.
Materials and Methods
The study was approved by the Institutional Review Board of Maharat Nakhon Ratchasima hospital. The electronic medical records of 40 consecutive patients admitted with neurological deficits resulting from TB spondylodiscitis during a 48-month time period from January 2009 to January 2013 were retrospectively reviewed. Confirmation of the diagnosis by histopathology, Mycobacterium tuberculosis culture and/or polymerase chain reaction (PCR) for tuberculosis from surgical biopsy specimens was available in all cases. Patients were included in the analysis if they had a follow-up of more than 12 months. A 47-year-old female with alcoholic liver cirrhosis who died of spontaneous bacterial peritonitis and gram-negative bacillus sepsis 6 months after extensive surgery was excluded from the study. A total of 39 cases were included; all were operated on by a single surgeon (W.S.).
The extensive (E) group was composed of patients with severe destructive vertebral lesions and low anesthetic risk. One-stage posterior transforaminal debridement and interbody fusion with bone graft was carried out to achieve sufficient stability. Laminectomy was done and the entire space between the medial walls of the pedicles was exposed. Articular process removal and pediculectomy on the severely affected side of lesion were performed to reach the diseased portion of vertebral bodies. Unilateral costotransversectomy was utilized in thoracic spines and thoracic nerve roots on the focal level were sacrificed for better exposure. In lumbar lesions, sufficient exposure for debridement was obtained deliberately by unilateral total facetectomy. The location of the lumbar nerve root was identified to ensure that postoperative nerve palsy would not be encountered from iatrogenic injury. Curettes and burr drills were used to remove lesions including the infected vertebral body sequestrum, necrotic intervertebral disc, pus and caseous granulation tissue as thoroughly as possible. Autogenous corticocancellous chips were placed around the anterior two-thirds of the space created by debridement and a tricortical iliac bone graft was inserted to reconstruct the anterior column. Finally, posterolateral arthrodesis of the instrumented levels with local autologous bone was undertaken (Fig. 1).

(A) Extensive surgery was performed on a 63-year-old male with low back pain and paraplegia for 2 months, with transforaminal debridement and interbody fusion using an autogenous iliac crest bone graft (white arrow), postoperative radiographs showing well-corrected sagittal alignment. (B) Preoperative magnetic resonance imaging (MRI) of the thoracic spine, T2-weighted in the sagittal and axial plane show typical pattern of T11–T12 vertebral destruction with intervening disc involvement, and severe vertebral collapse is noted (black arrow). Postoperative MRI shows a wide thoracic canal and well-maintained sagittal alignment at the 12-month follow-up. (C) Extension and flexion radiographs of the same patient at the 24-month follow-up.
The limited (L) group included patients who had less vertebral destruction and serious medical condition. This group could be treated with single-stage posterior decompression by transpedicular curettage and additional decompression procedures included hemi-laminectomy or complete laminectomy. The paraspinal abscess was drained using curettes and the infected bone was removed using pituitary forceps. This step was performed on the basis of more neurological and radiological signs. The patterns were similar in the thoracic and lumbar regions. No attempt at radical debridement was undertaken and no anterior reconstruction with a strut graft was carried out. Adequate stability and positively influenced the healing of bone defect were accomplished via long-segment instrumentation in spite of a small dead space often encountered at the early stage. In the final step, posterolateral fusion using autologous local bone graft of the instrumented segments was performed.
The global standard screw (GSS, GS Medical Co., Ltd, Geumcheon-gu, Seoul, Korea) pedicle screw system was used in all patients. Screws were inserted in the usual manner and also placed in pathological vertebrae if the upper part of the vertebral body and the pedicle was not involved. The patients could ambulate with external orthotic support comprising thoracolumbar or lumbosacral orthosis for at least 3 months postoperatively. All cases received isoniazid (I, 5 mg/kg), rifampicin (R, 10 mg/kg), pyrazinamide (Z, 25 mg/kg) and ethambutol (E, 15 mg/kg) for the first 2 months (2IRZE), then I/R/E for at least 10 months later (10IRE) until the abnormal levels of C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR) as markers of infection returned to normal or were significantly decreased after treatment. All patients remained in laboratory monitoring for at least 12 months postoperatively. Neurological outcome was evaluated by the Frankel classification [18]. Rapid recovery represented by improvement of at least one Frankel grade within 6 weeks after the surgery. Otherwise it was slow recovery. The visual analogue scale (VAS) score was used to assess pain symptoms [19]. Vertebral body loss (VBL) and angle of localized spinal deformity were measured as previously described [14]. Sagittal alignment was measured for each case on plain lateral radiographs by Cobb angle before and after the operation and at the final follow-up. The assessment of bony fusion was conducted as previously described [20]. Criteria were based on the standard of bone fusion: continuity of bony trabeculae bridging across the bone graft space, fusion segments not active (<3 degrees) on a flexion-extension radiograph and no gap at interface. All measurements were done by one of the authors (K.C.) who did not participate in the surgeries.
Baseline characteristics are presented as mean (±standard deviation) or median (interquartile range, IQR) for continuous variables and frequency (percentage) for categorical variables. Independent t-test was used for the comparison of the mean continuous numerical data and Mann-Whitney U test was used for the comparison of the medians. Categorical variable presented as percentages were analyzed using the chi-square test or Fisher's exact test when expected counts were less than five. Statistical analysis was performed to compare the outcomes using software program Stata for Macintosh version 12 (StataCorp LP, College Station, TX, USA).
Results
There were 25 men and 14 women with overall mean age of 53.8±17.6 years (range, 16 to 82 years). Group E was significantly younger than group L with a mean age of 47.2±19.2 years vs. 59.4±14.4 years (p=0.03). The majority of the patients (83.3%) that underwent extensive surgery were in the young age group (under 65 years of age), with statistical significance (p=0.04). Patients were followed-up for a median of 24 months (IQR, 18 to 30 months). The overall median preoperative CRP and ESR values were 78.9 mm/hr (IQR, 63.5 to 95.3 mm/hr) and 77 mg/L (IQR, 64 to 93 mg/L) respectively. Levels of both markers decreased gradually to normal values at 12 months. Significant differences in the mean operative time and intraoperative blood loss were observed between both operative groups (both p<0.01). No significant differences were noted between the two groups for length of stay in the hospital and postoperative hospitalizations. The most commonly found comorbidity was water-electrolyte imbalance (53.8%), followed by diabetes mellitus (35.9%) and anemia from chronic disease (33.3%). Underlying medical illnesses were demonstrated in all 21 (100%) patients in group L, while medical comorbidities had been recorded in 14 (77.8%) patients in group E; the difference between the groups was statistically significant (p=0.04). At weeks 2 and 6, VAS scores significantly decreased in both groups as compared to the preoperative scores (all p<0.01). There was a significant difference observed between the E and L group at 2 weeks (p=0.02), but no significant difference between groups at 6 weeks follow-up evaluation. Initial VBL was significantly higher in group E vs. group L (0.6, IQR 0.5 to 1.1 vs. 0.4, IQR 0.2 to 0.7; p=0.02). The mean correction of sagittal index and the final loss of correction in both groups showed significant differences (both p<0.01). Anywise, the differences between the groups were not statistically significant. All the patients demonstrated solid fusion at the 12-month follow-up. The E group had a significantly higher incidence of respiratory complications according to the using of postoperative ventilator when compared to the L group (61.1% vs. 23.8%, p=0.02), although the incidence of overall perioperative complications did not differ significantly between the groups. Tables 1 and 2 summarize the results of a comparative analysis between the groups.
In group L, pseudarthrosis was suspected in one case due to broken rods which was observed on plain radiograph 4 months after surgery. This patient did not complain of any back pain or pain in his legs while posterolateral fusion was still achieved radiographically by the longer time of greater than 12 months of follow-up; three-dimensional reconstructions of computed tomography scan were used to confirm fusion evidence in this 29-year-old male patient at 24 months postoperatively (Fig. 2). Another patient from group L (a 64-year-old male) was recommended to undergo repeated operation when a kyphotic deformity of adjacent segment abruptly progressed and the sites of noncontiguous relapse were seen on magnetic resonance image (MRI) scan 12 months after surgery, but he refused reoperation. Eventually, he was treated successfully with anti-TB drugs that extended an extra 12 months of therapy.

(A) Tuberculous spondylitis of T11–T12 (white arrowheads) and L5–S1 (black arrowheads) in a 29-year-old male patient, post-gadolinium T1-weighted magnetic resonance image in sagittal and axial plane show typical pattern of two vertebral bodies destruction, irregular rim enhancing intervertebral disc is presented. (B) Anterior-posterior view of plain lumbar spine radiograph at 4 months after limited surgery reveals broken rods but he did not complain of any back pain or pain in his legs, while posterolateral fusion was still achieved radiographically on lateral extension and flexion view. (C) Three-dimensional computed tomography scan was used to confirm fusion evidence at 24 months postoperatively.
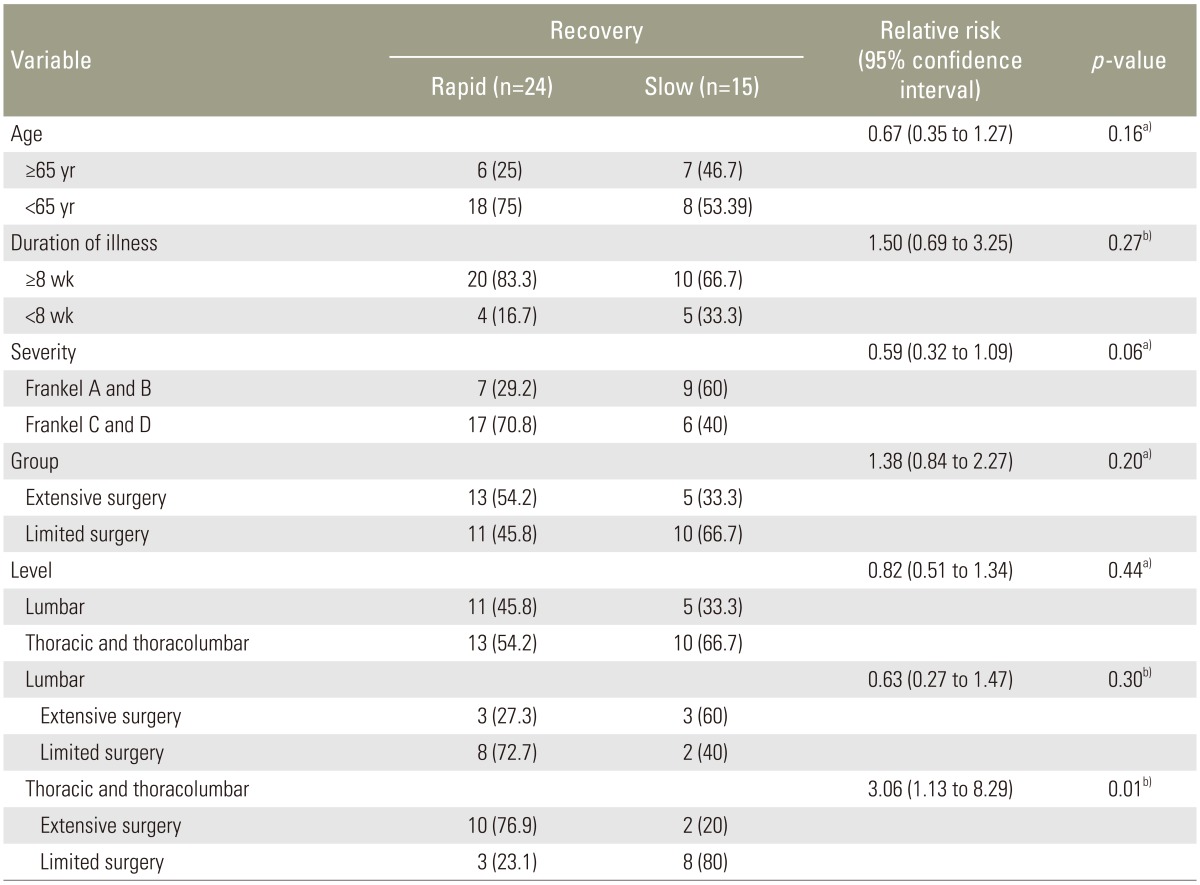
At the final follow-up, all 39 patients in both groups exhibited improved neurological function and did not demonstrate any deterioration (Table 3). There were no differences in the rate of recovery between age group, duration of illness, severity according to Frankel grade, operated level and operative group (all p>0.05). With regard to type of procedure, especially at thoracic and thoracolumbar spine, patients who were underwent extensive surgery had rapid neurological recovery significantly different from those of limited surgery (p=0.01; relative risk, 3.06; 95% confidence interval, 1.13 to 8.29) (Table 4).
Discussion
The diagnosis of spinal tuberculosis can be established on indolent onset of clinical symptoms, typical laboratory tests and compatible plain radiographic findings [12]. MRI is an important diagnostic tool for characterizing paravertebral and/or intraspinal extension of the disease prior to performing a surgical biopsy [21]. The microbiological diagnosis consists of both conventional methods (acid-fast microscopy, culture for anti-TB drug-susceptibility testing) and modern molecular techniques such as PCR on the biopsy specimens which are also valuable means for confirmation of diagnosis [22]. The treatment of spinal tuberculosis must be based on the use of effective anti-TB drugs, and early surgical decompression plays an important role in treating patients who suffer from severe pain and/or marked neurological impairment [3452223].
The surgical trend for Pott's paraplegia has constantly evolving as modern posterior spinal instrumentation which provides immediate stability and allows rapid patient mobilization [24]. With the minimal risk of anesthesia and with the less invasive spinal techniques, several investigators have started to report a wide variety of surgical procedures from this posterior approach and fixation to the treatment of TB spondylitis [81011121314151617]. Moreover, with the evidence suggesting that TB lesions that almost always affect the anterior column may achieve spontaneous fusion, the posterior approach represents a possible alternative surgical procedure in patients with less involved spinal tuberculosis [910]. Several spinal surgeons have advocated primary placement of transpedicular instrumentation for providing posterior stability and recovering activities of daily living after the operation [24]. Additionally, posterior pedicle screw instrumentation with fusion may be able to encourage neurological recovery because rigid stabilization enhances neurological improvement in traumatic spinal cord injury [25].
In the past, studies comparing the posterior approach with the anterior approach for spinal tuberculosis observed no difference in the outcomes between groups. Pu et al. [13], investigated 47 cases of thoracic and lumbar tuberculosis patients; 25 cases were treated by posterior debridement combined with interbody bone grafting and instrumentation, and the loss of kyphosis correction was also present in both groups (6.1° vs. 4.6° in posterior and anterior groups respectively). Lee et al. [15] studied 17 individuals with established TB on thoracic and thoracolumbar spine and reported that two or more vertebrae were involved in 94% of the patients, 10 of whom had undergone single-stage transpedicular decompression and posterior instrumentation. When the angle of kyphosis was <30°, significant kyphosis correction was found. But, the loss of correction was considerable in both groups (6.1° and 4.5° in posterior and anterior group, respectively). In the present study, the loss of correction was similar to prior studies [813141516]. Zhang et al. [12] studied 14 patients with upper thoracic tuberculosis; excellent neurological results were observed after one-stage debridement, combined interbody and instrumented fusion via posterior-only approach, and there was no significant loss of deformity correction at the final follow-up, with loss of correction being only 1.3°. The reasons for higher correction loss in the present study might be that TB lesions were not confined to only one segment, and placement of pedicle screws were attempted to fix inside the pedicle of the pathological vertebral body to reduce the extent of fixation, and also preserve more motion segments at the lumbar level [10]. The radiographic superiority of one-stage circumferential fusion using cage, especially in patients with lumbar spinal tuberculosis, might result in more favorable long-term outcome [26]. Similar findings were also published by other researchers, while the total operative time was longer, blood loss was higher and the titanium mesh cage that was used was more costly in cases of circumferential fusion [2728].
We offer several thoughts concerning the current one-stage posterior surgery performed as follows. The posterior approach was relatively uncomplicated. The long-segment instrumentation and posterolateral fusion could be successfully obtained stability in such a way that the spinal cord or nerve roots were not irritated and may promote efficient neurological recovery, thereby increasing mobility to hospitalized patients and decreasing complications of being in bed. The extensive clearance of caseous tissues that cause inflammatory response correlated with rapidly progressing recovery of function. Finally, the abrupt reduction of inflammation of neural elements was related to the improvement of disease activity and neurological grading.
Results of the two posterior decompressive surgical procedures for thoracic and lumbar tuberculosis were favorable. The overall incidence of complications in the two groups was not statistically different. But, the incidence of postoperative mechanical ventilation was significantly higher in group E compared with group L. This difference might be due to more complicated operative process, longer operative time and higher blood loss. Furthermore, the improvement in VAS scores on weeks 2 after surgery was significantly lesser in the E group. This might be because postoperative pain was slowly reduced for extensive surgery. The determination according to the type of the surgery should be individualized depending on the basis of the patient's general condition. Transforaminal approach in combination with internal fixation and posterolateral fusion with placement of interbody graft procedures were reserved for young (age <65 years) patients who could tolerate more complex reconstructive surgery. Performed extensively, these surgical procedures were suitable with lesions at spinal cord level because of wider exposure and more aggressive debridement of all infected tissues. So it might be assumed that there is the likely benefit of surgery to relieve myelopathy; rapid early neurological recovery was presently evident. Limited surgery with posterior transpedicular decompression in combination with pedicle screw instrumentation and posterolateral fusion procedures were better suited to less destructive forms of TB in aging adults with multiple comorbidities. Lastly and most importantly, completion of a full course anti-TB therapy and surgeon's surgical experience were the two key points to achieve success in reaching the goals of the treatment, regardless of the type of operation.
In the present article, the authors propose that the two techniques of the posterior-only approaches can lead to improved neurological function and acceptable radiographic results in patients undergoing surgical treatment for spinal tuberculosis. Nevertheless, it was an uncontrolled retrospective study obtained from a small population and relatively short follow-up period.
Conclusions
A transforaminal debridement, interbody fusion with instrumentation may be a viable choice in a relatively healthy young (age <65 years) patients, but postoperative ventilatory support as a complication is too high. The combination of extensive resection and stable reconstruction with interbody autografting via posterior-only approach seems to accelerate neurological recovery in thoracic and thoracolumbar spinal tuberculosis. Patients with poor general medical condition achieve acceptable neurological outcomes and kyphosis correction by shorter operative time and less blood loss through transpedicular decompression with instrumentation techniques.
Acknowledgments
The authors would like to appreciate Assist. Prof. Dr. Sudaporn Sudprasert, for her valuable comments while revising this manuscript. They also thank Dr. Jithayut Sueajui, MD for his considerable assistance with the illustrations.
Notes
Conflict of Interest: No potential conflict of interest relevant to this article was reported.