Two-Level Anterior Cervical Discectomy and Fusion versus Hybrid Total Disc Replacement for Bilevel Pathology with Cervical Radiculopathy/Myelopathy: A Comparative Study with a Minimum 2-Year Follow-up in an Indian Population
Article information
Abstract
Study Design
Retrospective study.
Purpose
To study the outcomes of two-level anterior cervical discectomy and fusion (2L-ACDF) versus hybrid total disc replacement (H-TDR) for cervical myeloradiculopathy.
Overview of Literature
For bilevel disc issues of the cervical spine, 2L-ACDF has been a historical tool with numerous implants used at different time frames. Recent developments in total disc replacement at mobile level with fusion at a spondylotic level known as hybrid fixation have added a new armamentarium for such disorders.
Methods
An analysis of 49 consecutive patients who underwent 2L-ACDF (n=22) and H-TDR (n=27) from January 1, 2014 to December 31, 2017 was performed. Data were studied as retrieved from InstaPACS ver. 4.0 (Mediff Technologies Pvt. Ltd., Bengaluru, India) and medical records.
Results
Twenty-two patients with 2L-ACDF and 27 patients with H-TDR were included. The mean±standard deviation (SD) follow-up duration was 4.0±1.5 years in H-TDR and 3.1±1.1 years in 2L-ACDF. The mean±SD Neck Disability Index (NDI) decreased from 26.1±7.6 to 6.5±3.9 in the H-TDR group and from 27.6±7.2 to 6.4±4.8 in the 2L-ACDF group at final follow-up. Disc height at suprajacent level in the 2L-ACDF group was 4.12±0.48 mm, 4.10±0.45 mm, and 4.05±0.48 mm preoperatively, at 1-year, and final follow-up, respectively. Disc height at supradjacent level in the H-TDR group was 4.28±0.36 mm, 4.20±0.32 mm, and 4.19±0.34 mm preoperatively, at 1-year, and final follow-up, respectively.
Conclusions
There was significantly improved NDI in both groups. Adjacent segment disc height loss was greater in the 2L-ACDF group than in H-TDR but not statistically significant (p=0.304). Supradjacent segment range of motion was greater in the 2L-ACDF group than in the H-TDR group (p=0.003). Both findings supported radiographic adjacent segment degeneration (ASD), but symptomatic ASD was absent in both groups.
Introduction
Anterior cervical discectomy and fusion (ACDF) has long been a gold standard for cervical fusion in spondylotic myeloradiculopathy of the cervical spine [1]. Adjacent segment degeneration (ASD) is a known complication of ACDF. ASD is asymptomatic most of the time, but if ASD becomes symptomatic, it may need revision surgery at the new segment of degeneration [2,3]. To counteract this known complication, the use of total disc replacement (TDR) of the cervical spine became popular. The last 2 decades had multiple studies related to TDR found in the literature with variable results. For bilevel symptomatic cervical disc degenerative disease refractory to adequate conservative treatment, two-level ACDF (2L-ACDF), hybrid total disc replacement (H-TDR), and two-level TDR are the modalities of treatment [4,5]. H-TDR is the optimal treatment for bilevel cervical disc degenerative disease if there are no significant spondylotic changes at one of the degeneration levels. It may be hypothesized that H-TDR might reduce ASD at the adjacent segment by maintaining anatomical conformity and maintaining fusion at more degenerative segments to reduce axial neck pain with adequate decompression of the cord and roots. Biomechanical studies have shown better applicability and acceptable usage of H-TDR for bilevel cervical disc degenerative disease [6,7]. This study compared the clinicoradiological outcomes of H-TDR and 2L-ACDF with a minimum 2-year follow-up for bilevel cervical myeloradiculopathy in an Indian population at a tertiary-level spine center.
Materials and Methods
A retrospective analysis of clinical and radiological data of patients who underwent H-TDR or 2L-ACDF for cervical myeloradiculopathy from January 1, 2014 to December 31, 2017 was performed. Informed consent was obtained. This work did not require an institutional review board approval for a retrospective study. Details on preoperative, operative, and follow-up details of the patients were retrieved from the medical records section. Radiological data were retrieved and reviewed on InstaPACS (picture archiving and communication system) ver. 4.0 (Mediff Technologies Pvt. Ltd., Bengaluru, India). Patient follow-up X-rays in the preoperative, postoperative period and at 3-month, 12-month, and final follow-up were studied (Fig. 1).
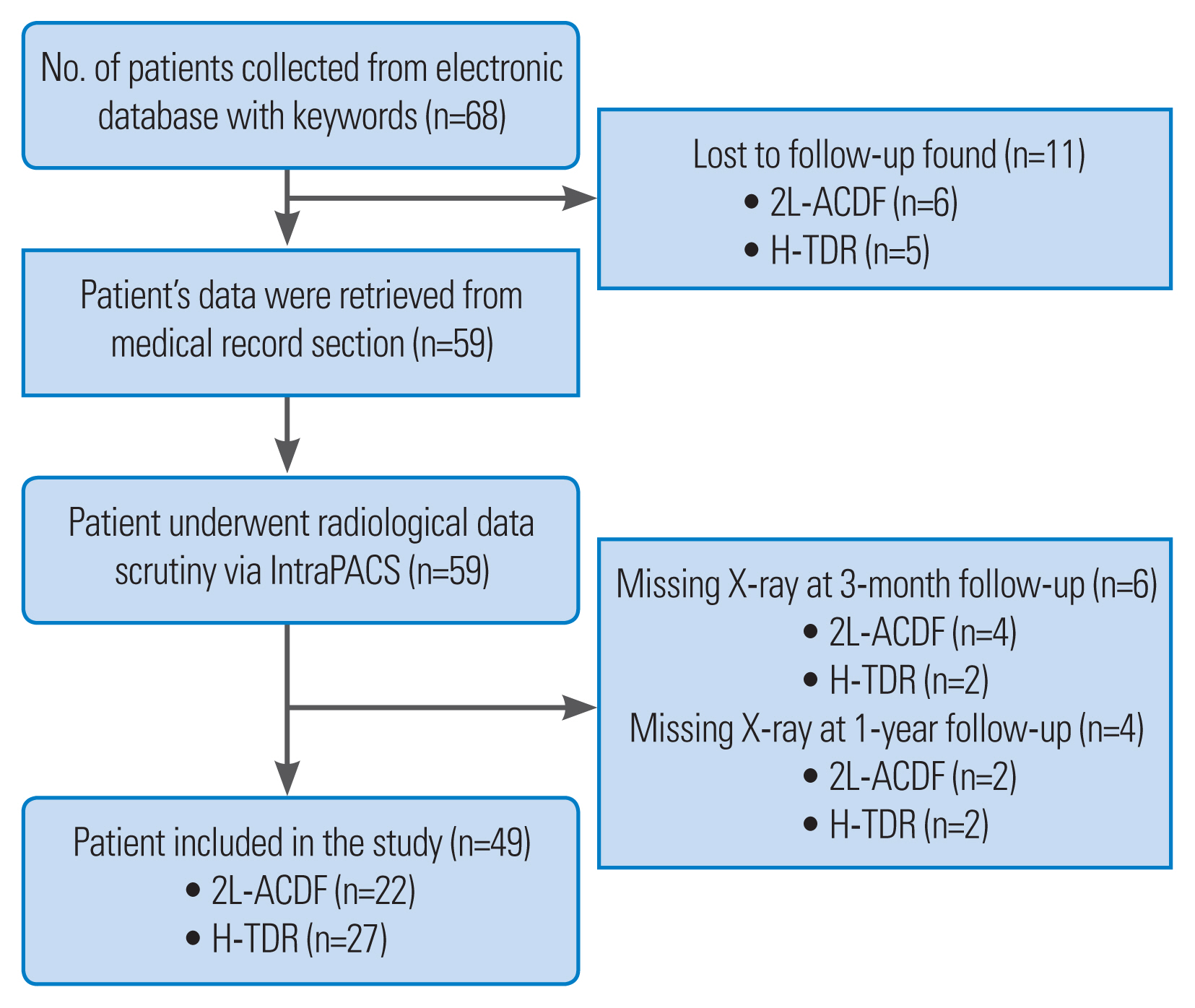
Flowchart depicting inclusion of the patient in the study. 2L-ACDF, two-level anterior cervical discectomy and fusion; H-TDR, hybrid total disc replacement; PACS, picture archiving and communication system.
Surgical details included hospital stay, operative time, blood loss, and any intraoperative or postoperative complication. Clinical details included Visual Analog Scale (VAS) for arm pain, Neck Disability Index (NDI) for neck pain, and the Japanese Orthopaedic Association (JOA) score for myelopathic patients. The radiological assessment included a range of motion (ROM) of prosthesis (difference in the angular measurement between the lower endplate of the upper vertebra and the upper endplate of the lower vertebra in flexion and extension X-rays), ROM of adjacent level (difference in the angular measurement at the supradjacent level), and C2–C7 alignment (Cobb angle between the C2 inferior endplate and the C7 superior endplate on neutral X-ray). Implant subsidence was measured in neutral X-ray. Middle disc height was measured at the TDR level and upper adjacent level to quantify subsidence. All radiological measurements were done using InstaPACS ver. 4.0 (Mediff Technologies Pvt. Ltd.) (Figs. 2, 3).
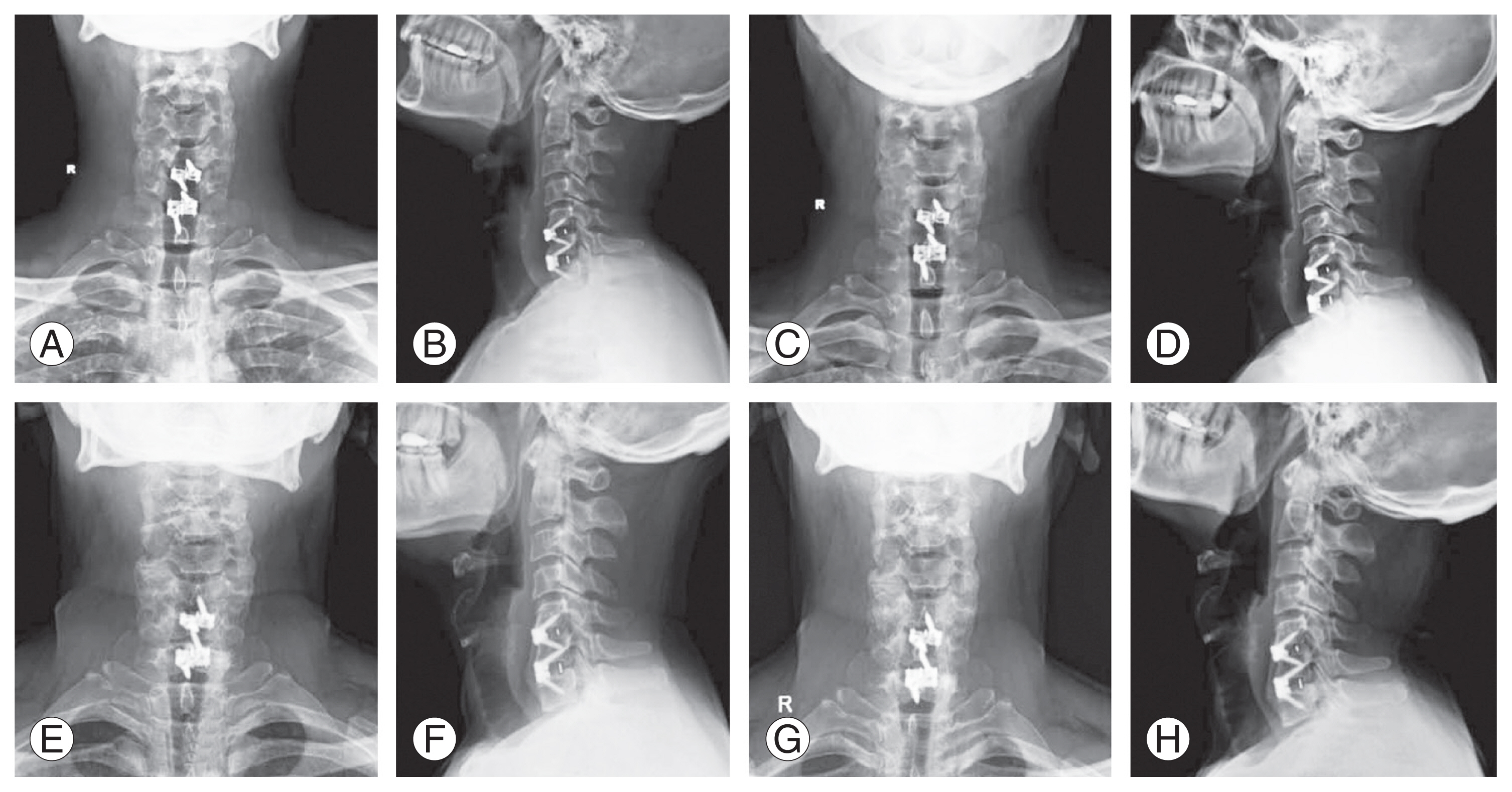
Postoperative X-ray at 6-week (A, AP; B, lateral), 3-month (C, AP; D, lateral), 1-year (E, AP; F, lateral), and final follow-up (G, AP; H, lateral) in patient undergoing two-level anterior cervical discectomy and fusion. AP, anteroposterior.
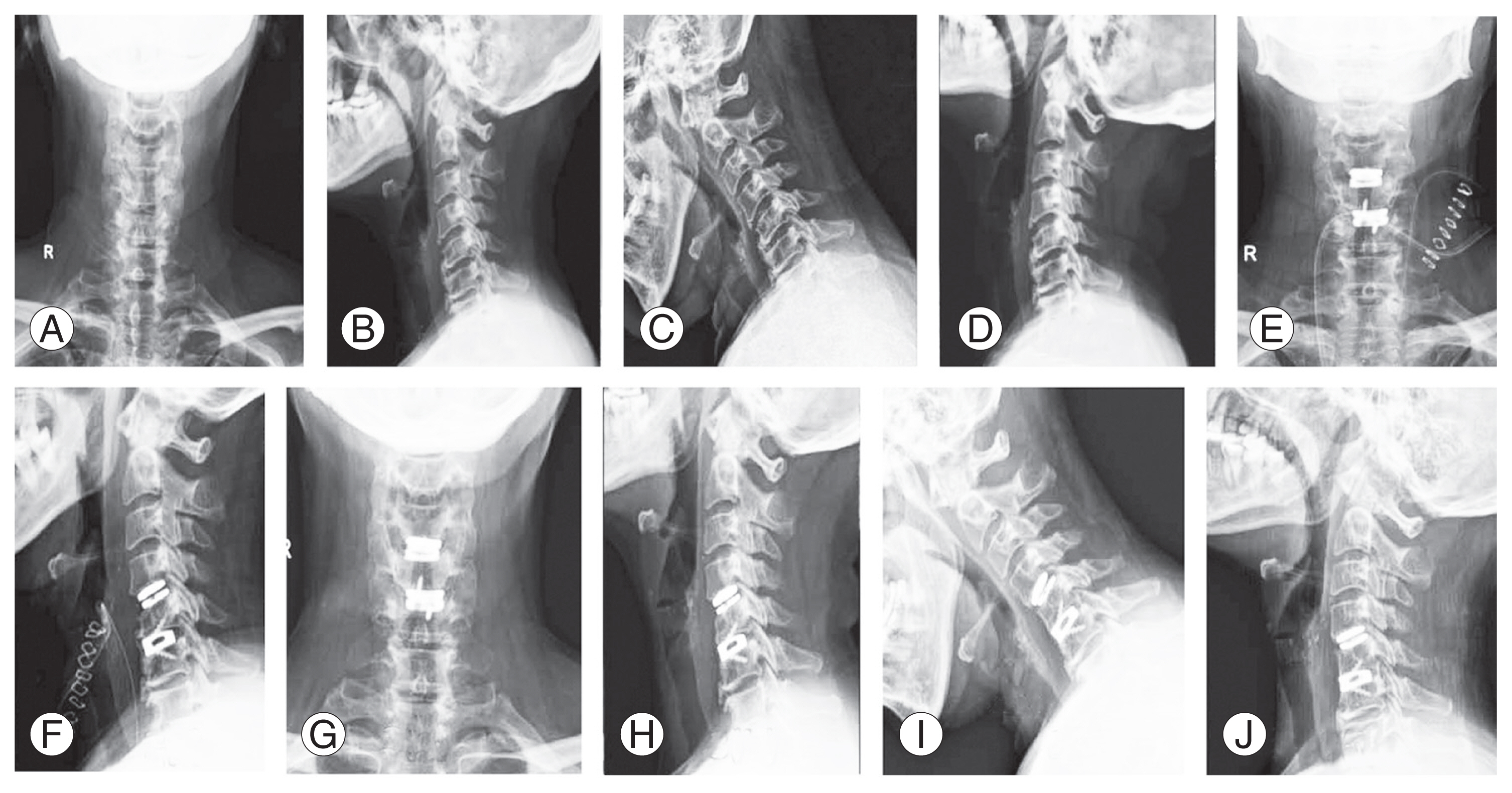
Preoperative X-ray (A, AP; B, lateral; C, lateral flexion; D, lateral extension), immediate postoperative X-ray (E, AP; F, lateral), 3-month follow-up X-ray (G, AP; H, lateral), and 1-year follow-up X-ray (I, lateral flexion; J, lateral extension) in patient undergoing hybrid total disc replacement. AP, anteroposterior.
A computed tomography scan was used to assess heterotopic ossification (HO) in the H-TDR group only at final follow-up. HO was assessed according to the Mehren/Suchomel modification of the McAfee scale for TDR [8] as follows: grade 0, no HO present; grade I, HO is detectable in front of the vertebral body but not in the anatomic interdiscal space; grade II, HO is growing into the disc space with possible affection of the function of the prosthesis; grade III, bridging ossifications still allow movement of the prosthesis; and grade IV, complete fusion of the treated segment without movement in flexion.
1. Surgical details
The patient was placed on the operating table in the supine position with the neck in the neutral position. The patient’s head was secured in place with tape across the forehead to maintain a neutral position, and his/her shoulders are secured down with tape to allow for proper visualization with fluoroscopy. The endplates were examined on lateral fluoroscopy to visualize that they are positioned in a parallel position. The Smith-Robinson approach was used [9]. Excessive exposure was avoided. Distraction pins were placed into the vertebral bodies directly superior and inferior to the disc space. The pins were placed in the midline of the vertebral body on an anteroposterior (AP) view. Discectomy and decompression were then performed at both levels. Once the discectomy was completed, the posterior longitudinal ligament was released to allow for a thorough assessment of the posterior and posterolateral decompression. Care was taken to remove all osteophytes as required. Effort was given to minimize the use of high-speed burr to prevent any bone debris. Abundant irrigation was done, and all bleeding edges were meticulously bone-waxed. Trials were then used to determine the proper implant size in all dimensions (height, width, and depth) and ensure proper alignment with fluoroscopic imaging guidance. The largest possible size implant in the AP and mediolateral planes was chosen. Once the proper implant size was selected, it was placed in the disc space on lateral fluoroscopy and confirmed on AP view. The size of the implant was based on a trial that occupies the maximum width and depth with the posterior border of the trial flush to the posterior vertebral border.
Hybrid surgery consisting of TDR at mobile level and ACDF at spondylotic level was done via a similar approach. Postoperatively, patients were mobilized on the first postoperative day and advised soft cervical collar for 2 weeks. All cases were started on 150 mg indomethacin for 14 days.
At the institute, disc replacement is contraindicated when there is segmental instability, disc height of <3 mm, significant facet joint degeneration/spondylosis, and significant kyphosis or osteoporosis. Therefore, patients with those features underwent fusion instead of disc replacement.
2. Statistical analysis
SAS ver. 9.4 (SAS Institute Inc., Cary, NC, USA) was used for all computations. Results on continuous measurements are presented as mean±standard deviation (SD) and minimum–maximum. Results on categorical measurements are presented as number (%). Significance was assessed at the 5% level. Student t-test (2×1-tailed)/Mann-Whitney test was used to find the significance of parameters on a continuous scale between two groups as per data distribution.
Results
Twenty-two patients with 2L-ACDF and 27 patients with H-TDR were included in the study. The mean±SD follow-up duration was 4.0±1.5 years in the H-TDR group and 3.1±1.1 years in the 2L-ACDF group. The mean±SD age was 43.4±8.8 years for 20 males and seven females in the H-TDR group and 53.3±8.8 years for 14 males and eight females in the 2L-ACDF group. Most of the surgeries were done for radiculopathy, with the most common site being C5–C6 and C6–C7 levels in both groups (Tables 1, 2).
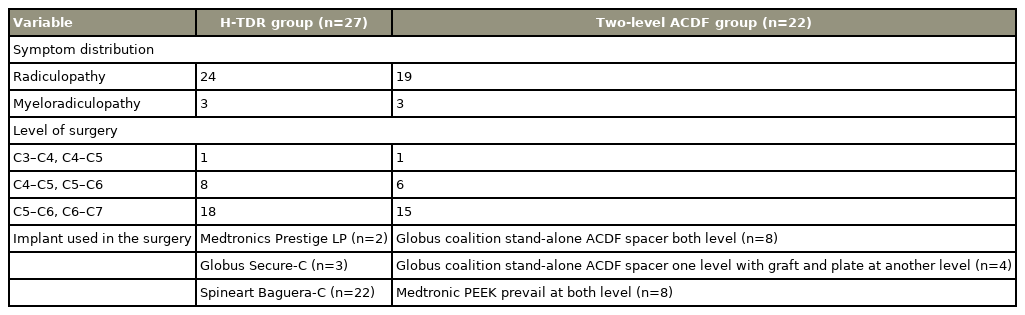
Comparison between the two groups showing symptom distribution, level of surgery, and implant used in the surgery
1. Clinical outcomes
At the time of admission, NDI was 27.63±7.24 in the 2L-ACDF group and 26.07±7.62 in the H-TDR group, which decreased in both groups over time at each follow-up. NDI at final follow-up was 6.36±4.77 in the 2L-ACDF group and 6.51±3.91 in the H-TDR group (Fig. 4A).
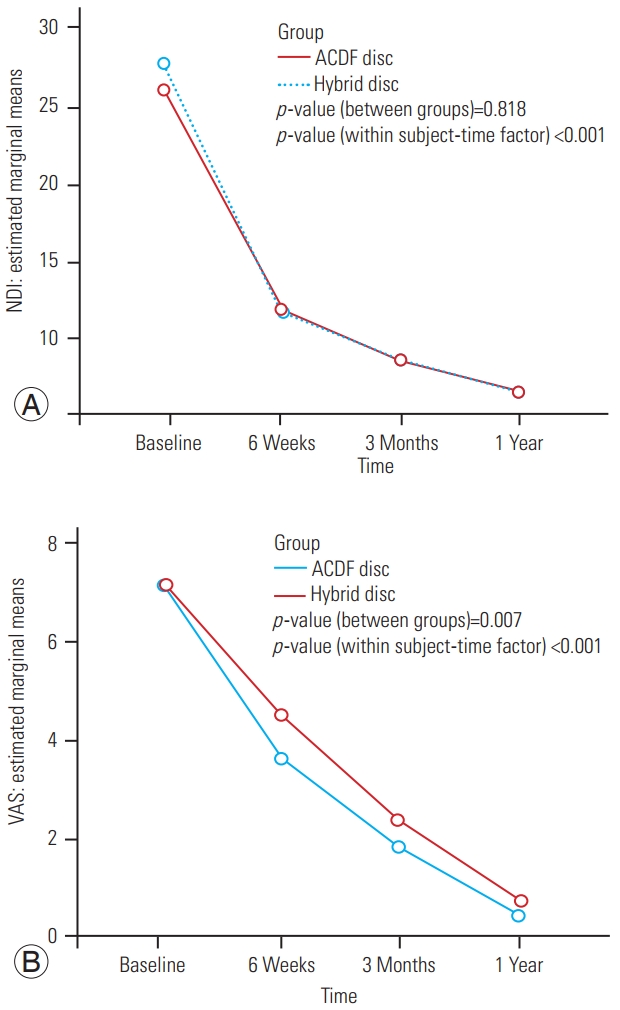
Comparison of (A) Neck Disability Index (NDI) scores and (B) Visual Analog Scale (VAS) scores (arm pain) at various time points between the two groups. ACDF, anterior cervical discectomy and fusion.
Similarly, VAS (arm pain) also decreased over time from 7.18±1.22 (2L-ACDF) and 7.11±1.31 (H-TDR) at the time of admission to 0.18±0.39 (2L-ACDF) and 0.35±0.56 (H-TDR) at final follow-up (Fig. 4B). Mean JOA was calculated in six patients (three in each group), which increased from 13 to 15.5 over time at final follow-up in both groups.
2. Radiological outcomes
Disc height in the 2L-ACDF group was 4.04±0.5 mm, 6.91±0.34 mm, 6.85±0.30 mm, 6.78±0.21 mm, and 6.78±0.21 mm preoperatively and at 6-week, 3-month, 1-year, and final follow-up, respectively. Disc height in the H-TDR group was 4.20±0.35 mm, 6.66±0.33 mm, 6.54±0.32 mm, 6.46±0.30 mm, and 6.47±0.29 mm preoperatively and at 6-week, 3-month, 1-year, and final follow-up, respectively (Fig. 5A). Disc height at suprajacent level in the 2L-ACDF group was 4.12±0.48 mm, 4.11±0.46 mm, 4.15±0.43 mm, 4.10±0.45 mm, and 4.05±0.48 preoperatively and at 6-week, 3-month, 1-year, and final follow-up, respectively. Disc height at supradjacent level in the H-TDR group was 4.28±0.36 mm, 4.28±0.37 mm, 4.16±0.22 mm, 4.20±0.32 mm, and 4.19±0.34 mm preoperatively and at 6-week, 3-month, 1-year, and final follow-up, respectively (Fig. 5B).

Comparison of (A) average disc height of two levels and (B) supradjacent level at various time points between the two groups. ACDF, anterior cervical discectomy and fusion.
ROM of the suprajacent level in both groups with C2–C7 alignment was calculated. In the 2L-ACDF group, it was 9.91°±1.08° preoperatively and increased to 10.76°±1.04° at 1-year and 10.78°±1.03° at final follow-up. In the H-TDR group, it was 9.48°±0.82° preoperatively and increased to 9.55°±0.84° at 1-year and 9.55°±0.84° at final follow-up. The mean±SD (minimum–maximum) ROM of prosthesis was 10.04°±1.07° (8.4°–12.2°) at 3-month follow-up, which was reduced to 8.51°±0.93° (7°–10.4°) at final follow-up in the H-TDR group (Table 3).

Comparison of ROM at supradjacent level and C2–C7 alignment at various time points between the two groups
Both findings on disc height at suprajacent level and ROM of the suprajacent level support radiographic ASD, but symptomatic ASD was absent in both groups. No obvious immediate or final follow-up complications were noted in both groups.
In the H-TDR group, HO was seen in seven patients (25.93%) at final follow-up. There was grade 0 HO in 20 patients (74.07%), grade I HO in two patients (7.4%), grade II HO in two patients (7.4%), grade III HO in two patients (7.4%), and grade IV HO in one patient (3.7%). HO restricting mobility was seen in three patients, grade III HO in two patients (7.4%) and grade IV HO in one patient (3.7%). Hence, at final follow-up, mobility on prosthesis was seen in 88.9% of the patients.
Discussion
In this study, comparing H-TDR (n=27) to 2L-ACDF (n=22), there was a consistent decrease in VAS (arm pain) and NDI from postoperative to final follow-up. There was an improvement in JOA in patients with cervical myelopathy in both groups, although there were only three cases in each group. The mean age was about a decade more in the 2L-ACDF group than in the H-TDR group. Disc height at adjacent level was lesser and ROM of adjacent level was greater at final follow-up in the 2L-ACDF group than in the H-TDR group, although it was not statistically significant. C2–C7 alignment was comparable in both groups.
In a study of Schwab et al. [10], increased motion compensation occurred at segments immediately adjacent to a single-level fusion. Significant differences occurred at the level above the fusion site for the C3–C4 and C4–C5 fusion. When the lower levels (C5–C6 and C6–C7) were fused, a significant amount of increased motion was observed at the levels immediately above and below the fusion [10]. In this study, although the level of surgery was not compared to the amount of motion, there was consistently more motion at supradjacent level in both groups, but it was greater in the 2L-ACDF group than in the H-TDR group. However, there were no cases involving symptomatic ASD in either group during the study period. It is inferred that a small sample size and a short follow-up period are responsible for these results. Despite the absence of symptomatic ASD, increased mobility in the supradjacent segments of both groups may have accelerated degeneration at long-term follow-up. ASD in ACDF cases has been reported in many previous studies [2,3,11,12]. It may remain asymptomatic for years with just a radiological sign of degeneration. These asymptomatic patients have been termed ASD, but if a similar group of patients develops symptoms, they may be classified as adjacent segment disease patients [13]. The adjacent segment disease incidence may range from 2.2% to 25% in patients undergoing ACDF [2,3,14]. Previous studies have shown that TDR decreases the incidence of ASD [15].
After biomechanical studies, H-TDR has shown good results to be used as an appropriate option in bilevel cervical myeloradiculopathy [6,7,16]. In their biomechanical study, Gandhi et al. [6] noted that TDR adjacent to fusion had significantly less increase in motion at all unaltered levels compared to the two-level fusion construct. In another biomechanical study, Liao et al. [16] found that hybrid conditions failed to restore normal motion within the construct, but they significantly normalized motion in adjacent segments. Previous studies on H-TDR have shown similar results to this study on serial decrement in VAS and NDI at different follow-ups [4,17,18]. JOA improved at final follow-up from 9.2 to 13.5 in Ren et al. [18], similar to this study [18].
In this study, the mean±SD ROM of prosthesis in H-TDR at final follow-up was 8.51°±0.93°, with C2–C7 ROM at 54.34°±1.61°. Previous studies on H-TDR have not shown consistent measurements of both C2–C7 ROM and ROM of prosthesis in each study. Few studies have measured C2–C7 ROM, whereas some have ROM of prosthesis measured as a radiological analysis. Barbagallo et al. [4] found functioning disc prosthesis at final follow-up in all cases undergoing H-TDR at a mean (range) follow-up duration of 23.8 (12–40) months. The mean±SD ROM of prosthesis at final follow-up was 7.9°±4.0° [4]. Lee et al. [19] recorded ROM as preserved at the level of arthroplasty at final follow-up, with a mean±SD ROM of 6.7°±2.7°. ROM of the arthroplasty level ranged from 4° to 16° in previous studies, demonstrating lots of variation depending on the prosthesis used [20,21]. Shin et al. [17] found a mean±SD C2–C7 ROM of 54.1°±12.7° at final follow-up, whereas Cardoso and Rosner [22] found a mean±SD C2–C7 ROM of 39.5°±10.04°. Similarly, Lee et al. [19] found a mean±SD C2–C7 ROM of 41.6°±8.1° at final follow-up. There was also nonsignificant subsidence seen with the use of the implant in this study. Similar subsidence was also seen by Fransen and Pointillart [23] in the Baguera prosthesis used in their study, but slightly more in Sharma et al. [24]. Although they did not discuss the reason for this late nonsignificant subsidence, it was perhaps from the sinking of the implant spikes into the endplates over time.
This study found advanced HO in 11.10% of the H-TDR cases and no or grade I and II HO in 88.9% of the cases. Wide variation was seen in HO (7.3%–69.2%) [8,25]. Although advanced stages of HO are associated with reduced prosthesis movement, its clinical significance is yet to be conclusively determined. With longer follow-ups coming, the presence of HO may be a rule rather than an exception in TDR. Its occurrence has been influenced by patient selection, implant, and surgical technique. In a comparative study, Noriega et al. [26] found grade I or no HO in 67% of the cases using Baguera compared to 10.5% with Prodisc C. Advanced HO (grade III or IV) was seen in 18.5% of the cases using Baguera compared to 73.8% using Prodisc and 65% using PCM [26]. Certain factors have been implicated in reducing HO. The placement of the device as posterior as possible to allow the maximum motion of the device, avoiding unnecessary bony exposure, liberal use of bone wax, avoiding the use of drill help prevent the release of bone growth factors [23,24]. Additionally, implants placed without the need for drilling or keel also help in reducing HO incidence due to the reduction of the release of bone growth factors from marrow [23,27]. Previous studies on 2L-ACDF and two-level TDR have shown variable results in outcomes in both groups in different studies. Fay et al. [28] noticed significant improvements in the neck or arm VAS, JOA scores, and NDI in both groups. Davis et al. [29] found that 2L-ACDF patients experienced higher subsequent surgery rates and displayed a higher rate of radiological ASD. Overall, two-level TDR patients maintained segmental ROM for 48 months without device failure. Radcliff et al. [30] found the reoperation rate significantly lower with TDR (4%) versus ACDF (16%). There were no significant differences in the adverse event rates between groups.
The limitation of this study was its small sample size. It was a retrospective study. The follow-up period was also relatively small. The implants and prostheses used were of different types, which may have influenced the results. Despite the limitations, this study might set up a benchmark of applicability of H-TDR in developing countries with good clinicoradiological outcomes.
Conclusions
In conclusion, both H-TDR and 2L-ACDF have comparable and good clinicoradiological outcomes. Significant improvement was seen in VAS (arm) and NDI (p=0.007) in both groups. Adjacent segment disc height loss was greater in the 2L-ACDF group than in the H-TDR group (p=0.009). Supradjacent segment ROM was greater in the 2L-ACDF group than in the H-TDR group but not statistically significant (p=0.304). These findings support radiographic ASD, but symptomatic ASD was absent in both groups. No obvious immediate or final follow-up complications were noted in both groups. H-TDR may be used as an alternative if not a substitute in bilevel cervical myeloradiculopathy with nonspondylotic features at one of the levels planned for surgery.
Notes
Conflict of Interest
No potential conflict of interest relevant to this article was reported.
Author Contributions
Jeevan Kumar Sharma: collection of data, preparation of manuscript; Kalidindi Kalyan Kumar Varma: statistical analysis preparation of final article, discussion; Abhinandan Reddy Mallepally: statistical analysis, referencing; Nandan Marathe: review of literature, referencing; Tarush Rustagi: framing of plan, cross-checking statistics, material and methods; Bibhudendu Mohapatra: guidance, Material and methods writing; Padmini Yadav: review of literature, figure and tables framing; and Kalidutta Das: patron, guidance, discussion framing.
